Topicort (Desoximetasone)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group D07A (Corticosteroids, Plain) Table of Contents Page INTRODUCTION 4 DISCLAIMER 6 GLOSSARY OF TERMS USED IN THIS DOCUMENT 7 ACTIVE SUBSTANCES Methylprednisolone (ATC: D07AA01) 8 Hydrocortisone (ATC: D07AA02) 9 Prednisolone (ATC: D07AA03) 11 Clobetasone (ATC: D07AB01) 13 Hydrocortisone butyrate (ATC: D07AB02) 16 Flumetasone (ATC: D07AB03) 18 Fluocortin (ATC: D07AB04) 21 Fluperolone (ATC: D07AB05) 22 Fluorometholone (ATC: D07AB06) 23 Fluprednidene (ATC: D07AB07) 24 Desonide (ATC: D07AB08) 25 Triamcinolone (ATC: D07AB09) 27 Alclometasone (ATC: D07AB10) 29 Hydrocortisone buteprate (ATC: D07AB11) 31 Dexamethasone (ATC: D07AB19) 32 Clocortolone (ATC: D07AB21) 34 Combinations of Corticosteroids (ATC: D07AB30) 35 Betamethasone (ATC: D07AC01) 36 Fluclorolone (ATC: D07AC02) 39 Desoximetasone (ATC: D07AC03) 40 Fluocinolone Acetonide (ATC: D07AC04) 43 Fluocortolone (ATC: D07AC05) 46 2 Diflucortolone (ATC: D07AC06) 47 Fludroxycortide (ATC: D07AC07) 50 Fluocinonide (ATC: D07AC08) 51 Budesonide (ATC: D07AC09) 54 Diflorasone (ATC: D07AC10) 55 Amcinonide (ATC: D07AC11) 56 Halometasone (ATC: D07AC12) 57 Mometasone (ATC: D07AC13) 58 Methylprednisolone Aceponate (ATC: D07AC14) 62 Beclometasone (ATC: D07AC15) 65 Hydrocortisone Aceponate (ATC: D07AC16) 68 Fluticasone (ATC: D07AC17) 69 Prednicarbate (ATC: D07AC18) 73 Difluprednate (ATC: D07AC19) 76 Ulobetasol (ATC: D07AC21) 77 Clobetasol (ATC: D07AD01) 78 Halcinonide (ATC: D07AD02) 81 LIST OF AUTHORS 82 3 INTRODUCTION The availability of medicines with or without a medical prescription has implications on patient safety, accessibility of medicines to patients and responsible management of healthcare expenditure. The decision on prescription status and related supply conditions is a core competency of national health authorities. -

Aetna Formulary Exclusions Drug List
Covered and non-covered drugs Drugs not covered – and their covered alternatives 2020 Advanced Control Plan – Aetna Formulary Exclusions Drug List 05.03.525.1B (7/20) Below is a list of medications that will not be covered without a Key prior authorization for medical necessity. If you continue using one of these drugs without prior approval, you may be required UPPERCASE Brand-name medicine to pay the full cost. Ask your doctor to choose one of the generic lowercase italics Generic medicine or brand formulary options listed below. Preferred Options For Excluded Medications1 Excluded drug name(s) Preferred option(s) ABILIFY aripiprazole, clozapine, olanzapine, quetiapine, quetiapine ext-rel, risperidone, ziprasidone, VRAYLAR ABSORICA isotretinoin ACANYA adapalene, benzoyl peroxide, clindamycin gel (except NDC^ 68682046275), clindamycin solution, clindamycin-benzoyl peroxide, erythromycin solution, erythromycin-benzoyl peroxide, tretinoin, EPIDUO, ONEXTON, TAZORAC ACIPHEX, esomeprazole, lansoprazole, omeprazole, pantoprazole, DEXILANT ACIPHEX SPRINKLE ACTICLATE doxycycline hyclate capsule, doxycycline hyclate tablet (except doxycycline hyclate tablet 50 mg [NDC^ 72143021160 only], 75 mg, 150 mg), minocycline, tetracycline ACTOS pioglitazone ACUVAIL bromfenac, diclofenac, ketorolac, PROLENSA acyclovir cream acyclovir (except acyclovir cream), valacyclovir ADCIRCA sildenafil, tadalafil ADZENYS XR-ODT amphetamine-dextroamphetamine mixed salts ext-rel†, dexmethylphenidate ext-rel, dextroamphetamine ext-rel, methylphenidate ext-rel†, MYDAYIS, -

