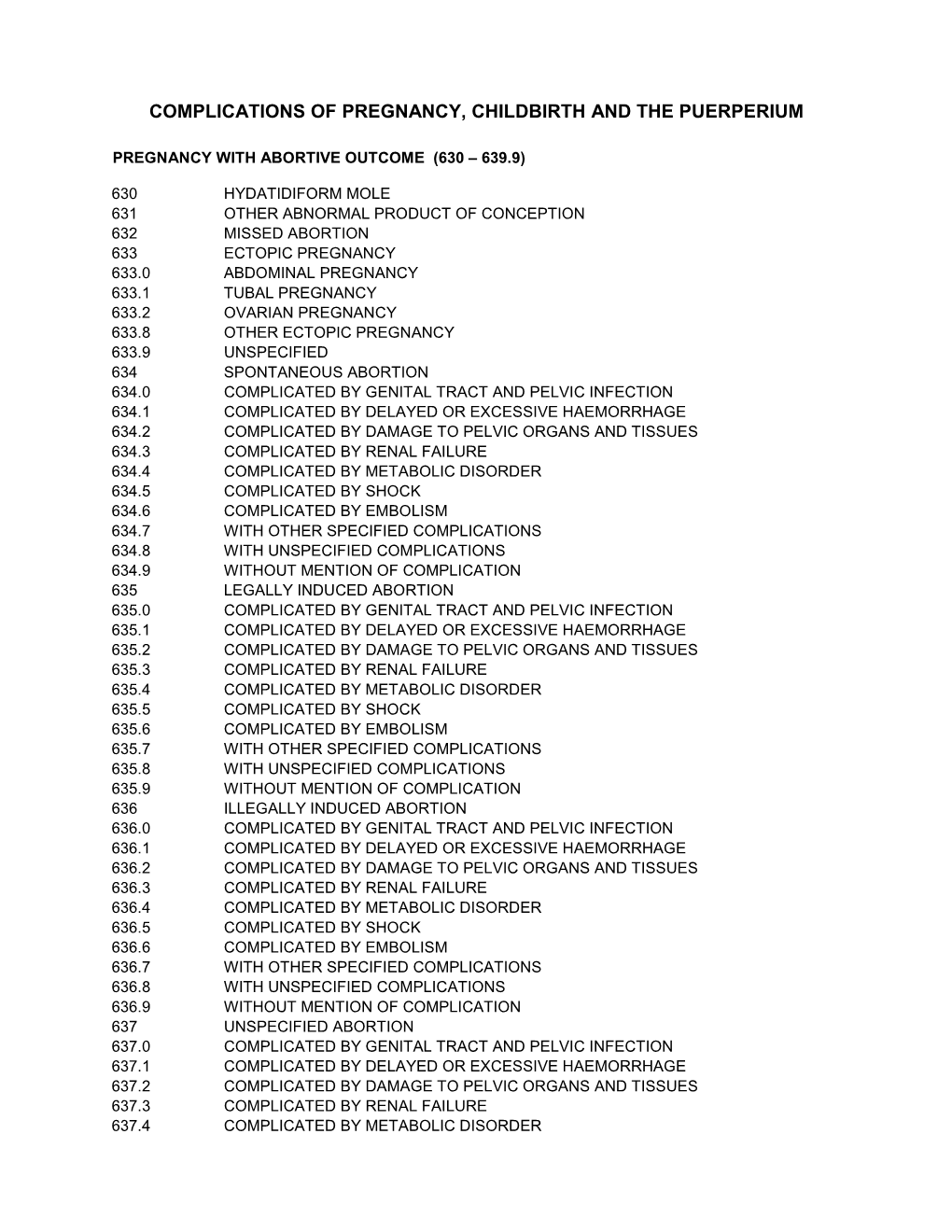
Diagnostic Codes (ICD9) Pregnancy Childbirth Puerperium
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intravenous Drug Use-Associated Infective Endocarditis in Pregnant Patients at a Hospital in West Virginia
Open Access Original Article DOI: 10.7759/cureus.17218 Intravenous Drug Use-Associated Infective Endocarditis in Pregnant Patients at a Hospital in West Virginia Deena Dahshan 1 , Mohamed Suliman 2 , Ebad U. Rahman 3 , Zachary Curtis 1 , Ellen Thompson 2 1. Internal Medicine, Marshall University Joan C. Edwards School of Medicine, Huntington, USA 2. Cardiology, Marshall University Joan C. Edwards School of Medicine, Huntington, USA 3. Internal Medicine, St. Mary's Medical Center, Huntington, USA Corresponding author: Deena Dahshan, [email protected] Abstract Introduction Due to high levels of intravenous drug use (IVDU) in West Virginia (WV), there are increasing numbers of hospitalizations for infective endocarditis (IE). More specifically, pregnant patients with IE are a uniquely challenging population, with complex management and a clinical course that further affects the health of the fetus, with high morbidity and mortality. Timely recognition and awareness of the most common bacterial causes will provide hospitals and clinicians with valuable information to manage future patients. Methods This retrospective study analyzed the clinical course of pregnant patients admitted with IE and IVDU history presenting at Cabell Huntington Hospital from 2013 to 2018. Inclusion criteria were women between 16 and 45 years of age confirmed to be pregnant by urine pregnancy test and ultrasonography with at least eight weeks gestation, with a first-time diagnosis of endocarditis and an identified history of IVDU. We excluded charts with pre-existing risk factors including a history of valvular disease, rheumatic heart disease, surgical valve repair or mechanical valve replacement, or a diagnosis of coagulopathies. The resulting charts were evaluated for isolated organisms, reported clinical course, and complications of the pregnancy. -
Low-Lying Placenta
LOW- LYING PLACENTA LOW-LYING PLACENTA WHAT IS PLACENTA PRAEVIA? The placenta develops along with the baby in the uterus (womb) during pregnancy. It connects the baby with the mother’s blood system and provides the baby with its source of oxygen and nourishment. The placenta is delivered after the baby and is also called the afterbirth. In some women the placenta attaches low in the uterus and may be near, or cover a part, or lie over the cervix (entrance to the womb). If it is shown in early ultrasound scans, it is called a low-lying placenta. In most cases, the placenta moves upwards as the uterus enlarges. For some women the placenta continues to lie in the lower part of the uterus in the last months of pregnancy. This condition is known as placenta praevia. If the placenta covers the cervix, this is known as major placenta praevia. Normal Placenta Placenta Praevia Major Placenta Praevia WHAT ARE THE RISKS TO MY BABY AND ME? When the placenta is in the lower part of the womb, there is a risk that you may bleed in the second half of pregnancy. Bleeding from placenta praevia can be heavy, and so put the life of the mother and baby at risk. However, deaths from placenta praevia are rare. You are more likely to need a caesarean section because the placenta is in the way of your baby being born. HOW IS PLACENTA PRAEVIA DIAGNOSED? A low-lying placenta may be suspected during the routine 20-week ultrasound scan. Most women who have a low-lying placenta at the routine 20-week scan will not go on to have a low-lying placenta later in the pregnancy – only 1 in 10 go on to have a placenta praevia. -

