The Ilio-Coccygeus Muscle
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
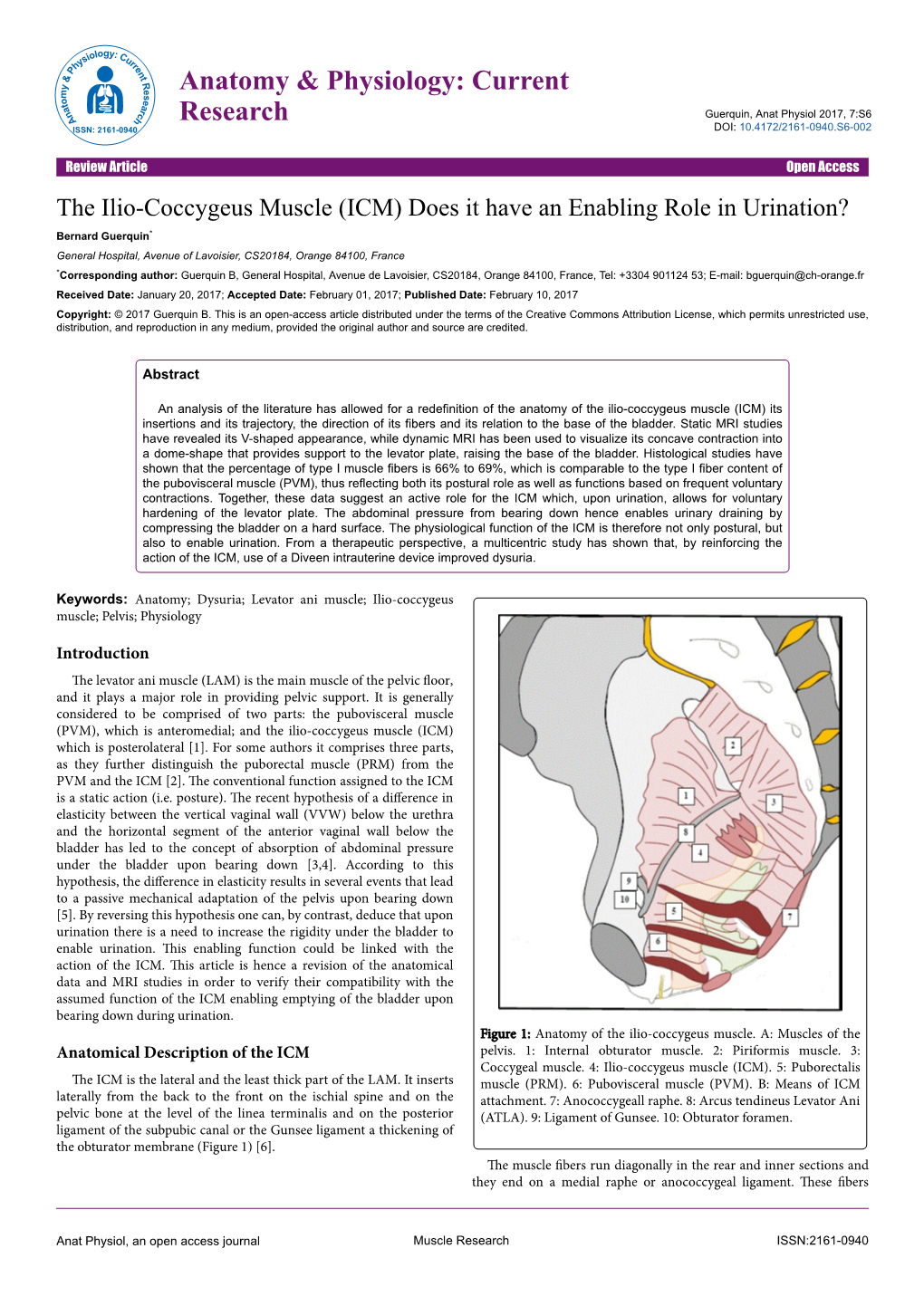
-

