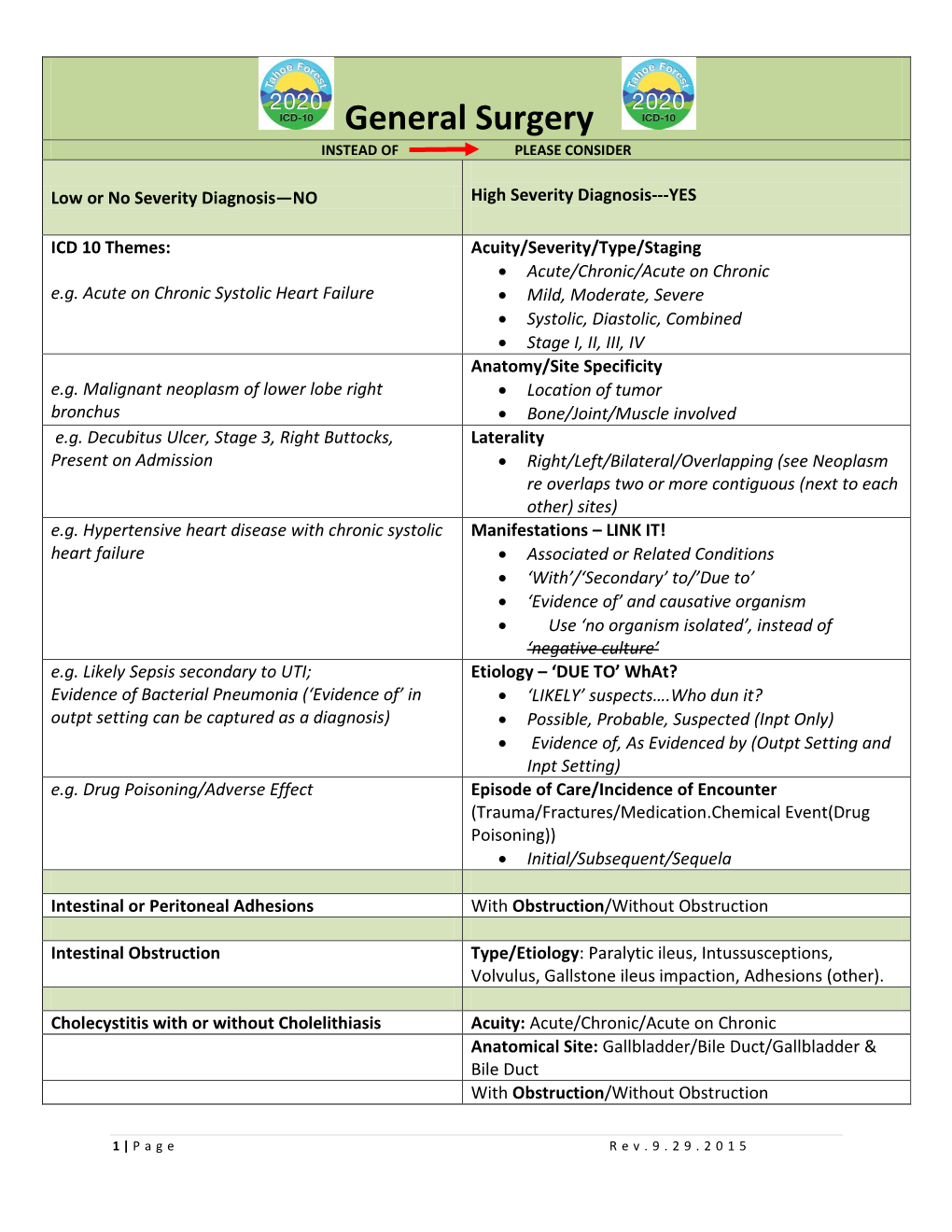
General Surgery INSTEAD of PLEASE CONSIDER
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gallstone Ileus As an Unexpected Complication of Cholelithiasis: Diagnostic Difficulties and Treatment
Turkish Journal of Trauma & Emergency Surgery Ulus Travma Acil Cerrahi Derg 2010;16 (4):344-348 Original Article Klinik Çalışma Gallstone ileus as an unexpected complication of cholelithiasis: diagnostic difficulties and treatment Kolelitiazisin beklenmedik komplikasyonu, safra taşı ileusu: Tanı zorlukları ve tedavi Savaş YAKAN,1 Ömer ENGİN,1 Tahsin TEKELİ,1 Bülent ÇALIK,2 Ali Galip DENEÇLİ,1 Ahmet ÇOKER,3 Mustafa HARMAN4 BACKGROUND AMAÇ Gallstone ileus is a rare complication of cholelithiasis, Safra taşı ileusu safra taşı hastalığının nadir ve genelde mostly in the elderly. The aim of this study was to evaluate yaşlılarda görülen bir komplikasyonudur. Çalışmamızın our experience with 12 gallstone ileus cases and discuss amacı safra taşı ileusu tanısı alan 12 hastayla ilgili dene- current opinion as reported in the literature. yimimizi değerlendirmek ve güncel literatür eşliğinde tar- tışmaktır. METHODS Data of 12 patients operated between January 1998 and GEREÇ VE YÖNTEM January 2008 with gallstone ileus were retrospectively Kliniğimizde Ocak 1998-2008 yılları arasında safra taşı ile- studied. usu nedeniyle ameliyat edilen 12 olgunun dosyaları retros- pektif olarak incelendi. RESULTS There were 12 cases (9 F, 75%; 3 M, 25%) with a mean age BULGULAR of 63.6 (50-80) years. Median duration of symptoms before Hastaların 9’u (%75) kadın, 3’ü (%25) erkek olup orta- admission to the hospital was 4.1 (1-15) days. Preoperative lama yaş 63,6 idi (dağılım, 50-80). Semptomların başla- diagnosis was made in only five cases (41.6%). Enteroli- masından hastaneye başvurmaya kadar geçen süre ortala- thotomy was done in nine cases (75%). Enterolithotomy and ma 4,1 (dağılım, 1-15) gün bulundu. -