Terminology for Describing Normally-Sited and Ectopic Pregnancies on Ultrasound: ESHRE Recommendations for Good Practice
Terminology for describing normally-sited and ectopic pregnancies on ultrasound: ESHRE recommendations for good practice Set-up The invitation to review was sent to the members of the SIG Implantation and early pregnancy (n=7443 email addresses). In addition, the invitation was mailed to the members of the ESHRE Executive Committee and the Committee of National Representatives (n=74). An announcement was also placed on the eshre.eu website. The stakeholder review started on 20th of April 2020, and was closed after 4 weeks, on the 18th of May 2020. Summary Thirty reviewers, representing nineteen countries, submitted a total of 212 comments (on average 7 comments per reviewer). All reviewers are listed on page 2. IMPACT OF THE COMMENTS 9% General comment or language correction 25% Comments resulting in a change Comments to which a reply 66% was formulated This report comprises the list of reviewers, and the overview of comments, with a reply from the working group. Page 1 of 40 List of reviewers Name Country Organization Masoud Kamrava Iran Steven Goldstein USA Ulrike Metzger France Grigorios Derdelis Greece Luca Savelli Italy Gangaraju Buvaneswari India Mridu Sinha India Onur Erol Turkey Aboubakr Mohamed Elnashar Egypt Jiuzhi Zeng China Carlos Calhaz-Jorge Portugal Dr. Nidaa Qatar Attilio Di Spiezio Sardo Italy Melinda Mitranovici Romania Ali Sami Gurbuz Turkey Philippe Merviel France Roy Farquharson UK Ilan Timor USA Alessandra Pipan United Arab Emirates Company, Taiwan IVF Wen Jui Yang Taiwan Group Center Lorenzo Abad de Velasco Spain Monica Varma India Kumaran Aswathy India Annick Geril Belgium Snezana Vidakovic Serbia Lukasz Polanski, Miriam Baumgarten, Rebecca McKay, Laura Rutherford, Ouma Pillay, Anita Jeyaraj, Kanna Jayaprakasan and Kamal Ojha UK organization Mohamed Shahin UK Mohsen M El-Sayed UK International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) ISUOG European Niche taskforce group of the ESGE and international Prof. -

Sonography in First Trimester Bleeding
Review Sonography in First Trimester Bleeding Manjiri Dighe, MD,1 Carlos Cuevas, MD,1 Mariam Moshiri, MD,1 Theodore Dubinsky, MD,1 Vikram S. Dogra, MD2 1 Department of Radiology, University of Washington Medical Center, Seattle, WA 98195 2 Department of Imaging Sciences, University of Rochester School of Medicine, 601 Elmwood Avenue, Box 648, Rochester, NY 14642 Received 19 April 2007; accepted 1 October 2007 ABSTRACT: Vaginal bleeding is the most common however, the most common cause of bleeding is cause of presentation to the emergency department spotting caused by implantation of the conceptus in the first trimester. Approximately half of patients into the endometrium. A complete assessment of with first trimester vaginal bleeding will lose the preg- the first trimester pregnancy requires correlation nancy. Clinical assessment is difficult, and sonogra- of serum b human chorionic gonadotropin (b- phy is necessary to determine if a normal fetus is hCG) levels with the appearance of the gesta- present and alive and to exclude other causes of bleeding (eg, ectopic or molar pregnancy). Diagnosis tional sac (GS) using sonography. of a normal intrauterine pregnancy not only helps the physician in terms of management but also gives psy- SPONTANEOUS ABORTION chologic relief to the patient. Improved ultrasound technology and high-frequency endovaginal trans- Spontaneous abortion is defined as the termina- ducers have enabled early diagnosis of abnormal and tion of a pregnancy before the twentieth completed ectopic pregnancies, decreasing maternal morbidity week of gestation. Sixty-five percent of spontane- and mortality. The main differential considerations of ous abortions occur in the first 16 weeks of preg- first trimester bleeding are spontaneous abortion, ec- nancy. -