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

UNJ Dec 2000
C o n s e rvative Management of Female Patients With Pelvic Pain Hollis Herm a n he primary symptoms of Female patients with hy p e r t o nus of the pelvic musculature can ex p e- h y p e rtonus of the pelvic rience pain; burning in the cl i t o r i s , u r e t h r a , vag i n a , or anu s ; c o n s t i- m u s c u l a t u r e in female p a t i o n ; u r i n a ry frequency and urge n cy ; and dy s p a r e u n i a . P hy s i c a l patients include pain; t h e r a py techniques are effective in treating female patients with Tb u rning in the clitoris, ure t h r a , pelvic pain, and can successfully reduce the major symptoms asso- vagina or anus; constipation; uri- ciated with it. Using a treatment plan individualized for each patient’s n a ry frequency and urgency; and s y m p t o m s , these techniques can provide considerable relief to d y s p a reu nia (DeFranca, 1996). patients with debilitating pelvic pain. T h e re are many names for hyper- tonus diagnoses involving these symptoms including: levatore s ani syndrome (Nicosia, 1985; Salvanti, 1987; Sohn, 1982), ten- alignment and instability are pre- Olive, 1998), vaginal pH alter- sion myalgia (Sinaki, 1977), sent (Lee, 1999). -

Case Report for a Refractory Levator Ani Syndrome Treated With
J Korean Med. 2017;38(2):73-77 http://dx.doi.org/10.13048/jkm.17019 pISSN 1010-0695 • eISSN 2288-3339 Case Report Case Report for a Refractory Levator Ani Syndrome Treated with Traditional Korean Medication Chang-Gue Son Liver and Immunology Research Center, Oriental Medical College in Daejeon University Objectives: To inform a clinical case of a refractory levator ani syndrome, that was improved by treatments of traditional Korean medicine (TKM). Methods: A 55-years old female had complained severe anorectal pain which didn’t respond to Western medicine therapeutics during 5 months including 45-day hospitalization. Whereas the symptom was rapidly resolved by the treatment in a Korean medicine hospital, and the clinical outcome was monitored. Result: There was no abnormality explaining the anorectal pain from blood tests, gastrointestinal endoscopy, sonogram and computed tomography for abdomen and pelvis. The patient was diagnosed with a levator ani syndrome. Based on the typical feature of tenderness of lower abdomen as well as beating sign around belly, an herbal drug, Shihogayonggolmoryo-tang (柴胡加龍骨牡蠣湯) was prescribed. In addition, the warm acupuncture at BL 31 to BL 33 and moxibustion on lower abdomen were given to the patient. The anorectal pain was radically reduced from treatment 7-day, and it almost disappeared within treatment 25-day. Conclusion: This case report would provide information for the potential of TKM therapies focused on the refractory levator ani syndrome which no satisfactory therapy exist. Key Words : Levator ani syndrome, Functional rectal pain, Traditional Korean medicine Introduction The etiology of LAS is unknown, but spasm of the levator ani muscles without detectable organic Levator ani syndrome (LAS) and proctalgia fugax pathology is proposed4). -

Levator Ani Syndrome What Is Levator Ani Syndrome? Levator Ani Syndrome Results from Spasm in the Pelvic Floor Muscles
Levator Ani Syndrome What is Levator Ani Syndrome? Levator Ani Syndrome results from spasm in the pelvic floor muscles. It is often caused by trauma in or around the pelvis, abdomen or back. Weak muscles can also spasm. Determining Whether You Have Levator Ani Syndrome There are no laboratory tests for this condition. Levator Ani Syndrome is a collection of symptoms and findings. Not all patients have all the symptoms. Only your doctor can diagnose Levator Ani Syndrome. The most common symptoms include: • Deep dull aching in the rectum/vagina • Referred pain to the thigh and buttock • Sensation of “sitting on a ball.” Pain is worse in sitting and with bowel movement. • Spasms and pain in the pelvic floor muscle • Pain during or after intercourse • Tests usually show there is no inflammatory bowel disease, infection, ulcers or other bowel problem. Treatments • Medications to decrease muscle spasm and pain. • Biofeedback to learn how to relax and contract the pelvic floor muscles properly. • Electrical stimulation to the pelvic floor muscles can relax these muscles and increase circulation and promote healing. • TENS (transcutaneous electrical nerve stimulation) electrical stimulation to the pelvic floor nerves in the lower spine may help to “cover up” the pain and to relax the muscles. • Physical therapy to treat spasm in the buttock muscles or problems in the sacroiliac joint. • Heat and ultrasound can be used by physical therapists to relax the pelvic floor muscles. • A special form of rectal and buttock massage can be performed by the doctor or therapist to decrease pain and spasm.. -

