Neonatal Isoerythrolysis Neonatal Isoerythrolysis Pathogenesis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Occurrence, Hematologic and Serum Biochemical Characteristics of Neonatal Isoerythrolysis in Arabian Horses of Iran
Archive of SID Original Paper DOI: 10.22067/veterinary.v1-2i10-11.71821 Received: 2018-Mar-27 Accepted after revision: 2018-Aug-07 Published online: 2018-Sep-26 Occurrence, hematologic and serum biochemical characteristics of neonatal isoerythrolysis in Arabian horses of Iran a a a Seyedeh Missagh Jalali, Mohammad Razi-Jalali, Alireza Ghadrdan-Mashhadi, b Maryam Motamed-Zargar a Department of Clinical Sciences, Faculty of Veterinary Medicine, Shahid Chamran University of Ahvaz, Ahvaz, Iran b Graduated student of Veterinary Medicine, Faculty of Veterinary Medicine, Shahid Chamran University of Ahvaz, Ahvaz, Iran Keywords assessment, the foal with hemolytic anemia showed neonatal isoerythrolysis, hemolytic anemia, Arabian horses, a major decline in hematocrit, hemoglobin concen- Khouzestan tration and erythrocyte count along with considerable leukocytosis and neutrophilia. Serum total and direct Abstract bilirubin concentrations in the NI case was about ten times higher than in the rest of the foals. This study Neonatal isoerythrolysis is a major cause of ane- revealed that neonatal isoerythrolysis can occur in Arabian mia in newborn foals. However, there are no docu- foals of Khouzestan and is associated with severe anemia mented data regarding the occurrence of neonatal and icterus which may lead to death. These findings can be isoerythrolysis in Arabian horses of Iran, which are beneficial in the establishment of preventive measures in mostly raised in Khouzestan province. Hence, this Arabian horse breeding industry in the region, as well as study was carried out to investigate the occurrence of improving therapeutic methods. neonatal isoerythrolysis in Arabian horses of Khou- zestan and assess the hematologic and serum bio- chemical profile of affected foals. -

Dr* Robert Hillman Cares for a Newborn with Assistance from Judy Chapman
Dr* Robert Hillman cares for a newborn with assistance from Judy Chapman. DO YOU HAVE A 'PREEMIE1? The perinatal period for the equine has been defined as the period from Day 300 of gestation, generally considered to be the lowest By Pamela Livesay-Wilkins '86 limit of viability, to 96 hours post-partum, "ith Special Thanks to Dr. Diane Craig when the foal is considered to have reached a steady state of body functions, recovering from the stresses of birth. Events in the fetus and in the mother need to be closely coordinated so There are times when the mother and the that the mother will give birth to a full-term, ^ tus are prepared for birth at different stages mature foal that is capable of survival outside ?f gestation. When it happens that the mother the uterus. However, there are a variety of ls ready first, the foal may be born premature. conditions that can occur and indicate that the Approximately 1% of all Thoroughbreds are mother and fetus were not equally prepared for “orn prematurely, and the incidence approaches birth. Most forms of prematurity have a this value in most other breeds, so it isn't common cause with abortion and the distinction surprising that most active horse breeders have between them is rather arbitrary, based t° deal with the problem of a premature foal at primarily on the prospect for fetal survival and some point. In the last decade the value of gestational age of the fetus. Chronic placental horses, particularly Thoroughbreds, has insufficiency due to twinning, body pregnancy Increased tremendously, reflected by an (pregnancy located in the body of the uterus increased interest on the part of both the rather than in one of the uterine horns), veterinarian and the client in neonatal critical umbilical cord abnormalities, hydrops of the care and management techniques. -