Diseases of the Digestive System (KOO-K93)
CHAPTER XI Diseases of the digestive system (KOO-K93) Diseases of oral cavity, salivary glands and jaws (KOO-K14) lijell Diseases of pulp and periapical tissues 1m Dentofacial anomalies [including malocclusion] Excludes: hemifacial atrophy or hypertrophy (Q67.4) K07 .0 Major anomalies of jaw size Hyperplasia, hypoplasia: • mandibular • maxillary Macrognathism (mandibular)(maxillary) Micrognathism (mandibular)( maxillary) Excludes: acromegaly (E22.0) Robin's syndrome (087.07) K07 .1 Anomalies of jaw-cranial base relationship Asymmetry of jaw Prognathism (mandibular)( maxillary) Retrognathism (mandibular)(maxillary) K07.2 Anomalies of dental arch relationship Cross bite (anterior)(posterior) Dis to-occlusion Mesio-occlusion Midline deviation of dental arch Openbite (anterior )(posterior) Overbite (excessive): • deep • horizontal • vertical Overjet Posterior lingual occlusion of mandibular teeth 289 ICO-N A K07.3 Anomalies of tooth position Crowding Diastema Displacement of tooth or teeth Rotation Spacing, abnormal Transposition Impacted or embedded teeth with abnormal position of such teeth or adjacent teeth K07.4 Malocclusion, unspecified K07.5 Dentofacial functional abnormalities Abnormal jaw closure Malocclusion due to: • abnormal swallowing • mouth breathing • tongue, lip or finger habits K07.6 Temporomandibular joint disorders Costen's complex or syndrome Derangement of temporomandibular joint Snapping jaw Temporomandibular joint-pain-dysfunction syndrome Excludes: current temporomandibular joint: • dislocation (S03.0) • strain (S03.4) K07.8 Other dentofacial anomalies K07.9 Dentofacial anomaly, unspecified 1m Stomatitis and related lesions K12.0 Recurrent oral aphthae Aphthous stomatitis (major)(minor) Bednar's aphthae Periadenitis mucosa necrotica recurrens Recurrent aphthous ulcer Stomatitis herpetiformis 290 DISEASES OF THE DIGESTIVE SYSTEM Diseases of oesophagus, stomach and duodenum (K20-K31) Ill Oesophagitis Abscess of oesophagus Oesophagitis: • NOS • chemical • peptic Use additional external cause code (Chapter XX), if desired, to identify cause. -

Antepartum Haemorrhage
OBSTETRICS AND GYNAECOLOGY CLINICAL PRACTICE GUIDELINE Antepartum haemorrhage Scope (Staff): WNHS Obstetrics and Gynaecology Directorate staff Scope (Area): Obstetrics and Gynaecology Directorate clinical areas at KEMH, OPH and home visiting (e.g. Community Midwifery Program) This document should be read in conjunction with this Disclaimer Contents Initial management: MFAU APH QRG ................................................. 2 Subsequent management of APH: QRG ............................................. 5 Management of an APH ........................................................................ 7 Key points ............................................................................................................... 7 Background information .......................................................................................... 7 Causes of APH ....................................................................................................... 7 Defining the severity of an APH .............................................................................. 8 Initial assessment ................................................................................................... 8 Emergency management ........................................................................................ 9 Maternal well-being ................................................................................................. 9 History taking ....................................................................................................... -