Chronic Pelvic Pain & Pelvic Floor Myalgia Updated
Welcome to the chronic pelvic pain and pelvic floor myalgia lecture. My name is Dr. Maria Giroux. I am an Obstetrics and Gynecology resident interested in urogynecology. This lecture was created with Dr. Rashmi Bhargava and Dr. Huse Kamencic, who are gynecologists, and Suzanne Funk, a pelvic floor physiotherapist in Regina, Saskatchewan, Canada. We designed a multidisciplinary training program for teaching the assessment of the pelvic floor musculature to identify a possible muscular cause or contribution to chronic pelvic pain and provide early referral for appropriate treatment. We then performed a randomized trial to compare the effectiveness of hands-on vs video-based training methods. The results of this research study will be presented at the AUGS/IUGA Joint Scientific Meeting in Nashville in September 2019. We found both hands-on and video-based training methods are effective. There was no difference in the degree of improvement in assessment scores between the 2 methods. Participants found the training program to be useful for clinical practice. For both versions, we have designed a ”Guide to the Assessment of the Pelvic Floor Musculature,” which are cards with the anatomy of the pelvic floor and step-by step instructions of how to perform the assessment. In this lecture, we present the video-based training program. We have also created a workshop for the hands-on version. For more information about our research and workshop, please visit the website below. This lecture is designed for residents, fellows, general gynecologists, -

Transverse Abdominis Strengthening
10/20/2017 OBSTETRICS Objectives: The student should be Physical Therapy in Women’s able to: Health Care • Understand the roles and responsibilities of the physical therapist in working with obstetrical patients during and after pregnancy and Carol Figuers, PT, EdD childbirth Professor • Recognize physical therapy interventions for Doctor of Physical Therapy Division pregnancy & postpartum Duke University School of Medicine Hormonal Changes & Pelvic Girdle PT Interventions – Back Pain • Instability of joints • Symmetrical body movements • SI dysfunction main cause of • Small ranges of motion “back pain” in women* • “Baby Hugger” belts • Isometric exercises around pelvis and stabilization • Body mechanics Boissonnault JS, Klenstinski JU, Pearcy K. The role of *Garras et al. Single‐leg‐stance (flamingo) radiographs to assess pelvic instability: How exercise in the management of pelvic girdle and low much motion is normal? J Bone Joint Surg Am. 2008. back pain in pregnancy: A systematic review of the literature. JOWHPT, 2012. Transverse abdominis Check for Diastasis Recti strengthening 1 10/20/2017 Transversus Abdominis strengthening Tips for Managing Back Pain • Posture & Body Mechanics – Avoid carrying objects on one hip (assymmetry) – Avoid crossing legs – Carry loads in middle – Change positions frequently – Get muscles “ready” to move – Support lumbar spine – Watch body mechanics with ADL’s Tips for Managing Back Pain Suggestions for Healthy Exercise • Dealing with pain • Mild to moderate exercise at least 3 times/week – Have partner -

Anatomy of Pelvic Floor Dysfunction
Anatomy of Pelvic Floor Dysfunction Marlene M. Corton, MD KEYWORDS Pelvic floor Levator ani muscles Pelvic connective tissue Ureter Retropubic space Prevesical space NORMAL PELVIC ORGAN SUPPORT The main support of the uterus and vagina is provided by the interaction between the levator ani (LA) muscles (Fig. 1) and the connective tissue that attaches the cervix and vagina to the pelvic walls (Fig. 2).1 The relative contribution of the connective tissue and levator ani muscles to the normal support anatomy has been the subject of controversy for more than a century.2–5 Consequently, many inconsistencies in termi- nology are found in the literature describing pelvic floor muscles and connective tissue. The information presented in this article is based on a current review of the literature. LEVATOR ANI MUSCLE SUPPORT The LA muscles are the most important muscles in the pelvic floor and represent a crit- ical component of pelvic organ support (see Fig. 1). The normal levators maintain a constant state of contraction, thus providing an active floor that supports the weight of the abdominopelvic contents against the forces of intra-abdominal pressure.6 This action is thought to prevent constant or excessive strain on the pelvic ‘‘ligaments’’ and ‘‘fascia’’ (Fig. 3A). The normal resting contraction of the levators is maintained by the action of type I (slow twitch) fibers, which predominate in this muscle.7 This baseline activity of the levators keeps the urogenital hiatus (UGH) closed and draws the distal parts of the urethra, vagina, and rectum toward the pubic bones. Type II (fast twitch) muscle fibers allow for reflex muscle contraction elicited by sudden increases in abdominal pressure (Fig. -
![Perinea] Musculature in the Black Bengal Goat](https://docslib.b-cdn.net/cover/3469/perinea-musculature-in-the-black-bengal-goat-1623469.webp)
Perinea] Musculature in the Black Bengal Goat
J. Bangladesh Agril. Univ. 3(1): 77-82, 2005 ISSN 1810-3030 Perinea] musculature in the Black Bengal goat Z. Hague, M.A. Quasem, M.R. Karim and M.Z.1. Khan Department of Anatomy and Histology, Bangladesh Agricultural University, Mymensingh Abstract With the aim of preparing topographic descriptions and illustrations of the perineaj muscles of the black Bengal does, 12 adult animals were used. The animals were anaesthetized and bled to death by giving incision on the right common carotid artery. Whole vascular system was flashed with 0.85% physiological saline solution and then 10% formalin was injected through the same route for well preservation. After preservation, the muscles of the perineum were surgically isolated, transected and studied. It revealed that muscles of the pelvic diaphragm were M. levator ani and M. coccygeus. The M. levator ani was originated entirely from the sacrosciatic ligament and M. coccygeus from the medial side of the ischiatic spine and from the inside of the sacrotuberal ligament. M. levator ani was poorly developed and was blended with coccygeus for some distance at their insertion. Muscles of the urogenital diaphragm were M. urethralis, M. ischiourethralis and M. bulboglandularis. M. bulboglandularis was a small circular muscle which enclosed the major vestibular gland. Anal musculature of the perineum were M. sphincter ani externus, M. rectococcygeus and M. rectractor clitoridis. M. sphincter ani externus completely encircled the anus. Its fibers crossed ventral to the anus and continued into the opposite labium and the labium on the same side. M. rectococcygeus inserted on th the ventral surface of the 5th and 6 caudal vertebrae. -