D:\My Documents\Vet Alumnus
For Private Circulation Only Vol. XXXVIII (No. 2) December, 2016 Vet Alumnus Vol. XXXVII (No. 2) December, 2016 1 ISSN 2319-5762 Editor: Dr. Amarjit Singh Associate Editor: Dr. Jaswinder Singh Vet Alumnus Vol. XXXVII (No. 2) December, 2016 2 CONTENTS 1. SOME ANATOMICAL DIFFERENCES IN STIFLE 1 JOINT OF BUFFALO AND CATTLE VARINDER UPPAL, NEELAM BANSAL, ANURADHA GUPTA AND OPINDER SINGH 2. BUSINESS OPPORTUNITIES FOR VETERINARIANS IN INDIA 5 MK GUPTA AND HK VERMA 3. CLASSICAL SWINE FEVER-DREADLY DISEASE IN PIGS 11 V. MAHAJAN, G. FILIA, M. S. BAL AND AMARJIT SINGH 4. CRYSTALLOID PLUS COLLOID BASED FLUID THERAPY 14 FOR DYSTOCIA AFFECTED BUFFALO SARVPREET SINGH GHUMAN 5. HOW TO PREPARE YOUR DOG FOR A DOG SHOW 16 KIRTI DUA 6. ULTRASONOGRAPHY: A ROBUST TOOL TO IDENTIFY 21 SUB-FERTILITY IN BREEDING BULLS KHUSHPREET SINGH, AJEET KUMAR AND BILAWAL SINGH 7. LAMENESS IN YOUNG DOGS 24 VANDANA SANGWAN AND YASEEN MOHD SHEIKH JANI 8. PHYSICAL OCCUPATIONAL HEALTH HAZARDS IN VETERINARY 27 PRACTICE AND THEIR MANAGEMENT RAJESH KASRIJA AND SIMRANPREET KAUR 9. POLICY AND STRATEGY FOR GENETIC IMPROVEMENT OF 32 DAIRY ANIMALS IN PUNJAB SIMARJEET KAUR, P.K. SINGH* AND P.S. BRAR 10. A BRIEF INTRODUCTION ON BLOOD GROUPS IN EQUINES 41 AND NEONATAL ISOERYTHEOLYSIS. RABYIAJAVED, PH.D SCHOLAR Note : Authors are sole responsible for the contents given in articles Vet Alumnus Vol. XXXVII (No. 2) December, 2016 3 SOME ANATOMICAL DIFFERENCES IN STIFLE JOINT OF BUFFALO AND CATTLE VARINDER UPPAL, NEELAM BANSAL, ANURADHA GUPTA AND OPINDER SINGH Department of Anatomy, GADVASU, Ludhiana The stifle joint is the largest and most complex and modified hinge joint. -

Proposal for Crossmatch Project 18.10.12.Docx
Aus der Klinik für kleine Haustiere des Fachbereichs Veterinärmedizin der Freien Universität Berlin Studies in feline pre-transfusion testing: Evaluating a novel blood typing device and serial cross-matching in transfusion patients Inauguraldissertation zur Erlangung des Grades eines Doktors der Veterinärmedizin an der Freien Universität Berlin Vorgelegt von Layla Hourani Tierärztin aus Rostock Berlin 2017 Journal-Nr.: 3990 Gedruckt mit Genehmigung des Fachbereichs Veterinä rmedizin der Freien Universitä t Berlin Dekan: Univ.-Prof. Dr. Jürgen Zentek Erster Gutachter: Univ.-Prof. Dr. Barbara Kohn Zweiter Gutachter: Univ.-Prof. Dr. Heidrun Gehlen Dritter Gutachter: Univ.-Prof. Dr. Robert Klopfleisch Deskriptoren (nach CAB-Thesaurus): blood type, blood typing, cat, cross-matching, pre- transfusion testing, point-of-care, transfusion medicine, transfusion safety Tag der Promotion: 19.07.2017 2 To Friedolin, Krikri, Molly, Spotty and the old gibbon couple at Sababurg Zoo 3 Table of contents LIST OF ABBREVIATIONS.....................................................................................................................6 TABLES AND FIGURES .........................................................................................................................7 1 INTRODUCTION ...........................................................................................................................8 1.1 HISTORY OF TRANSFUSION MEDICINE AND TRANSFUSION SAFETY .......................................................9 1.2 PATIENT SAFETY IN -
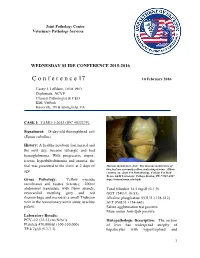