Pre - PA Allowance Age 18 Years of Age Or Older Quantity 60 Grams Every 90 Days ______
DOXEPIN CREAM 5% (Prudoxin, Zonalon) Pre - PA Allowance Age 18 years of age or older Quantity 60 grams every 90 days _______________________________________________________________ Prior-Approval Requirements Age 18 years of age or older Diagnosis Patient must have the following: Moderate pruritus, due to atopic dermatitis (eczema) or lichen simplex chronicus AND the following: 1. Inadequate response, intolerance or contraindication to ONE medication in EACH of the following categories: a. Topical antihistamine (see Appendix I) b. High potency topical corticosteroid (see Appendix II) 2. Physician agrees to taper patient’s dose to the FDA recommended dose, and after tapered will only use for short-term pruritus relief (up to 8 days) a. Patients using over 60 grams of topical doxepin in 90 days be required to taper to 60 grams topical doxepin within 90 days Prior - Approval Limits Quantity 180 grams for 90 days Duration 3 months ___________________________________________________________________ Prior – Approval Renewal Requirements None (see appendix below) Doxepin 5% cream FEP Clinical Rationale DOXEPIN CREAM 5% (Prudoxin, Zonalon) APPENDIX I Drug Dosage Form Diphenhydramine Cream Phenyltoloxamine Lotion/ Cream Tripelennamine Cream Phendiamine Cream APPENDIX II Relative Potency of Selected Topical Corticosteroid Drug ProductsDosage Form Strength I. Very high potency Augmented betamethasone Ointment, Gel 0.05% dipropionate Clobetasol propionate Cream, Ointment 0.05% Diflorasone diacetate Ointment 0.05% Halobetasol propionate Cream, Ointment 0.05% II. High potency Amcinonide Cream, Lotion, 0.1% Augmented betamethasone Cream,Ointment Lotion 0.05% dipropionate Betamethasone Cream, Ointment 0.05% Betamethasonedipropionate valerate Ointment 0.1% Desoximetasone Cream, Ointment 0.25% Gel 0.05% Diflorasone diacetate Cream, Ointment 0.05% (emollient base) Fluocinonide Cream, Ointment, Gel 0.05% Halcinonide Cream, Ointment 0.1% Triamcinolone acetonide Cream, Ointment 0.5% III. -

CMS Backs Coverage for Diet, Lifestyle Changes
60 Practice Trends S KIN & ALLERGY N EWS • March 2005 CMS Backs Coverage for Diet, Lifestyle Changes BY JOYCE FRIEDEN of how much patients improved on the pro- may be self-selecting for the program at a regimens such as that of Dr. Ornish. Associate Editor, Practice Trends gram was adherence. “The more people time when their weight and other negative But Dr. Ornish said he was merely ask- changed, the better they got,” he noted. indicators are at their peak. “How much ing for these types of programs to be treat- B ALTIMORE — There might not have Advisory committee members ex- of the effect we’re observing is simply re- ed the same way as other interventions. been thunderous applause at the meeting pressed several concerns about Dr. Or- gression to the mean?” he asked. “We will pay for bypass surgery and an- of the Medicare Coverage Advisory Com- nish’s results. Dr. Ornish admitted that there was gioplasty, but diet and lifestyle interven- mittee, but the quiet approval was quite Clifford Goodman, Ph.D., a senior sci- some regression but added, “there is a di- tions, Medicare generally doesn’t pay for enough for Dean Ornish, M.D. entist with the Lewin Group, a Falls rect correlation between degree of ad- it,” he said, adding that many insurers pay The committee, which advises Medicare Church, Va. consulting firm, noted that herence and outcomes at 1 year.” for cholesterol-lowering statin drugs even on coverage issues, voted to recommend some of the improvements in the patient Adherence was a concern for several though studies have shown that patients that Medicare cover the use of physician- groups started to reverse slightly after a panel members who wondered whether go off the drugs after a few months be- supervised intensive diet and lifestyle year, and speculated that many patients patients could really keep up with strict cause they don’t like the side effects. -