A 'Wandering' Gallstone
SAJS Case Report A ‘wandering’ gallstone M Kuehnast, MB ChB, DA (SA) T Sewchuran, MB ChB S Andronikou, MB BCh, FCRad (SA), FRCR (Lond), PhD, Visiting Professor Department of Diagnostic Radiology, Faculty of Health Sciences, University of the Witwatersrand, and Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg When all three of the features of Rigler’s triad are present on an abdominal radiograph, the cause of a small-bowel obstruction can be identified. S Afr J Surg 2012;50(3):104-105. DOI:10.7196/SAJS.1339 Case report A 71-year-old man presented with possible gastric outlet obstruction. Previously treated for ulcerative colitis, he had had a colectomy and had undergone Park’s procedure (construction of an ileal-anal pouch). At presentation, the patient’s main complaint was a 4-day history of abdominal pain and vomiting. He was dehydrated, with associated metabolic alkalosis. He also had a history of acute-on- chronic renal failure, diabetes and hypertension. On admission, plain abdominal radiographs (Figs 1 and 2) demonstrated signs of small-bowel obstruction, multiple radio- opaque stones (including one large one) in the region of the right hypochondrium, and intrabiliary gas. The patient therefore represented a classic case of Rigler’s triad, indicating ‘gallstone ileus’. An ultrasound scan of the abdomen confirmed the pneumobilia and multiple small stones in the gallbladder. Also there was no Fig. 1. A supine abdominal radiograph demonstrating multiple, radio-opaque intra- or extrahepatic bile duct dilation, and there were no signs of stones in the right hypochondrium. (Some of these stones may be located in cholecystitis. -

General Surgery
Fast Forward Top 50 Codes General2014 Surgery ICD-9-CM Code ICD-10-CM Code(s) ICD-9-CM Code ICD-10-CM Code(s) 550.90 Inguinal hernia, without K40.90 Unilateral inguinal 789.00 Abdominal pain, unspecfied mention of obstruction hernia, without or gangrene, unilateral or obstruction or ICD-10-CM R10.0 Acute abdomen unspecified (not specified as gangrene, not Codes R10.10 Upper abdominal pain, unspecified recurrent) specified as recurrent R10.11 Right upper quadrant pain 278.01 Morbid obesity R10.12 Left upper quadrant pain R10.13 Epigastric pain ICD-10-CM E66.01 Morbid (severe) obesity due to excess calories R10.2 Pelvic and perineal pain Codes ** Code first obesity complicating pregnancy, childbirth and the R10.30 Lower abdominal pain, unspecified puerperium, if applicable (O99.21-) R10.31 Right lower quadrant pain Use additional code to identify body mass index (BMI), if known R10.32 Left lower quadrant pain (Z68-) R10.33 Periumbilical pain 574.20 Calculus of gallbladder without K80.20 Calculus of gallbladder R10.84 Generalized abdominal pain mention of cholecystitis, with- without cholecystitis R10.9 Unspecified abdominal pain out mention of obstruction without obstruction 553.3 Diaphragmatic hernia 211.3 Benign neoplasm of colon ICD-10-CM K44.9 Diaphragmatic hernia without obstruction or gangrene ICD-10-CM D12.0 Benign neoplasm of cecum Codes K44.0 Diaphragmatic hernia with obstruction, without gangrene Codes D12.1 Benign neoplasm of appendix K44.1 Diaphragmatic hernia with gangrene D12.2 Benign neoplasm of ascending colon Q79.0 Congenital -

