On the Just and Accurate Representation of Transgender Persons in Research and the Clinic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Attraction and Sex Symbol of Males in the Eyes of Malaysian Male-To-Female Transsexuals
International Journal of Social Science and Humanity, Vol. 3, No. 2, March 2013 Attraction and Sex Symbol of Males in the Eyes of Malaysian Male-to-Female Transsexuals Amran Hassan and Suriati Ghazali they are female in emotion but „trapped‟ in the male bodies. Abstract—Male-to-female transsexual issues, especially their sexual orientation, has become complicated due to their tendency to regard themselves as women, and are exclusively II. REVIEW OF LITERATURE attracted to men. This paper explores one group in male-to-female transsexuals, which is homosexual transsexuals, Research on male-to-female transsexuals‟ sexual attraction and their attraction towards homosexual and heterosexual men. towards men is still scarce. One among a few is by [7], who The objective of this paper is to identify aspects of sexual discovered that attraction to Male Physique was positively attraction in the body or nature of the men that attract correlated with Sexual Attraction to Males among homosexual transsexuals to develop romantic relationship with Autogynephilic transsexuals. It is possible that attraction to them. Qualitative methods were used in gathering the data. This includes in-depth interviews that have been carried out on six the male physique could develop along with the secondary homosexual transsexuals, which were selected using purposive emergence of attraction to males that [5] describes. and snowball sampling. The location of the fieldwork was Port Transsexual research in Malaysia generally focuses on Dickson, Negeri Sembilan, Malaysia. The result shows that factors leading to transsexualism and issues around it, rather facial appearance, specific body parts such as chest, calves and than sexuality and sexual attraction. -

Early History of the Concept of Autogynephilia
Archives of Sexual Behavior, Vol. 34, No. 4, August 2005, pp. 439–446 (C 2005) DOI: 10.1007/s10508-005-4343-8 Early History of the Concept of Autogynephilia Ray Blanchard, Ph.D.1,2,3 Received August 4, 2004; revision received November 27, 2004; accepted November 27, 2004 Since the beginning of the last century, clinical observers have described the propensity of certain males to be erotically aroused by the thought or image of themselves as women. Because there was no specific term to denote this phenomenon, clinicians’ references to it were generally oblique or periphrastic. The closest available word was transvestism. The definition of transvestism accepted by the end of the twentieth century, however, did not just fail to capture the wide range of erotically arousing cross-gender behaviors and fantasies in which women’s garments per se play a small role or none at all; it actually directed attention away from them. The absence of an adequate terminology became acute in the writer’s research on the taxonomy of gender identity disorders in biological males. This had suggested that heterosexual, asexual, and bisexual transsexuals are more similar to each other—and to transvestites—than any of them is to the homosexual type, and that the common feature in transvestites and the three types of non-homosexual transsexuals is a history of erotic arousal in association with the thought or image of themselves as women. At the same time, the writer was becoming aware of male patients who are sexually aroused only by the idea of having a woman’s body and not at all by the idea of wearing women’s clothes. -

The Psychopathology of “Sex Reassignment” Surgery Assessing Its Medical, Psychological, and Ethical Appropriateness
The Psychopathology of “Sex Reassignment” Surgery Assessing Its Medical, Psychological, and Ethical Appropriateness Richard Fitzgibbons, M.D., Philip M. Sutton, and Dale O’Leary Abstract. Is it ethical to perform a surgery whose purpose is to make a male look like a female or a female to appear male? Is it medically appropri- ate? Sexual reassignment surgery (SRS) violates basic medical and ethical principles and is therefore not ethically or medically appropriate. (1) SRS mutilates a healthy, non-diseased body. To perform surgery on a healthy body involves unnecessary risks; therefore, SRS violates the principle primum non nocere, “first, do no harm.” (2) Candidates for SRS may believe that they are trapped in the bodies of the wrong sex and therefore desire or, more accurately, demand SRS; however, this belief is generated by a disordered perception of self. Such a fixed, irrational belief is appropriately described as a delusion. SRS, therefore, is a “category mistake”—it offers a surgical solution for psychological problems such as a failure to accept the goodness Richard Fitzgibbons, M.D., a psychiatrist, is the director of Comprehensive Coun- seling Services outside Philadelphia. Philip Sutton, Ph.D., is a psychologist in private practice in South Bend, Indiana; he also works in elementary schools in the Diocese of Fort Wayne–South Bend and at Sacred Heart Major Seminary in Detroit. Dale O’Leary is the author of One Man One Woman: A Catholic’s Guide to Defending Marriage and The Gender Agenda: Redefining Equality. © 2009 The National Catholic Bioethics Center 97 THE NATIONAL CATHOLIC BIOETHICS QUARTERLY SPRING 2009 of one’s masculinity or femininity, lack of secure attachment relationships in childhood with same-sex peers or a parent, self-rejection, untreated gender identity disorder, addiction to masturbation and fantasy, poor body image, excessive anger, and severe psychopathology in a parent. -