Recode - Guidelines for Use the System Is Hierarchical I.E
ReCoDe - Guidelines for use The system is hierarchical i.e. categories at the head of the list take priority over those lower down. However multiple relevant conditions can be recorded. The primary condition is the highest on the list that is applicable to the case. Secondary condition is the next relevant condition down the list e.g. for codes B2, F3, and A7 - the primary code is A7, secondary code is B2 etc. ReCoDe - version 2.0 Group Condition further definition inclusion/exclusion A Fetus A1 Lethal congenital anomaly Lethal or severe. Any structural, genetic, or metabolic defect arising at conception or during embryogenesis incompatible with life or potentially treatable but causing death. A2 Infection Positive fetal microbiologic or serological culture. 2.1 Chronic – e.g. TORCH E.g. congenital or intrauterine pneumonia, cytomegalovirus, 2.2 Acute rubella, herpes. A3 Non-immune hydrops fetalis Presence of any two of the following signs: Ascites pericardial effusion pleural effusion subcutaneous oedema. A4 Iso-immunisation Blood group incompatibility rhesus or non rhesus (ABO). Death ascribable to blood group incompatibility. An indirect Coomb test greater than 1/16 and fetal hydrops (see A3). A5 Fetomaternal haemorrhage Haemorrhage into maternal circulation Kleihauer-Betke test > 0.4%1. A6 Twin-twin transfusion Presence of polyhydramnios (maximum vertical pocket of ≥ 8 cm) and oligohydramnios (maximum vertical pocket of ≤ 2 cm)2. A7 Fetal growth restriction SGA by customised percentile, intrauterine growth retardation. < 10th customised weight for gestational age centile3 OR IUGR reported on clinical or pathological grounds. A8 Other fetus Death due to other specific fetal conditions e.g. -

State Medicaid Manual
Page 1 of 37 Louisiana Medicaid Approved Pay and Chase Primary Prenatal Care Diagnosis Codes MCOs must use the "pay and chase" method of payment for prenatal services for individuals with other Health Insurance. The MCO must seek reimbursement from the third party within 60 days after the end of the month in which payment is made. Primary prenatal diagnoses which do not require primary health insurance claim filing by most providers are confined to those listed below. Hospitals are not included and must continue to file claims with the primary health insurance carriers. ICD-9-CM to ICD-10 crosswalk for Prenatal Diagnosis Codes ICD-9-CM Description Code V22.0 Supervision of normal pregnancy V22.1 V23 Supervision of high risk pregnancy V28 Antenatal screening 640-648 Complications related to pregnancy 651-658 Other conditions requiring care in 671 pregnancy 673 675-676 ICD-10-CM Diagnosis Codes – for Prenatal Services upon Implementation of ICD-10 ICD-9-CM code V22.0 maps to the following ICD-10-CM codes Z3400 Encounter for supervision of normal first pregnancy, unspecified trimester Z3403 Encounter for supervision of normal first pregnancy, third trimester Z3401 Encounter for supervision of normal first pregnancy, first trimester Z3402 Encounter for supervision of normal first pregnancy, second trimester ICD-9-CM code V22. -