C O N F E R E N C E 17 10 February 2016
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2015-2016 C o n f e r e n c e 17 10 February 2016 Casey J. LeBlanc, DVM, PhD Diplomate, ACVP Clinical Pathologist & CEO KDL VetPath Knoxville, TN & Springfield, VA CASE I: TAMU-1-2013 (JPC 4033379). Signalment: 18-day-old thoroughbred colt (Equus caballus) History: A healthy newborn foal nursed and the next day, became lethargic and had hemoglobinuria. With progressive stupor, icterus, hyperbilirubinemia and anemia, the foal was presented to the clinic at 2 days of Mucous membranes, foal. The mucous membranes of this foal are extremely yellow, indicating icterus. (Photo age. courtesy of: Dept Vet Pathobiology, College Vet Med Texas A&M University, College Station, TX 77843-4467 Gross Pathology: Yellow mucous http://vetmed.tamu.edu/vtpb) membranes and tissues (icterus); ~200ml abdominal transudate with fibrin strands; Total bilirubin 14.5 mg/dl (0-1.9) myocardial mottling grey and red GGT 124U/L (0-53) (hemorrhage and necrosis) a small Thebsian Alkaline phosphatase 553U/L (128-512) vein in the noncoronary aortic sinus; urachus ALT 850U/L (134-643) patent. Saline agglutination test positive Mare serum Anti-Qab positive Laboratory Results: PCV=12 (32-53) no Nrbc’s Histopathologic Description: The section Platelets 470,000/ul (100-350,000) of liver has widespread atrophy of TP 4.7g/dl (5.3-7.3) hepatocytes with hypertrophied and 1 Liver, foal. There is extensive pigment deposition throughout the section, to include brown granules in hepatocytes (lipofuscin- yellow arrows), brown spicular material (acid hematin – green arrows) and distended bile canaliculi (cholestasis – black arrows). -

Prevalence of Ca Blood Type and Alloantibodies in a Population of Horses from Italy
animals Article Prevalence of Ca Blood Type and Alloantibodies in a Population of Horses from Italy Daniela Proverbio 1,* , Roberta Perego 1,* , Luciana Baggiani 1, Francesco Ferrucci 2, Enrica Zucca 2 , Federico Nobile 3 and Eva Spada 1 1 Veterinary Transfusion Research Laboratory (REVLab), Department of Veterinary Medicine (DIMEVET), University of Milan, via dell’Università 6, 26900 Lodi, Italy; [email protected] (L.B.); [email protected] (E.S.) 2 Department of Health, Animal Science and Food Safety (VESPA), University of Milan, via dell’Università 6, 26900 Lodi, Italy; [email protected] (F.F.); [email protected] (E.Z.) 3 Veterinary pratictioner, Via Budrio 44, 20153 Milan, Italy; [email protected] * Correspondence: [email protected] (D.P.); [email protected] (R.P.); Tel.: +39-3482266335 (D.P.); +39-3388658384 (R.P.) Received: 5 May 2020; Accepted: 10 July 2020; Published: 13 July 2020 Simple Summary: Indications for whole blood transfusion in equine critical care include severe anemia from surgical blood loss or acute hemorrhage, hemolysis and neonatal isoerythrolysis. In horses, as in other animals, transfusions are associated with a number of inherent risks such as transfusion reactions. Pretransfusion screening and blood typing are indicated to minimize the risk of incompatible red cell transfusions. Equine blood types include seven systems, namely A, C, D, K, P, Q, and U. The major RBC antigens that warrant identification before packed RBC or whole blood transfusions in horses are Ca and Aa. The frequencies of blood groups can vary from one population to another and from one breed to another. -

Hemolytic Disease of the Newborn 33