Wo 2008/127291 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (43) International Publication Date PCT (10) International Publication Number 23 October 2008 (23.10.2008) WO 2008/127291 A2 (51) International Patent Classification: Jeffrey, J. [US/US]; 106 Glenview Drive, Los Alamos, GOlN 33/53 (2006.01) GOlN 33/68 (2006.01) NM 87544 (US). HARRIS, Michael, N. [US/US]; 295 GOlN 21/76 (2006.01) GOlN 23/223 (2006.01) Kilby Avenue, Los Alamos, NM 87544 (US). BURRELL, Anthony, K. [NZ/US]; 2431 Canyon Glen, Los Alamos, (21) International Application Number: NM 87544 (US). PCT/US2007/021888 (74) Agents: COTTRELL, Bruce, H. et al.; Los Alamos (22) International Filing Date: 10 October 2007 (10.10.2007) National Laboratory, LGTP, MS A187, Los Alamos, NM 87545 (US). (25) Filing Language: English (81) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of national protection available): AE, AG, AL, AM, AT,AU, AZ, BA, BB, BG, BH, BR, BW, BY,BZ, CA, CH, (30) Priority Data: CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, 60/850,594 10 October 2006 (10.10.2006) US ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, (71) Applicants (for all designated States except US): LOS LR, LS, LT, LU, LY,MA, MD, ME, MG, MK, MN, MW, ALAMOS NATIONAL SECURITY,LLC [US/US]; Los MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PG, PH, PL, Alamos National Laboratory, Lc/ip, Ms A187, Los Alamos, PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, SV, SY, NM 87545 (US). -
Dupixent (Dupilumab)
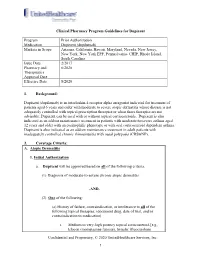
Clinical Pharmacy Program Guidelines for Dupixent Program Prior Authorization Medication Dupixent (dupilumab) Markets in Scope Arizona, California, Hawaii, Maryland, Nevada, New Jersey, New York, New York EPP, Pennsylvania- CHIP, Rhode Island, South Carolina Issue Date 2/2017 Pharmacy and 6/2020 Therapeutics Approval Date Effective Date 8/2020 1. Background: Dupixent (dupilumab) is an interleukin-4 receptor alpha antagonist indicated for treatment of patients aged 6 years and older with moderate to severe atopic dermatitis whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. Dupixent can be used with or without topical corticosteroids. Dupixent is also indicated as an add-on maintenance treatment in patients with moderate-to-severe asthma aged 12 years and older with an eosinophilic phenotype or with oral corticosteroid dependent asthma. Dupixent is also indicated as an add-on maintenance treatment in adult patients with inadequately controlled chronic rhinosinusitis with nasal polyposis (CRSwNP). 2. Coverage Criteria: A. Atopic Dermatitis 1. Initial Authorization a. Dupixent will be approved based on all of the following criteria: (1) Diagnosis of moderate-to-severe chronic atopic dermatitis -AND- (2) One of the following: (a) History of failure, contraindication, or intolerance to all of the following topical therapies: (document drug, date of trial, and/or contraindication to medication) i. Medium to very-high potency topical corticosteroid [e.g., Elocon (mometasone furoate), Synalar (fluocinolone Confidential and Proprietary, © 2020 UnitedHealthcare Services, Inc. 1 acetonide), Lidex (fluocinonide)] ii. One topical calcineurin inhibitor [e.g., Elidel (pimecrolimus), Protopic (tacrolimus)] iii. Eucrisa (crisaborole) -OR- (b) Both of the following: i. -

Proteome-Scale Detection of Drug-Target Interactions Using Correlations in Transcriptomic Perturbations
bioRxiv preprint doi: https://doi.org/10.1101/254367; this version posted January 25, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Proteome-scale detection of drug-target interactions using correlations in transcriptomic perturbations Nicolas A. Pabon1,✝, Yan Xia2,✝, Samuel K. Estabrooks3, Zhaofeng Ye4, Amanda K. Herbrand5, Evelyn Süß5, Ricardo M. Biondi5, Victoria A. Assimon6, Jason E. Gestwicki6, Jeffrey L. Brodsky3, Carlos J. Camacho1,*, and Ziv Bar-Joseph2 1 Department of Computational and Systems Biology, University of Pittsburgh , Pittsburgh, PA 15213 2 Machine Learning Department, School of Computer Science, Carnegie Mellon University, 15213 3 Department of Biological Sciences, University of Pittsburgh, Pittsburgh, PA 15260 4 School of Medicine, Tsinghua University, Beijing, China 100084 5 Department of Internal Medicine I, Universitätsklinikum Frankfurt, 60590 Frankfurt, Germany 6 Department of Pharmaceutical Chemistry, University of California, San Francisco, San Francisco, CA 94158 ✝ These two authors contributed equally * To whom correspondence should be addressed Corresponding Author: Carlos Camacho 3077 Biomedical Science Tower 3 3501 Fifth Avenue Pittsburgh, PA 15260 412-648-7776, Fax: 412-648-3163 E-mail: [email protected] http://structure.pitt.edu 1 bioRxiv preprint doi: https://doi.org/10.1101/254367; this version posted January 25, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Keywords: LINCS, polypharmacology, target prediction, drug discovery, gene expression, virtual screen, high-throughput Availability: Supplementary Methods, Results, Data and Matlab code are available at the supporting website http://sb.cs.cmu.edu/Target2/. -