Stone Ileus: an Unusual Presentation of Crohn's Disease
Ma, et al. Int J Surg Res Pract 2016, 3:046 International Journal of Volume 3 | Issue 2 ISSN: 2378-3397 Surgery Research and Practice Case Report: Open Access Stone Ileus: An Unusual Presentation of Crohn’s Disease Charles Ma and H Tracy Davido Department of Critical Care and Acute Care Surgery, University of Minnesota Health, USA *Corresponding author: H Tracy Davido MD, Assistant Professor of Surgery, Department of Critical Care and Acute Care Surgery, University of Minnesota Health, 11-115A Phillips Wangensteen Building, 420 Delaware St. SE, MMC 195, Minneapolis, MN 55455, USA, Tel: 612-626-6441, E-mail: [email protected] Introduction Case Report Stone ileus, also known as enterolith ileus enterolithiaisis, is a rare A 67-year-old morbidly obese woman came to the emergency complication of cholelithiasis and an even rarer symptom of Crohn’s department at our institution with an upper respiratory infection, disease. Gallstone ileus is secondary to fistula formation between decreased appetite, and malaise. Her past medical history was the gallbladder and the gastrointestinal (GI) system. Enterolithiasis significant for an open cholecystectomy more than 30 years earlier. of Crohn’s disease is thought to arise from the stasis of succus She had no additional past surgical history or diagnoses. The initial within the small bowel eventually leading to stone formation and workup revealed acute renal failure, with significant electrolyte growth. Both gallstone ileus and enterolithiasis of Crohn’s disease abnormalities and dehydration. She underwent intravenous fluid can result in subsequent mechanical bowel obstruction. Gallstone resuscitation and electrolyte replacement in the Medical Intensive ileus accounts for 1% to 4% of mechanical bowel obstructions, with Care Unit; however, while hospitalized, she developed new-onset higher a incidence in women over age 60 [1]. -

ICD-10 Diagnostic Codes for the Discharge Diagnoses for the Cohort of Patients Included in This Study
ICD-10 diagnostic codes for the discharge diagnoses for the cohort of patients included in this study ICD-10 code and diagnosis Gastrointestinal ulcers K25.1 Gastric ulcer, acute with perforation K25.2 Gastric ulcer, acute with both haemorrhage and perforation K25.5 Gastric ulcer, chronic or unspecified with perforation K25.6 Gastric ulcer, chronic or unspecified with both haemorrhage and perforation K26.1 Duodenal ulcer, acute with perforation K26.2 Duodenal ulcer, acute with both haemorrhage and perforation K26.5 Duodenal ulcer, chronic or unspecified with perforation K26.6 Duodenal ulcer, chronic or unspecified with both haemorrhage and perforation K27.1 Peptic ulcer, acute with perforation K27.2 Peptic ulcer, acute with both haemorrhage and perforation K27.5 Peptic ulcer, chronic or unspecified with perforation K27.6 Peptic ulcer, chronic or unspecified with both haemorrhage and perforation K28.0 Gastrojejunal ulcer, acute with haemorrhage K28.1 Gastrojejunal ulcer, acute with perforation K28.2 Gastrojejunal ulcer, acute with both haemorrhage and perforation K28.3 Gastrojejunal ulcer, acute without haemorrhage or perforation K28.5 Gastrojejunal ulcer, chronic or unspecified with perforation K28.6 Gastrojejunal ulcer, chronic or unspecified with both haemorrhage and perforation K28.7 Gastrojejunal ulcer, chronic without haemorrhage or perforation K28.9 Gastrojejunal ulcer, unspecified without haemorrhage or perforation Hernias K40.0 Bilateral inguinal hernia with obstruction without gangrene K40.1 Bilateral inguinal hernia, with gangrene -