Transgenderism in Buddhism RELIG ST 4H03 Carolynn Chennery 12.09.15
Destroying the Binary: Transgenderism in Buddhism RELIG ST 4H03 Carolynn Chennery 12.09.15 If doctrines and medical texts of Buddhism show a relationship between the third gender and a bodhisattvas being that achieves nirvana, why is there discrimination towards transgenderism and how can we explore it to understand it? Buddhism is a religion that seeks peace and an escape from rebirth of suffering for every being, regardless of their biological sex. Despite Buddhism’s origins in a patriarchal society like most religions, it offers both men and women the ability to achieve enlightenment, viewing them as equal like in the Lotus Sutra, one of Buddhism’s most important literature pieces. Not much is written or known about the third transgendered being though in regards to how they are accepted within Buddhism and their abilities to achieve nirvana. Being transgendered is a seemingly taboo identity and invites controversy in many societies, but key scriptures of Mahayana Buddhism such as the Lotus Sutra and Vimalakirti Sutra demonstrate that the third gender is far from problematic in achieving nirvana. Therefore, this research paper will strive to look at why the third gender is discriminated against in Buddhism despite its relationship to scriptures and achieving enlightenment. First it will focus on Buddhist sutras and then extend into medical texts that are relevant within Buddhist origins and finish by leading into how the transgender being is accepted socially in the sangha. By looking at both doctrines and medical texts one will be able to see the relevancy of the body both scripturally and medically and thus begin to understand it culturally within modern day religious law and societal acceptance. -

September 2019 New Releases
September 2019 New Releases what’s inside featured exclusives PAGE 3 RUSH Releases Vinyl Available Immediately! 72 Vinyl Audio 3 CD Audio 13 FEATURED RELEASES SUBHUMANS - KMFDM - FIDDLER ON THE ROOF: CRISIS POINT PARADISE 2018 CAST ALBUM Music Video DVD & Blu-ray 45 Non-Music Video DVD & Blu-ray 49 Order Form 75 Deletions and Price Changes 78 800.888.0486 THE HILLS HAVE EYES 2 NOIR ARCHIVE VOLUME TO HELL AND BACK: 203 Windsor Rd., Pottstown, PA 19464 [LIMITED EDITION] 3: 1957-1960 (9-FILM THE KANE HODDER SUBHUMANS - DEIDRE & THE DARK - KMFDM - www.MVDb2b.com COLLECTION) STORY CRISIS POINT VARIETY HOUR PARADISE HILLS HAVE EYES 2, SEE YOU IN SEPTEMBER! THE HILLS HAVE EYES 2, Wes Craven’s 1984 follow up to his classic original 1977 film, finds the lone survivor of a cannibal tribe detouring a motocross team across the desert straight into a pack of devouring ogres! The Hills are alive with the sound of screaming! From ARROW VIDEO, THE HILLS HAVE EYES 2 bluray is packed with extras that includes a limited edition 40-page book. If blinding horror is what you’re Craven, then this sequel delivers the goods! THE HILLS HAVE EYES 2 will see you in September, and the ogres will sing ‘Bye-bye, so long, farewell!’ Priests who are able to turn into dinosaurs may be an overused theme in film (!) but nobody does it better than WILD EYE films! THE VELOCIPASTOR DVD and bluray finds a despondent priest moving to China to find himself, only to find he can turn into a giant dinosaur. -