A Review of Topical Corticosteroid Sprays for the Treatment of Inflammatory Dermatoses
Volume 25 Number 8| August 2019| Dermatology Online Journal || Review 25(8):3 A review of topical corticosteroid sprays for the treatment of inflammatory dermatoses Kyle A Habet1 MD, Sree S Kolli1 BA, Adrian Pona1 MD, Steven R Feldman1,2,3 MD PhD Affiliations: 1Center for Dermatology Research, Department of Dermatology, Wake Forest School of Medicine, Winston-Salem, North Carolina, 2Department of Pathology, Wake Forest School of Medicine, Winston-Salem, North Carolina, 3Department of Social Sciences & Health Policy, Wake Forest School of Medicine, Winston-Salem, North Carolina Corresponding Author: Kyle A. Habet, MD, Department of Dermatology, Wake Forest School of Medicine, Medical Center Boulevard, Winston-Salem, NC 27157-1071, Tel: 06 8616-0331, E-mail: [email protected] Introduction Abstract Topical corticosteroids are ubiquitous in the Background: Topical corticosteroids are available in treatment of various dermatoses [1]. Vehicles many vehicles. However, patients’ preference for available for topical corticosteroids include creams, vehicles are variable and could be tailored to ointments, gels, lotions, solutions, and sprays. maximize patient adherence. Spray vehicles may Although ointments, creams, and gels are often offer, convenience, and strong efficacy. prescribed, an increasing use of nontraditional Methods: A literature review was conducted using vehicles, including sprays and foams, are being keywords: clobetasol, desoximetasone, betamethasone, triamcinolone, corticosteroid, prescribed for psoriasis and other inflammatory -

Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Psoriasis
Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Psoriasis Diagnosis: PSORIASIS TREATMENT RECOMMENDATIONS: • Careful physical exam for possible strep infection (throat, perianal area, inguinal folds) and treatment if positive. • Careful history for persistent or frequent history of morning stiffness or joint pain Location Eyelids Elidel 1% cream (or other calcineurin inhibitor) Face, Axillae, Hydrocortisone 2.5% ointment (or other Class 6 or 7 topical steroid) Inguinal Folds Body Thin/mild: Triamcinolone 0.1% ointment (or other Class 3, 4 topical steroid) Thick/severe: Mometasone 0.1% ointment (or other Class 1 or 2 topical steroid) Scalp Mild (or patients with dry hair): Fluocinolone 0.01% (Derma-smoothe) oil Severe: Clobetasol 0.05 % solution Shampoo: (over-the-counter) • Salicylic acid containing shampoo (e.g. T sal shampoo) • Tar containing shampoo (e.g. T gel shampoo) • Baker’s P&S shampoo Nails Mometasone 0.1% ointment (or other Class 1 or 2 topical steroid) • Apply medication to nail folds/cuticle PATIENT RESOURCES: National Psoriasis Foundation www.psoriasis.org REFERRAL RECOMMENDATIONS: • Please refer patient if there is extensive involvement (>5-10% BSA), or localiZed involvement that has failed treatment recommendations above. • If patient has persistent morning stiffness or joint complaints, please also refer to rheumatology for evaluation for possible psoriatic arthritis Educational recommendations are made from the best evidence, expert opinions and consideration for the patients and families cared for by the service. This is NOT intended to impose standards of care preventing selective variation in practice that are necessary to meet the unique needs of individual patients. The physician must consider each patient’s circumstance to make the ultimate judgment regarding best care. -