Gallstone Ileus After Cholecystectomy Johnny Cheng, D.O.1, Meghan Timmerman, D.O.1, Jennifer Cheng, OMS III.2, Henrique Fernandez, M.D
Gallstone ileus after cholecystectomy Johnny Cheng, D.O.1, Meghan Timmerman, D.O.1, Jennifer Cheng, OMS III.2, Henrique Fernandez, M.D. FACP3. 1Parkview Medical Center Internal Medicine Residency program, Pueblo, Colorado 2Rocky Vista University College of Osteopathic Medicine, Parker, Colorado 3Parkview Medical Center Director of Gastroenterology Fellowship program, Pueblo, Colorado Gallstone ileus is an uncommon cause of mechanical bowel obstruction caused by a biliary-enteric fistula. This infrequent cause of small bowel obstruction is usually compounded by multiple medical conditions that generally requires a complex surgery. In the population of patients over 65 years old, 25% of non-strangulated small bowel obstructions are caused by gallstone ileus. Due to the delayed diagnosis, mortality is high nearing one in five cases. In this case report, we address if prophylactic cholecystectomy would prevent gallstone ileus. An 83-year-old female with unknown past medical history presented to a rural emergency room with abdominal pain for the past three days. She had associated nausea and vomiting with localized pain to the right upper quadrant. There was no hematochezia, melena, or hematemesis. A CT of the abdomen revealed evidence of a large stone in the duodenum, ileus, air in the gallbladder fossa and no visualization of the gallbladder. Subsequently, she was transferred to another facility for higher level of care with admission to the intensive care unit (ICU). Vitals upon admission to the ICU reveal blood pressure 70/26, heart rate 103, respiratory rate 22, oxygen saturation of 93% on room air, temperature 98.1 Fahrenheit. Labs: WBC 10.0, Hgb 14.7, Hct 45.0, Plt 388, Sodium 133, Potassium 4.5, Chloride 98, Carbon Dioxide 17, BUN 43, Creatinine 2.20, Glucose 148, Calcium 10.2, Total bilirubin 0.9, AST 36, ALT 32, Alkaline Phosphatase 165, Total protein 7.1, Albumin 4.0, Lipase 381. -

Cholecystocolonic Fistula: Facts and Myths. a Review of the 231
J Hepatobiliary Pancreat Surg (2009) 16:8–18 DOI 10.1007/s00534-008-0014-1 REVIEW ARTICLE Cholecystocolonic fistula: facts and myths. A review of the 231 published cases Renato Costi Æ Bruto Randone Æ Vincenzo Violi Æ Olivier Scatton Æ Leopoldo Sarli Æ Olivier Soubrane Æ Bertrand Dousset Æ Thierry Montariol Received: 19 March 2008 / Accepted: 28 April 2008 / Published online: 17 December 2008 Ó Springer 2008 Abstract Resolution of colonic biliary ileus by interventional Background Cholecystocolonic fistula (CCF) is the sec- endoscopy is reported. ond most common cholecystoenteric fistula and is often Conclusion CCF should be considered in differential discovered intraoperatively, resulting in a challenging sit- diagnosis of diarrhea, especially in old, female patients. A uation for the surgeon, who is forced to switch to a possible second hepatobiliary abnormality should be complex procedure, often in old, unfit patients. Manage- always investigated. Extemporaneous frozen section ment of this uncommon but possible finding is still ill should be performed if gallbladder cancer is suspected. defined. Depending on clinical presentation, different treatments for Methods An extensive review of 160 articles published CCF are indicated, ranging from minimally invasive pro- from 1950 to 2006 concerning 231 cases of CCF was cedures to extensive resection. performed. Results CCF is mostly an affliction of women in their Keywords Cholecystocolonic fistula Á Biliary ileus Á sixth to seventh decades and is rarely diagnosed preoper- Diagnosis Á Treatment Á Laparoscopy atively. Chronic diarrhea is the key symptom in nonemergency patients, but, in one-fourth of cases, CCF presents with an acute onset, mostly biliary ileus. -