Contemporary Institutional and Popular Frameworks for Gender Variance
Georgia State University ScholarWorks @ Georgia State University Anthropology Theses Department of Anthropology 4-21-2010 "They Need Labels": Contemporary Institutional and Popular Frameworks for Gender Variance Ophelia Bradley Georgia State University Follow this and additional works at: https://scholarworks.gsu.edu/anthro_theses Recommended Citation Bradley, Ophelia, ""They Need Labels": Contemporary Institutional and Popular Frameworks for Gender Variance." Thesis, Georgia State University, 2010. https://scholarworks.gsu.edu/anthro_theses/35 This Thesis is brought to you for free and open access by the Department of Anthropology at ScholarWorks @ Georgia State University. It has been accepted for inclusion in Anthropology Theses by an authorized administrator of ScholarWorks @ Georgia State University. For more information, please contact [email protected]. “THEY NEED LABELS”: CONTEMPORARY INSTITUTIONAL AND POPULAR FRAMEWORKS FOR GENDER VARIANCE by OPHELIA D. BRADLEY Under the Direction of Dr. Jennifer Patico ABSTRACT This study addresses the complex issues of etiology and conceptualization of gender variance in the modern West. By analyzing medical, psychological, and popular approaches to gender variance, I demonstrate the highly political nature of each of these paradigms and how gender variant individuals engage with these discourses in the elaboration of their own gender identities. I focus on the role of institutional authority in shaping popular ideas about gender variance and the relationship of gender variant individuals who seek medical intervention towards the systems that regulate their care. Also relevant are the tensions between those who view gender variance as an expression of an essential cross-sex gender (as in traditional transsexual narrative) and those who believe that gender is socially constructed and non-binary. -

Gender and SEXUALITY “DISORDERS” and Alexandre Baril and Kathryn Trevenen Sexuality University of Ottawa, Canada Abstract
Annual Review EXPLORING ABLEISM AND of Critical Psychology 11, 2014 CISNORMATIVITY IN THE CONCEPTUALIZATION OF IDENTITY Gender AND SEXUALITY “DISORDERS” and Alexandre Baril and Kathryn Trevenen Sexuality University of Ottawa, Canada Abstract This article explores different conceptualizations of, and debates about, Body Integrity Identity Disorder and Gender Identity Disorder to first examine how these “identity disorders” have been both linked to and distinguished from, the “sexual disorders” of apotemnophilia (the de- sire to amputate healthy limbs) and autogynephilia (the desire to per- ceive oneself as a woman). We argue that distinctions between identity disorders and sexual disorders or paraphilias reflect a troubling hier- archy in medical, social and political discourses between “legitimate” desires to transition or modify bodies (those based in identity claims) and “illegitimate” desires (those based in sexual desire or sexuality). This article secondly and more broadly explores how this hierarchy between “identity troubles” and paraphilias is rooted in a sex-negative, ableist, and cisnormative society, that makes it extremely difficult for activists, individuals, medical professionals, ethicists and anyone else, to conceptualize or understand the desires that some people express around transforming their bodies—whether the transformation relates to sex, gender or ability. We argue that instead of seeking to “explain” these desires in ways that further pathologize the people articulating them, we need to challenge the ableism and cisnormativity that require explanations for some bodies, subjectivities and desires while leaving dominant normative bodies and subjectivities intact. We thus end the article by exploring possibilities for forging connections between trans studies and critical disability studies that would open up options for listening and responding to the claims of transabled people. -

Transfeminine Disruptions of Feminist Progress
Georgia State University ScholarWorks @ Georgia State University Anthropology Theses Department of Anthropology 5-10-2019 Necrotic Machines/Zombie Genders: Transfeminine Disruptions of Feminist Progress Alexandra Chace Georgia State University Follow this and additional works at: https://scholarworks.gsu.edu/anthro_theses Recommended Citation Chace, Alexandra, "Necrotic Machines/Zombie Genders: Transfeminine Disruptions of Feminist Progress." Thesis, Georgia State University, 2019. https://scholarworks.gsu.edu/anthro_theses/141 This Thesis is brought to you for free and open access by the Department of Anthropology at ScholarWorks @ Georgia State University. It has been accepted for inclusion in Anthropology Theses by an authorized administrator of ScholarWorks @ Georgia State University. For more information, please contact [email protected]. NECROTIC MACHINES/ZOMBIE GENDERS: TRANSFEMININE DISRUPTIONS OF FEMINIST PROGRESS by ALEXANDRA CHACE Under the Direction of Cassandra White, Ph.D. ABSTRACT Predominant narratives of trans womanhood—from biomedical sources, Feminist depictions, and film representations—typically present trans women as monstrous and antagonistic to normative cisgender society. Accordingly, this thesis traces this opposi- tional frame to the roots of ’trans’ as a cultural category, through 20th century biomedi- cal discourses, Feminist conceptions of trans woman identity, and horror films in order to better understand the contemporary proliferation of antipathy and violence towards transgender women. In so doing, this thesis revisits trans exclusionary theorists such as Mary Daly and Janice Raymond, developing Daly’s concept of ’robotitude’ into a notion of transitory ’necrosis’, positing the zombie as a moving post-human model for map- ping anti-trans violence and transphobia in regard to becoming-trans. This thesis further argues for trans identity not as a stable ontology, but as a hauntological trajectory of be- coming in which trans lives are rendered illegible and occluded. -