Umbilical Cord Accidents
UMBILICAL CORD ACCIDENTS DR PADMASRI R PROF & HOD, DEPT OF OBSTETRICS & GYNAECOLOGY SAPTHAGIRI INSTITUTE OF MEDICAL SCIENCES 1 • “Cord accident,” defined by obstruction of fetal blood flow through the umbilical cord, is a common ante- or perinatal occurrence. • Obstruction can be either acute, as in cases of cord prolapse during delivery, or sub acute to-chronic, as in cases of grossly abnormal umbilical cords Placental findings in cord accidents. Mana M Parast From Stillbirth Summit 2011, Minneapolis, USA 2 TYPES Acute events Sub Acute on Chronic • Umbilical Cord Prolapse • Loops • Knots • Vasa Praevia • Entanglements • Coiling • Torsion • Rupture • Haematomas, thrombosis • Cysts, tumours • Nuchal Cord • Insertion - velamentous cord CORD COMPRESSION – SUDDEN IUD’s 3 CORD COMPRESSION 2 Principles of asphyxia are: a. Cord compression -preventing venous return to the fetus b. Umbilical vasospasm -preventing venous and arterial blood flow to and from the fetus due to exposure to external environment. 4 Recovery time from compression • 1min, 1 time 100% compression – 5 mins to recover- oxygen levels decrease by 50% • 5 mins comp – 30 mins to recover • Continued 5 min compressions every 30 mins causes fetal decompensation RISK FACTORS FOR CORD PROLAPSE GENERAL PROCEDURE RELATED Artificial rupture of membranes with high Multiparity presenting part Vaginal manipulation of the fetus with ruptured Low birthweight (< 2.5 kg) membranes Preterm labour (< 37+0 External cephalic version (during procedure) weeks) Fetal congenital anomalies Internal podalic version Breech presentation Stabilising induction of labour Transverse, oblique and Insertion of intrauterine pressure transducer unstable lie* Second twin Large balloon catheter induction of labour Polyhydramnios Unengaged presenting part Low-lying placenta RCOG Green-top Guideline No. -

Perinatal Arterial Ischemic Stroke: an Unusual Causal Mechanism
ical C lin as C e f R o l e Russo et al., J Clin Case Rep 2014, 4:8 a p n o r r u t DOI: 10.4172/2165-7920.1000401 s o J Journal of Clinical Case Reports ISSN: 2165-7920 Case Report Open Access Perinatal Arterial Ischemic Stroke: An Unusual Causal Mechanism Francesca Maria Russo1*, Giuseppe Paterlini2 and Patrizia Vergani1 1Department of Obstetrics and Gynecology, University of Milano-Bicocca, Monza, Italy 2Department of Pediatrics and Neonatal Intensive Care Unit, University of Milano-Bicocca, Monza, Italy Abstract Perinatal Arterial Ischemic Stroke (AIS) is an important cause of neurological morbidity in infants. Some risk factors have been identified, but its pathogenesis remains unclear. We present a case of perinatal in which macroscopic examination of the placenta revealed the presence of a vasa praevia. We hypothesize that compression of the vasa praevia during labor could have determined the formation of thrombi, which were subsequently embolized into the fetal circulation causing perinatal AIS. Background increased flow in the districts of the sylvian artery. No cardiac anatomic or functional abnormalities were found. Coagulation studies were Perinatal arterial ischemic stroke (AIS) is estimated to occur in the normal range and disorders of the coagulation pathway were in 1/1600 to 1/5000 births [1]. Even if rare, it is an important cause excluded. Thrombophilias were excluded both in the baby and in the of mortality and morbidity in neonates. A meta-analysis showed mother. that 57% of infants who suffer perinatal AIS develop motor and/or cognitive deficits, and 3% die [2]. -