Cholecystoduodenal Fistula and Gallstone Ileus: a Case Report
Journal of Surgery: Open Access SciO p Forschene n HUB for Sc i e n t i f i c R e s e a r c h ISSN 2470-0991 | Open Access CASE REPORT Volume 5 - Issue 4 Cholecystoduodenal Fistula and Gallstone Ileus: A Case Report Célia Garritano1,*, Bruna Lago Chaves2, Aline Machado Teixeira Auad2, Peter França Lins de Carvalho2, Thaís de Sousa Gonçalves2, and Hiron Marcos Barreto Rodrigues2 1Department of General and Specialized Surgery, Gaffrée e Guinle Teaching Hospital, Federal University of the State of Rio de Janeiro, Brazil 2Resident physician, Gafrée e Guinle Teaching Hospital, Federal University of the State of Rio de Janeiro, Brazil *Corresponding author: Célia Garritano, Department of General and Specialized Surgery, Gaffrée e Guinle Teaching Hospital, Federal University of the State of Rio de Janeiro, Brazil, Tel: 5521999882814; E-mail: [email protected] Received: 19 Aug, 2019 | Accepted: 16 Sep, 2019 | Published: 21 Sep, 2019 Citation: Garritano C, Chaves BL, Auad AMT, de Carvalho PFL, de Sousa Gonçalves T, et al. (2019) Cholecystoduodenal Fistula and Gallstone Ileus: A Case Report. J Surg Open Access 5(4): dx.doi.org/10.16966/2470-0991.190 Copyright: © 2019 Garritano C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract The gallstone ileus is a serious complication of cholelithiasis due to the formation of a fistula from the gallbladder to the subjacent duodenum. The gallstones are usually large enough to cause intestinal obstruction. -

Rigler Triad in Gallstone Ileus Lorena Brandariz-Gil, Tamara Fernández-De-Miguel and José Perea Department of General and Gastrointestinal Surgery
1130-0108/2016/108/9/581-582 REVISTA ESPAÑOLA DE ENFERMEDADES DIGESTIVAS REV ESP ENFERM DIG © Copyright 2016. SEPD y © ARÁN EDICIONES, S.L. 2016, Vol. 108, N.º 9, pp. 581-582 PICTURES IN DIGESTIVE PATHOLOGY Rigler triad in gallstone ileus Lorena Brandariz-Gil, Tamara Fernández-de-Miguel and José Perea Department of General and Gastrointestinal Surgery. Hospital Universitario 12 de Octubre. Madrid, Spain CASE REPORT An 82-year-old female was referred to our department with symptoms of abdominal distension and pain, con- stipation and vomiting in the past 48 hours. The clinical exam showed distension and diffuse abdominal pain, with no signs of peritonism. It was associated with 38 °C fever, leukocytosis and elevated creatinina in laboratory tests. The abdominal X-ray (Fig. 1) showed small bowel dil- Fig. 2. Chronic cholecystitis with cholelithiasis, associated with fistula (whi- atation as a result of an intestinal obstruction, an image te arrow). Intrahepatic aerobilia (black arrow). of lithiasis in the lower right quadrant and aerobilia. By abdominal CT scan, chronic cholecystitis, intrahepatic aerobilia, and a cholecystoduodenal fistula were recog- Surgical exeresis of the gallstone was performed to nized (Fig. 2), associated with an intestinal obstruction resolve the intestinal obstruction, with a second-look sur- caused by a gallstone in terminal ileum (gallstone ileus). gery for the cholecystoduodenal fistula. DISCUSSION Gallstone ileus is an infrequent complication of a bili- ary disease that produces an intestinal obstruction. This is a mechanic obstruction caused by a gallstone passing through a bilio-digestive communication, usually a cholecystoduo- denal fistula (1). It is more prevalent in elderly females as a result of an unresolved chronic cholecystitis. -