LGBTQIA+ Allyship at IMSA
The Illinois Mathematics and Science Academy LGBTQIA+ Allyship at IMSA Safe Zone Participant Guide WHAT IS A SAFE ZONE? A SafeZone or a safe space is a confidential place where all people can bring their authentic selves and feel safe, welcome and included. It may be a classroom, an office or an entire institution. Creating safe zones or safe spaces is a proactive step that schools, agencies and corporations can take to create welcoming, inclusive spaces so that all people are empowered to reach their full potential. The LGBTQIA+ SafeZone programs aim to increase the awareness, knowledge, and skills for individuals and address the challenges that exist when one wants to advocate for their LGBTQIA+ peers, family members, friends, coworkers and for themselves. LGBTQIA+ Facts and Stats 2 According to the CDC 2015 Youth Risk Behavior Survey, of surveyed LGB students: ¬ Were 140% (12% v. 5%) more likely to not go to school at least one day during the 30 days prior to the survey because of safety concerns, compared with heterosexual students. ¬ 10% were threatened or injured with a weapon on school property. ¬ 34% were bullied on school property. ¬ 28% were bullied electronically. ¬ 23% of LGB students who dated/went out with someone during the 12 months before the survey experienced sexual dating violence in the prior year. ¬ 18% of LGB students had experienced physical dating violence. ¬ 18% of LGB students had been forced to have sexual intercourse at some point in their lives. ¬ 95% of LGBTQ youth report they have trouble getting to sleep at night. LGB youth are at greater risk for depression, suicide, substance use, and sexual behaviors that can place them at increased risk for HIV and other sexually transmitted diseases (STDs). -

In Transition: Analyzing Shifting and Competing Anglophone Discourses
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Saskatchewan's Research Archive In Transition: Analyzing Shifting and Competing Anglophone Discourses Impacting Canadian Trans People A thesis submitted to the College of Graduate and Postdoctoral Studies in partial fulfillment of the requirements for the Degree of Master of Arts in the Department of Psychology, University of Saskatchewan, Saskatoon, Saskatchewan By Maaya Kuri Hitomi Copyright Maaya Kuri Hitomi, June/2018. All rights reserved Permission of use In presenting this thesis in partial fulfillment of the requirements for a Postgraduate degree from the University of Saskatchewan, I agree that the Libraries of this University may make it freely available for inspection. I further agree that permission for copying of this thesis in any manner, in whole or in part, for scholarly purposes may be granted by the professor or professors who supervised my thesis work or, in their absence, by the Head of the Department or the Dean of the College in which my thesis work was done. It is understood that any copying or publication or use of this thesis/dissertation or parts thereof for financial gain shall not be allowed without my written permission. It is also understood that due recognition shall be given to me and to the University of Saskatchewan in any scholarly use which may be made of any material in my thesis. Head of the Psychology Department 154 Arts, 9 Campus Drive Saskatoon, Saskatchewan, S7N 5A5 Canada OR Dean College of Graduate and Postdoctoral Studies University of Saskatchewan 116 Thorvaldson Building, 110 Science Place Saskatoon, Saskatchewan, S7N 5C9 Canada i Abstract Medical, community, and academic discourses offer competing interpretations of sex, gender, and the complexities of trans experiences, with variable attention to trans contributions to social and political thought and practice. -