The Identification and Validation of Neural Tube Defects in the General Practice Research Database
THE IDENTIFICATION AND VALIDATION OF NEURAL TUBE DEFECTS IN THE GENERAL PRACTICE RESEARCH DATABASE Scott T. Devine A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the School of Public Health (Epidemiology). Chapel Hill 2007 Approved by Advisor: Suzanne West Reader: Elizabeth Andrews Reader: Patricia Tennis Reader: John Thorp Reader: Andrew Olshan © 2007 Scott T Devine ALL RIGHTS RESERVED - ii- ABSTRACT Scott T. Devine The Identification And Validation Of Neural Tube Defects In The General Practice Research Database (Under the direction of Dr. Suzanne West) Background: Our objectives were to develop an algorithm for the identification of pregnancies in the General Practice Research Database (GPRD) that could be used to study birth outcomes and pregnancy and to determine if the GPRD could be used to identify cases of neural tube defects (NTDs). Methods: We constructed a pregnancy identification algorithm to identify pregnancies in 15 to 45 year old women between January 1, 1987 and September 14, 2004. The algorithm was evaluated for accuracy through a series of alternate analyses and reviews of electronic records. We then created electronic case definitions of anencephaly, encephalocele, meningocele and spina bifida and used them to identify potential NTD cases. We validated cases by querying general practitioners (GPs) via questionnaire. Results: We analyzed 98,922,326 records from 980,474 individuals and identified 255,400 women who had a total of 374,878 pregnancies. There were 271,613 full-term live births, 2,106 pre- or post-term births, 1,191 multi-fetus deliveries, 55,614 spontaneous abortions or miscarriages, 43,264 elective terminations, 7 stillbirths in combination with a live birth, and 1,083 stillbirths or fetal deaths. -

Board-Review-Series-Obstetrics-Gynecology-Pearls.Pdf
ObstetricsandGynecology BOARDREVIEW Third Edition Stephen G. Somkuti, MD, PhD Associate Professor Department of Obstetrics and Gynecology and Reproductive Sciences Temple University School of Medicine School Philadelphia, Pennsylvania Director, The Toll Center for Reproductive Sciences Division of Reproductive Endocrinology Department of Obstetrics and Gynecology Abington Memorial Hospital Abington Reproductive Medicine Abington, Pennsylvania New York Chicago San Francisco Lisbon London Madrid Mexico City Milan New Delhi San Juan Seoul Singapore Sydney Toronto Copyright © 2008 by the McGraw-Hill Companies, Inc. All rights reserved. Manufactured in the United States of America. Except as permitted under the United States Copyright Act of 1976, no part of this publication may be reproduced or distributed in any form or by any means, or stored in a database or retrieval system, without the prior written permission of the publisher. 0-07-164298-6 The material in this eBook also appears in the print version of this title: 0-07-149703-X. All trademarks are trademarks of their respective owners. Rather than put a trademark symbol after every occurrence of a trademarked name, we use names in an editorial fashion only, and to the benefit of the trademark owner, with no intention of infringement of the trademark. Where such designations appear in this book, they have been printed with initial caps. McGraw-Hill eBooks are available at special quantity discounts to use as premiums and sales promotions, or for use in corporate training programs. For more information, please contact George Hoare, Special Sales, at [email protected] or (212) 904-4069. TERMS OF USE This is a copyrighted work and The McGraw-Hill Companies, Inc.