Diastasis Recti Abdominus Association Spring Conference 2018
Diagnosis and treatment of DRA. 4/13/18 MPTA Spring Conference 2018. Kansas City Jennifer Cumming, PT, MSPT, Diagnosis and treatment of CLT, WCS Missouri Physical Therapy No disclosures Diastasis Recti Abdominus Association Spring Conference 2018 Objective Case study #1 complaints 1. Understand anatomy of abdominal wall and deep motor control • Mrs. H is 37 year old who is 6 months post-partum system • Back pain since late pregnancy and postpartum period. 2. Understand the causes and prevalence of diastasis rectus • Pain not responding to traditional physical therapy abdominus (DRA) • Pain with transition movements and bending 3. Understand how to assess for DRA • Also c/o stress urinary incontinence and pain with intercourse 4. Understand basic treatment strategies for improving functionality of abdominal wall and deep motor control system Case study #1 orthopedic assessment Case study #2 complaints • 1 ½ finger diastasis rectus abdominus just inferior to umbilicus • Ms. S is a 20 year old elite college level athlete • Active straight leg raise (ASLR) with best correction at PSIS indicating • History of DRA developing with high level athletic training involvement of posterior deep motor control system • Complains of LBP with prolonged sitting, bending, and lifting activities • L3 right rotation at level of DRA • Hypertonicity B internal oblique muscles Property of J Cumming, PT, MSPT, CLT, WCS. Do not copy without permission. 1 Diagnosis and treatment of DRA. 4/13/18 MPTA Spring Conference 2018. Kansas City Case study #2 orthopedic assessment -

Female Chronic Pelvic Pain Syndromes 1 Standard of Care
BRIGHAM AND WOMEN’S HOSPITAL Department of Rehabilitation Services Physical Therapy Standard of Care: Female Chronic Pelvic Pain Syndromes ICD 9 Codes: 719.45 Pain in the pelvic region 625.9 Vulvar/pelvic pain/vulvodynia/vestibulodynia (localized provoked vestibulodynia or unprovoked) 625.0 Dyspareunia 595.1 Interstitial cystitis/painful bladder syndrome 739.5 Pelvic floor dysfunction 569.42 Anal/rectal pain 564.6 Proctalgia fugax/spasm anal sphincter 724.79 Coccygodynia 781.3 Muscular incoordination (other possible pain diagnoses: prolapse 618.0) Case Type/Diagnosis: Chronic pelvic pain (CPP) can be defined as: “non-malignant pain perceived in structures related to the pelvis, in the anterior abdominal wall below the level of the umbilicus, the spine from T10 (ovarian nerve supply) or T12 (nerve supply to pelvic musculoskeletal structures) to S5, the perineum, and all external and internal tissues within these reference zones”. 1 Specifically, pelvic pain syndrome has been further defined as: “the occurrence of persistent or recurrent episodic pelvic pain associated with symptoms suggestive of lower urinary tract, sexual, bowel or gynecological dysfunction with no proven infection or other obvious pathology”.1 Generally, female pelvic pain has been defined as pain and dysfunction in and around the pelvic outlet, specifically the suprapubic, vulvar, and anal regions. A plethora of various terms/diagnoses encompass pelvic pain as a symptom, including but not limited to: chronic pelvic pain (CPP), vulvar pain, vulvodynia, vestibulitis/vestibulodynia (localized provoked vestibulodynia or unprovoked vestibulodynia), vaginismus, dyspareunia, interstitial cystitis (IC)/painful bladder syndrome (PBS), proctalgia fugax, levator ani syndrome, pelvic floor dysfunction, vulvodynia, vestibulitis/vestibulodynia dyspareunia, vaginismus, coccygodynia, levator ani syndrome, tension myaglia of the pelvic floor, shortened pelvic floor, and muscular incoordination of the pelvic floor muscles. -