Rutgers Journal of Sociology Knowledge in Contention Volume II, 2018
RJS The Rutgers Journal of Sociology Knowledge in Contention Volume II, 2018 Rutgers, The State University of New Jersey, New Brunswick Copyright ©2018, Graduate Program in Sociology About RJS The Rutgers Journal of Sociology: Emerging Areas in Sociological Inquiry provides a forum for graduate students and junior faculty to present well-researched and theoretically compelling review articles on an annual topic in sociology. Each volume features comprehensive commentary on emerging areas of sociological interest. These are critical evaluations of current research synthesized into cohesive ar- ticles about the state of the art in the discipline. Works that highlight the cutting edge of the field, either in terms of theoretical, method- ological, or topical areas, are privileged. Editors: Jorie Hofstra, Rutgers University Kathryn Burrows, Rutgers University CONTENTS | Knowledge in Contention EDITORS’ NOTE Jorie Hofstra, Kathryn Burrows 1 Papers POWER IN THE PRODUCTION OF TRANSGENDER KNOWLEDGE: THE CONTROVERSY OVER THE MAN WHO WOULD BE QUEEN Elroi J. Windsor, University of West Georgia 2 MARITAL WARRIORS? PRODUCING KNOWLEDGE TO DEFLECT CONTROVERSY IN MARRIAGE PROMOTION EFFORTS Melanie Heath, McMaster University 38 AGING AS DISEASE: HOW RADICAL VIEWS ON LONGEVITY EXPOSE UNEXAMINED ASSUMPTIONS IN MAINSTREAM THEORY ON SUCCESSFUL AGING Maoz Brown, University of Chicago 70 EDITORS’ INTRODUCTION JORIE HOFSTRA KATHRYN BURROWS his volume of The Rutgers Journal of Sociology addresses the Ttheme of Knowledge in Contention. The authors included in this volume approach the theme from different angles. In “Power in the Production of Transgender Knowledge: The Controversy over The Man Who Would Be Queen,” Elroi J. Windsor argues, through close analysis of a public controversy over ways of know- ing about transgender people, for the importance of positional- ity to the production of knowledge of marginalized populations. -
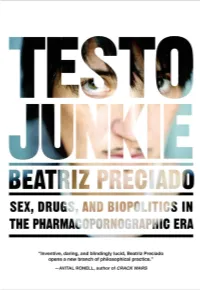
Testo Junkie Is a Key Text to Comprehend the Deep Interconnectedness of Sex and Drugs Today.”
“ Testo Junkie is a wild ride. Preciado leaves the identity politics of taking T to others, and instead, in the tradition of William S. Burroughs, Kathy Acker, and Jean Genet, s/he conducts a wild textual experiment. The results are spectacular . The gendered body will never be the same again.” —JACK HALBERSTAM, author of THE QUEER ART OF FAILURE “ Beatriz Preciado’s brilliant book oscillates between high theory and the surging rush of testosterone. Flush with elegant theoretical formulations, lascivious sex nar- ratives, and astute histories of gender, Testo Junkie is a key text to comprehend the deep interconnectedness of sex and drugs today.” —JOSÉ ESTEBAN MUÑOZ, author of CRUISING UTOPIA “The ideas in Beatriz Preciado’s pornosophical gem are a thousand curious fingers slipped beneath the underpants of conventional thinking. Teach the sex scenes in your seminars, and read the flights of theory aloud to your latest lover amid a tangle of sweaty sheets.” —SUSAN STRYKER, author of THE TRANSGENDER STUDIES READER “ Testo Junkie is unlike anything I’ve ever read. Beatriz Preciado has produced a volume of work that goes far beyond memoir to create an entirely new way of understanding not only the history of sex, gender, and the body, but of life as we have come to know it. Powerful and disturbing in the most pleasurable way.” —DEL LAGRACE VOLCANO, author of FEMMES OF POWER “ Beatriz Preciado offers an exhilarating and sometimes shattering portrait of how gen- dershapesthewaysweliveandfuckandgrieveandfightandlove.Testo Junkie is a fearless chronicle of the gender revolution currently in progress. Anyone who has a gender—or has dispensed with one—should read this book.” —GAYLE SALAMON, author of ASSUMING A BODY “ Inventive, daring, and blindingly lucid, Beatriz Preciado opens a new branch of phil- osophical practice.