Small Bowel Obstruction Secondary to Gallstone Ileus with Finding of Rigler’S Triad on CT Abdomen: a Case Report
Case Report Clinics in Surgery Published: 09 Feb, 2017 Small Bowel Obstruction Secondary to Gallstone Ileus with Finding of Rigler’s Triad on CT Abdomen: A Case Report Raniga H, Shekhar A and Hendehewa R* Department of Surgery, Caboolture Hospital, Australia Abstract Gallstone ileus is an infrequent cause of small bowel obstruction. It mainly affects the elderly population with a female predominance. Many individuals often have concurrent history of chronic cholelithiasis. A fistula between the gallbladder and duodenum allow for the passage of a gallstone into the small bowel potentially leading to mechanical obstruction. Diagnosis can be difficult even with the help of modern imaging modalities which can lead to a delay in management and high risk of morbidity and mortality. This case demonstrates a commonly cited sign of gallstone ileus known as Rigler’s Triad; small bowel obstruction, a gallstone outside the gallbladder, and air in the biliary tree. Introduction Small bowel obstruction is a serious condition which has the potential to become a surgical emergency if left untreated. The most common causes of small bowel obstruction in adults include adhesions, hernias and tumour [1]. However, rarer causes of mechanical bowel obstruction should be considered if a diagnosis is uncertain. Gallstone ileus is an important but rare cause of small bowel obstruction accounting for about 1-4% of cases of intestinal obstruction [2]. The intermittent and variable symptomatology of gallstone ileus may potentially delay diagnosis which may be a contributing factor that accounts to its relatively high rate of associated morbidity and mortality. In this case, we describe a case of acute small bowel obstruction in a 58-year-old lady secondary to an impacted gallstone at the terminal ileum. -

Abdominal Pain and Vomiting in an Elderly Diabetic Woman Proptosis In
712 Postgrad Med J 2003;79:712–714 mechanical obstruction that might require Postgrad Med J: first published as 10.1136/pgmj.2002.004127a on 5 January 2004. Downloaded from SELF ASSESSMENT ANSWERS urgent enterolithotomy.4 The recurrence rate of gall stone ileus is less than 2%.2 Abdominal pain and vomiting Clinical features Usually abdominal pain is a prominent Final diagnosis in an elderly diabetic woman symptom, and associated illnesses such as diabetes and cardiovascular disease are com- Gall stone ileus. Q1: What abnormalities are seen on mon. It causes signs of small bowel obstruc- the plain film (fig 1; see p 709) and References tion like nausea, vomiting, abdominal 1 Foss HL, Summers JD. Intestinal obstruction from computed tomogram (fig 2; see p 709) distension, and absence of bowel sounds in gall stones. Ann Surg 1942;115:721–35. of the abdomen? cases of complete obstruction. Signs of 2 Reisner RM, Cohen JR. Gallstone ileus: a review Plain film shows air in the biliary tract and intestinal obstruction are seen mostly if the of 1001 reported cases. Am Surg gall bladder, dilated loops of small intestine, gall stone impacts at the ileocaecal junction. 1994;60:441–6. and multiple air-fluid levels in small bowel However, the characteristic features of intest- 3 Clavien PA, Richon J, Burgan S, et al. Gallstone loops. The computed tomogram shows large inal obstruction are found in only 50% to 70% ileus. Br J Surg 1990;77:737–42. of patients.23This may be because as the gall 4 Williams IM, Hughes ODM, Hicks E, et al. -

Gallstone Perforation of the Ileum Without Obstruction M. Parkert
Postgrad Med J: first published as 10.1136/pgmj.60.708.696 on 1 October 1984. Downloaded from Postgraduate Medical Journal (October 1984) 60, 696-697 Gallstone perforation of the ileum without obstruction S. SHANKAR* J. W. P. BRADLEY F.R.C.S. F.R.C.S. M. PARKERt F.R.C.S. Department of General Surgery, Harefield Hospital, Middlesex Summary A case of perforated ileum due to an impacted gall stone without associated intestinal obstruction, is reported. The problem in diagnosis and management are discussed. KEY WORDS: perforated ileum, gallstones. Introduction Gallstone ileus is a well recognized complication of copyright. cholelithiasis, usually associated with one or other form of cholecysto-enteric or choledocho-enteric fistula (Day and Marks, 1975). No case of perforated ileum due to asymptomatic impacted gallstone is g known by us to have been previously reported. The presentation and problems of management are de- scribed. http://pmj.bmj.com/ Case report A 74-year-old woman was admitted for investiga- tion of progressive anorexia and weight loss. She had been under medical treatment for congestive cardiac FIG. 1. Barium meal showing a biliary fistula between the common failure and hypothyroidism for some months. She bile duct and the first part of the duodenum. Air is present in the admitted to post-prandial vomiting, but had no biliary tree (arrow). dysphagia. There was no history of dyspepsia or jaundice. Her exercise tolerance was markedly di- duodenal diverticulum in the medial aspect of the on September 27, 2021 by guest. Protected minished. second part of the duodenum (Fig.