Nickel Contact Dermatitis
Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Nickel Contact Dermatitis Diagnosis: NICKEL CONTACT DERMATITIS GENERAL INFORMATION: • Most common presentation is an erythematous scaly plaque under the umbilicus secondary to nickel-containing snaps on pants. • May also present around the ears, neck, wrist, cheeks, or axilla, corresponding to contact with jewelry, watches, cell phones, or razors. • Sometimes, especially in severe cases, may be accompanied by “id reaction” with scattered skin-colored papules often concentrated on the forehead, elbows and/or knees. TREATMENT RECOMMENDATIONS: • Avoid nickel-containing products! o Common sources of nickel are belt buckles, buttons on jeans, and costume jewelry o In general, >22k gold, titanium, and platinum jewelry is safe to use o If complete avoidance is not possible (e.g. school uniform), to minimize contact of skin with nickel, can apply clear nail polish to the nickel containing metal. The clear nail polish will need to be periodically reapplied. Shirts or clothing may also be tucked in. • Consider using triamcinolone 0.1% ointment (or other Class 1, 2, or 3 topical steroid) to help symptoms of pruritus; however, the rash will not resolve or will recur with continued or repeat exposure to nickel. Class 1 (Ultrapotent) Class 2 (High Potency) Class 3 (High Potency) Clobetasol propionate 0.05% ointment, cream Amcinonide 0.1% ointment Amcinonide 0.1% cream Betamethasone dipropionate 0.05% ointment Betamethasone dipropionate 0.05% ointment, Betamethasone dipropionate -

Desoximetasone 0.25% and Tacrolimus 0.1% Ointments Versus Tacrolimus Alone in the Treatment of Atopic Dermatitis
THERAPEUTICS FOR THE CLINICIAN Desoximetasone 0.25% and Tacrolimus 0.1% Ointments Versus Tacrolimus Alone in the Treatment of Atopic Dermatitis Adelaide A. Hebert, MD; John Koo, MD; Joseph Fowler, MD; Brian Berman, MD, PhD; Carl Rosenberg, PhD; Jacob Levitt, MD Long-term in vitro compatibility of desoximeta- pruritus at the application site was diminished in sone and tacrolimus ointments prompted the subjects treated with desoximetasone and tacro- current trial in humans. We aimed to evaluate limus together compared with tacrolimus alone the efficacy of twice-daily simultaneous appli- (P=.04). Combination treatment with desoximeta- cation of desoximetasone and tacrolimus in the sone and tacrolimus offered increased efficacy treatment of atopic dermatitis versus tacrolimus and tolerability over tacrolimus alone in patients monotherapy. Eighty-two subjects were treated with atopic dermatitis. in this multicenter, single-group, double-blinded, Cutis. 2006;78:357-363. paired, 3-week follow-up clinical study of desox- imetasone 0.25% and tacrolimus 0.1% ointments versus tacrolimus 0.1% ointment and vehicle. ombination therapy is a mainstay of topi- Subjects were treated twice daily for 21 days or cal dermatologic therapeutics. Classically, this until clearing. Safety and efficacy were assessed C strategy has been employed to treat psoriasis.1-3 at days 3, 7, 14, and 21. The combination of Often, physicians take for granted that 2 ointments, desoximetasone and tacrolimus ointment was when simultaneously applied, will be compatible and superior to tacrolimus alone (P=.0002) in treating that one will not degrade in the presence of the other. atopic dermatitis as measured by the summary of However, topical drug incompatibilities do exist. -

Diaper Dermatitis
Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Diaper Dermatitis Diagnosis: DIAPER DERMATITIS GENERAL INFORMATION: • Diaper dermatitis, regardless of cause, can frequently recur until the patient is toilet-trained and out of diapers. • Irritant contact dermatitis is favored when there are satellite papules/pustules and spares the inguinal folds • Candidal diaper dermatitis is favored when there are satellite papules/pustules and often involves the inguinal folds. • Cleaning recommendations o Can use a spray bottle or warm running water with soft wash cloth or flannel wipes to clean. o If necessary, use fragrance and preservative free wet wipes (e.g. Seventh Generation or Pampers Sensitive Brands) • Barrier methods o Use thick layer (“like icing on a cake”) of Vaseline or Aquaphor with each diaper change OR o Use thick layer (“like frosting on a cake”) extra strength destin (40% zinc oxide). When changing the diaper, do NOT remove the “frosting”. Just pat dry and put more frosting on. The only time, baby’s skin on bottom should be seen is after a bowel movement or after bathing. • Families should be reminded that topical steroids should not be used on a daily basis, only for short intervals during flares. • If diaper dermatitis is refractory to treatment, especially if there is facial involvement, consider assessing for zinc deficiency. TREATMENT RECOMMENDATIONS: • Mild: Start hydrocortisone 2.5% ointment (or other Class 5 or 6 topical steroid) mixed in equal amounts with miconazole 1% cream (or other anti-Candidal alternative) twice daily until improvement is seen. Follow application with a thick layer of Vaseline or Aquaphor.