Levator Ani Syndrome Review a Case Study and Literature Review
CLINICAL PRACTICE Levator ani syndrome Review A case study and literature review BACKGROUND Although anorectal symptoms are a common problem seen in general practice, general practitioners may sometimes Ching Luen Ng encounter patients presenting with anorectal pain without a detectable cause. MBBS, FRACGP, FHKCFP, FHKAM(FamMed) is a trainer in OBJECTIVE Family Medicine, Kowloon West This article discusses a case of recurrent anorectal pain in a young woman due to levator ani syndrome, and the current Cluster, Hospital Authority, Hong evidence for treatment of levator ani syndrome. Kong, and Doctor-in-charge, Ha Kwai Chung General Out Patient DISCUSSION Clinic, Kwai Chung. chingluen@ Levator ani syndrome usually presents with recurrent or chronic rectal pain without detectable organic pathology. yahoo.com.hk Digital massage, sitz bath, muscle relaxants, electrogalvanic stimulation and biofeedback are the treatment modalities most frequently described in the literature. Case study – Ms C Ms C, a 28 year old registered nurse, attended my clinic because of anal pain for 4 hours. She described that the pain had started shortly after defaecation on that morning and was ‘constricting’ in nature and ‘moderate’ in severity. There was no rectal bleeding and no recent change of bowel habit. She denied any previous or recent anal sex. She had had two similar attacks in the past 4 months. She did not consult a doctor with the previous episodes because the anal pain subsided within 2–3 hours. On proctoscopic and per rectal examination, no anal fissure, fistula-in-ano, perianal abscess, haemorrhoids, perianal haematoma, rectal tumour or ulcer could be found. There was mild tenderness at the left side of the rectal canal. -

Anatomy and Histology of Apical Support: a Literature Review Concerning Cardinal and Uterosacral Ligaments
Int Urogynecol J DOI 10.1007/s00192-012-1819-7 REVIEW ARTICLE Anatomy and histology of apical support: a literature review concerning cardinal and uterosacral ligaments Rajeev Ramanah & Mitchell B. Berger & Bernard M. Parratte & John O. L. DeLancey Received: 10 February 2012 /Accepted: 24 April 2012 # The International Urogynecological Association 2012 Abstract The objective of this work was to collect and Autonomous nerve fibers are a major constituent of the deep summarize relevant literature on the anatomy, histology, USL. CL is defined as a perivascular sheath with a proximal and imaging of apical support of the upper vagina and the insertion around the origin of the internal iliac artery and a uterus provided by the cardinal (CL) and uterosacral (USL) distal insertion on the cervix and/or vagina. It is divided into ligaments. A literature search in English, French, and Ger- a cranial (vascular) and a caudal (neural) portions. Histolog- man languages was carried out with the keywords apical ically, it contains mainly vessels, with no distinct band of support, cardinal ligament, transverse cervical ligament, connective tissue. Both the deep USL and the caudal CL are Mackenrodt ligament, parametrium, paracervix, retinaculum closely related to the inferior hypogastric plexus. USL and uteri, web, uterosacral ligament, and sacrouterine ligament CL are visceral ligaments, with mesentery-like structures in the PubMed database. Other relevant journal and text- containing vessels, nerves, connective tissue, and adipose book articles were sought by retrieving references cited in tissue. previous PubMed articles. Fifty references were examined in peer-reviewed journals and textbooks. The USL extends Keywords Apical supports .