Hemolytic Disease 16 of the Newborn Blood Type A or Q negative red cells in mare A or Q positive fetus A or Q negative red cells in mare now sensitized to red cells of foal Anti-A or Q antibody secreted in colostrum and absorbed by foal. Antibodies destroy red cells of foal. 32 Quick Look: Hematology emolytic disease of the newborn, also known as present in high titer in all type B cats so prior pregnancy Hneonatal isoerythrolysis (NI), and in humans as or transfusion is not required for antibodies to form, and erythroblastosis fetalis or Rh disease, is another cause of hemolysis may occur in the first pregnancy. The anti-B alloimmune hemolysis. Maternal antibodies form when antibody present in Type A cats is not strong enough to the mother is sensitized to foreign antigens on the red cause this problem. cells of her fetus. These red cells have been inherited In cattle, use of vaccines (e.g., anaplasmosis) con- from the sire (Figure). taining blood products has resulted in cows becoming sensitized. If the bull has the same red cell antigens as Pathogenesis the vaccine donor, then the calf may share these antigens Human mothers may become sensitized to certain anti- and develop hemolysis. In dogs, transfusion of DEA 1.1– gens, most commonly Rh through exposure to fetal red positive blood can sensitize negative bitches and be a cells during pregnancy or at parturition. Sensitization cause of hemolysis should she be bred to a positive male. could also occur from a prior transfusion. If fetal red cells In horses, one can detect sensitization of the mare by in subsequent pregnancies contain these antigens, mater- performing a Coombs’ test (see Chapter 14) on the sire’s nal antibody may pass through the placenta and cause red cells mixed with the serum of the mare either before hemolysis before birth of the fetus. -

Red Blood Cell Surface Antigens Responsible for Neonatal Isoerythrolysis in Thoroughbred Horses of Jeju Island
J Vet Clin 29(6) : 431-434 (2012) Red Blood Cell Surface Antigens Responsible for Neonatal Isoerythrolysis in Thoroughbred Horses of Jeju Island Jung-Whan Song, Young-min Yun, Gui-cheol Choi*, Yong-duk Lee*, Ji-hoon Jeong* and Kyoung-kap Lee1 College of Veterinary Medicine, Jeju National University, Jeju 690-756, Korea *Jeju Studfarm, Korea Racing Authority, Jeju 695-961, Korea (Accepted: December 03, 2012) Abstract : This study was conducted to survey red blood cell (RBC) antigens Aa, Ca and Qa types, which are considered to be the most significantly associated with occurrence of neonatal isoerythrolysis, and the results are expected to provide valuable informations in organization of breeding plan, hence preventing the disease. Blood samples were collected from 262 Thoroughbred horses in Jeju island. Two percent cell suspension has been prepared from each sample and they were tested by indirect antiglobulin test. Of the 226 mare's samples, 9(3.98%) were Aa negative, 8(3.54%) were Ca negative, 17(7.52%) were Qa negative. Of the 36 Stallion's samples, 1(2.78%) was Aa negative, 3(8.33%) were Ca negative, 3(8.33%) were Qa negative. On the basis of these data, a database for breeding compatability could be set, and it would play an important role as a reference for arranging the mating partners. Key words : Neonatal isoerythrolysis, Aa Ca Qa antigens, Indirect anti-globulin test, Thoroughbred. Introduction Interestingly, it has been reported that mares lacking the Aa and Ca groups will spontaneously develop Ca antibody (1). Neonatal isoerythrolysis (NI) or hemolytic anemia of the NI reportedly has a prevalence of 1% in Thoroughbred newborn, although not commonly encountered in equine horses and a 2% prevalence in Standardbred horses. -

Horse Genetics, 2Nd Edition
Horse Genetics, 2nd Edition Horse Genetics, 2nd Edition Ernest Bailey M.H. Gluck Equine Research Center University of Kentucky Lexington, Kentucky, USA and Samantha A. Brooks Department of Animal Science Cornell University Ithaca, New York, USA CABI is a trading name of CAB International CABI CABI Nosworthy Way 38 Chauncey Street Wallingford Suite 1002 Oxfordshire OX10 8DE Boston, MA 02111 UK USA Tel: +44 (0)1491 832111 Tel: +1 800 552 3083 (toll free) Fax: +44 (0)1491 833508 Tel: +1 (0)617 395 4051 E-mail: [email protected] E-mail: [email protected] Website: www.cabi.org © E. Bailey and S.A. Brooks 2013. All rights reserved. No part of this publication may be reproduced in any form or by any means, electronically, mechanically, by photocopying, recording or otherwise, without the prior permission of the copyright owners. A catalogue record for this book is available from the British Library, London, UK. Library of Congress Cataloging-in-Publication Data Bailey, Ernest (Ernest Frank) Horse genetics / Ernest Bailey, University of Kentucky, M.H. Gluck Equine Research Center, Lexington, KY, USA, and Samantha A. Brooks, Cornell University, Department of Animal Science, Ithaca, NY, USA. -- 2nd edition. pages cm Previous edition by Ann T. Bowling. Includes bibliographical references and index. ISBN 978-1-84593-675-4 (pbk. : alk. paper) -- ISBN 978-1-78064-329-8 (hardback : alk. paper) 1. Horses--Breeding. 2. Horses--Genetics. I. Brooks, Samantha A., 1979- II. Bowling, Ann T. Horse genetics. III. Title. SF291.B63 2013 636.1'0821--dc23 2012049905 ISBN-13: 978 1 84593 675 4 (pbk) 978 1 78064 329 8 (hbk) Commissioning editor: Sarah Hulbert Editorial assistant: Alexandra Lainsbury Production editor: Lauren Povey Typeset by SPi, Pondicherry, India. -

Occurrence, Hematologic and Serum Biochemical Characteristics of Neonatal Isoerythrolysis in Arabian Horses of Iran
Original Paper DOI: 10.22067/veterinary.v1-2i10-11.71821 Received: 2018-Mar-27 Accepted after revision: 2018-Aug-07 Published online: 2018-Sep-26 Occurrence, hematologic and serum biochemical characteristics of neonatal isoerythrolysis in Arabian horses of Iran a a a Seyedeh Missagh Jalali, Mohammad Razi-Jalali, Alireza Ghadrdan-Mashhadi, b Maryam Motamed-Zargar a Department of Clinical Sciences, Faculty of Veterinary Medicine, Shahid Chamran University of Ahvaz, Ahvaz, Iran b Graduated student of Veterinary Medicine, Faculty of Veterinary Medicine, Shahid Chamran University of Ahvaz, Ahvaz, Iran Keywords assessment, the foal with hemolytic anemia showed neonatal isoerythrolysis, hemolytic anemia, Arabian horses, a major decline in hematocrit, hemoglobin concen- Khouzestan tration and erythrocyte count along with considerable leukocytosis and neutrophilia. Serum total and direct Abstract bilirubin concentrations in the NI case was about ten times higher than in the rest of the foals. This study Neonatal isoerythrolysis is a major cause of ane- revealed that neonatal isoerythrolysis can occur in Arabian mia in newborn foals. However, there are no docu- foals of Khouzestan and is associated with severe anemia mented data regarding the occurrence of neonatal and icterus which may lead to death. These findings can be isoerythrolysis in Arabian horses of Iran, which are beneficial in the establishment of preventive measures in mostly raised in Khouzestan province. Hence, this Arabian horse breeding industry in the region, as well as study was carried out to investigate the occurrence of improving therapeutic methods. neonatal isoerythrolysis in Arabian horses of Khou- zestan and assess the hematologic and serum bio- chemical profile of affected foals. -

Certificate of Analysis for Lot P091005-001
Telephone: 509-334-5815 Fax: 509-332-5356 VMRD E-mail: [email protected] PO Box 502, Pullman, WA 99163 USA Web site: http://www.vmrd.com Certificate of Analysis EQUINE COOMBS REAGENT CATALOG NO.: 492-2 VOLUME: 2 ml LOT: P091005-001 EXPIRATION DATE: 22 February 2014 INTRODUCTION: The equine Coombs test, also called direct antiglobulin test, is designed to detect immune-mediated erythrocyte destruction which occurs in autoimmune hemolytic anemia, and in some cases with infections and neoplastic disorders, in neonatal isoerythrolysis. Hemolysis in these diseases is caused by the erythrocytes being coated with antibody (IgG, IgM) and/or complement components (C3). Coated erythrocytes are lysed in the bloodstream and/or removed by phagocytes. The Coombs reagent is an antiserum to equine IgG, IgM, and C3 prepared in goats. After obtaining the antiserum, complement is inactivated at 56C for 30 minutes and then the antiserum is absorbed repeatedly with washed normal equine erythrocytes. These treatments ensure that the Coombs reagent will not react with normal equine erythrocytes. However, equine erythrocytes that are coated with IgG, IgM, and/or C3 will be agglutinated by the Coombs reagent because it contains antibodies to equine IgG, IgM, and C3. QUALITY CONTROL METHOD: Washed sheep red blood cells (SRBC) were sensitized with the Equine Coombs Positive Control (catalog no. 472-2). The procedure is performed according to the Coombs Positive Control Procedure. The Equine Coombs Reagent was tested according to the Equine Coombs Reagent Procedure. Specific Reaction: The Coombs reagent produced agglutination on sensitized SRBCs of 1+ agglutination at 1/2, 1-2+ at 1/4 and +/- agglutination at 1/8. -

Neonatal Isoerythrolysis
Neonatal Isoerythrolysis Jon Palmer, VMD, New Bolton Center, University of Pennsylvania Neonatal Isoerythrolysis (NI) is an immune mediated hemolytic anemia of new born foals mediated by maternal anti-RBC antibodies absorbed from colostrum. Conditions necessary for NI to occur 1) The foal must inherit certain RBC antigens from the sire that the dam does not have. 2) The dam has to be previously sensitized to these RBC antigens through: a. Placental bleeding from fetal membranes to maternal blood during previous pregnancies with same RBC antigens in foal’s blood (most mares at risk are multiparous) b. Previous whole blood transfusion c. Equine biologics or plasma contaminated with RBC antigens 3) During the current pregnancy the mare is re-exposed, mounts an antibody response and concentrates the antibodies in her colostrum. 4) The foal must ingest and absorb the colostrum in sufficient quantities to cause disease. The most common of the 32 blood group antigens in the horse to be involved is the Aa and the Qa locus which is thought to account for 90% of the reactions. The R and S groups are 3rd and 4th most common. The frequency of the genes for these antigens and thus the frequency that they are the culprits vary among breeds. Both agglutination and hemolysis may occur depending on the antibodies present in the colostrum. Both intravascular and extravascular hemolysis may occur. Jon Palmer, VMD New Bolton Center Frequency of Antigens and Risk of Antibody Production in Different Breeds % of mares without Likelihood foal has Breed Antigen antigen (at risk) inherited antigen Thoroughbred Aa 2% 85% Qa 16% 60% Standardbred Pacers Aa 22% 44% Trotters Aa 3% 82% All Std Qa 0% Saddlebred Aa 25% 50% Qa 68% 12% Quarter Horse Aa 25% 49% Qa 68% 18% Morgan Aa 18% 57% Qa 0% Arabian Aa 3% 82% Qa 72% 20% from: Bailey, E.