Characterization and Targeting of Malignant Stem Cells in Patients with Advanced Myelodysplastic Syndromes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Prospective, Multicenter, Phase-II Trial of Ibrutinib Plus Venetoclax In
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 A prospective, multicenter, phase-II trial of ibrutinib plus venetoclax in patients with creatinine clearance ≥ 30 ml/min who have relapsed or refractory chronic lymphocytic leukemia (RR-CLL) with or without TP53 aberrations HOVON 141 CLL / VIsion Trial of the HOVON and Nordic CLL study groups PROTOCOL Principal Investigator : Arnon P Kater (HOVON) Carsten U Niemann (Nordic CLL study Group)) Sponsor : HOVON EudraCT number : 2016-002599-29 ; Page 1 of 107 Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 LOCAL INVESTIGATOR SIGNATURE PAGE Local site name: Signature of Local Investigator Date Printed Name of Local Investigator By my signature, I agree to personally supervise the conduct of this study in my affiliation and to ensure its conduct in compliance with the protocol, informed consent, IRB/EC procedures, the Declaration of Helsinki, ICH Good Clinical Practices guideline, the EU directive Good Clinical Practice (2001-20-EG), and local regulations governing the conduct of clinical studies. -

214120Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 214120Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number NDA 214120 Application Type Type 3 Priority or Standard Priority Submit Date 3/3/2020 Received Date 3/3/2020 PDUFA Goal Date 9/3/2020 Office/Division OOD/DHM1 Review Completion Date 9/1/2020 Applicant Celgene Corporation Established Name Azacitidine (Proposed) Trade Name Onureg Pharmacologic Class Nucleoside metabolic inhibitor Formulations Tablet (200 mg, 300 mg) (b) (4) Applicant Proposed Indication/Population Recommendation on Regulatory Regular approval Action Recommended Indication/ For continued treatment of adult patients with acute Population myeloid leukemia who achieved first complete remission (CR) or complete remission with incomplete blood count recovery (CRi) following intensive induction chemotherapy and are not able to complete intensive curative therapy. SNOMED CT for the Recommended 91861009 Indication/Population Recommended Dosing Regimen 300 mg orally daily on Days 1 through 14 of each 28-day cycle Reference ID: 4664570 NDA Multidisciplinary Review and Evaluation NDA 214120 Onureg (azacitidine tablets) TABLE OF CONTENTS TABLE OF CONTENTS ................................................................................................................................... 2 TABLE OF TABLES ....................................................................................................................................... -

Intravesical Instillation of Azacitidine Suppresses Tumor Formation Through TNF-R1 and TRAIL-R2 Signaling in Genotoxic Carcinogen-Induced Bladder Cancer
cancers Article Intravesical Instillation of Azacitidine Suppresses Tumor Formation through TNF-R1 and TRAIL-R2 Signaling in Genotoxic Carcinogen-Induced Bladder Cancer Shao-Chuan Wang 1,2,3, Ya-Chuan Chang 2, Min-You Wu 2, Chia-Ying Yu 2, Sung-Lang Chen 1,2,3 and Wen-Wei Sung 1,2,3,* 1 Department of Urology, Chung Shan Medical University Hospital, Taichung 40201, Taiwan; [email protected] (S.-C.W.); [email protected] (S.-L.C.) 2 School of Medicine, Chung Shan Medical University, Taichung 40201, Taiwan; [email protected] (Y.-C.C.); [email protected] (M.-Y.W.); [email protected] (C.-Y.Y.) 3 Institute of Medicine, Chung Shan Medical University, Taichung 40201, Taiwan * Correspondence: [email protected] or fl[email protected]; Tel.: +886-4-2473-9595 Simple Summary: Approximately 70% of all bladder cancer is diagnosed as non-muscle invasive bladder cancer and can be treated by transurethral resection of the bladder tumor, followed by intravesical instillation chemotherapy. Bacille Calmette-Guérin (BCG) is the first-line agent for intravesical instillation, but its accessibility has been limited for years due to a BCG shortage. Here, our aim was to evaluate the therapeutic role of intravesical instillation of azacitidine, a DNA methyltransferase inhibitor, in bladder cancer. Cell model experiments showed that azacitidine inhibited TNFR1 downstream pathways to downregulate HIF-1α, claspin, and survivin. Concomitant Citation: Wang, S.-C.; Chang, Y.-C.; upregulation of the TRAIL R2 pathway by azacitidine ultimately drove the tumor cells to apoptosis. Wu, M.-Y.; Yu, C.-Y.; Chen, S.-L.; Sung, Rats with genotoxic carcinogen-induced bladder cancer showed a significantly reduced in vivo tumor W.-W. -

The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia
International Journal of Molecular Sciences Review The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia Marta Weronika Lato 1 , Anna Przysucha 1, Sylwia Grosman 1, Joanna Zawitkowska 2 and Monika Lejman 3,* 1 Student Scientific Society, Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] (M.W.L.); [email protected] (A.P.); [email protected] (S.G.) 2 Department of Pediatric Hematology, Oncology and Transplantology, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 3 Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland * Correspondence: [email protected] Abstract: Childhood acute lymphoblastic leukemia is a genetically heterogeneous cancer that ac- counts for 10–15% of T-cell acute lymphoblastic leukemia (T-ALL) cases. The T-ALL event-free survival rate (EFS) is 85%. The evaluation of structural and numerical chromosomal changes is important for a comprehensive biological characterization of T-ALL, but there are currently no ge- netic prognostic markers. Despite chemotherapy regimens, steroids, and allogeneic transplantation, relapse is the main problem in children with T-ALL. Due to the development of high-throughput molecular methods, the ability to define subgroups of T-ALL has significantly improved in the last few years. The profiling of the gene expression of T-ALL has led to the identification of T-ALL subgroups, and it is important in determining prognostic factors and choosing an appropriate treatment. Novel therapies targeting molecular aberrations offer promise in achieving better first remission with the Citation: Lato, M.W.; Przysucha, A.; hope of preventing relapse. -

LEUKEMIA CHEMOTHERAPY REGIMENS (Part 1 of 2) the Selection, Dosing, and Administration of Anti-Cancer Agents and the Management of Associated Toxicities Are Complex
LEUKEMIA CHEMOTHERAPY REGIMENS (Part 1 of 2) The selection, dosing, and administration of anti-cancer agents and the management of associated toxicities are complex. Drug dose modifications and schedule and initiation of supportive care interventions are often necessary because of expected toxicities and because of individual patient variability, prior treatment, and comorbidities. Thus, the optimal delivery of anti-cancer agents requires a healthcare delivery team experienced in the use of such agents and the management of associated toxicities in patients with cancer. The chemotherapy regimens below may include both FDA-approved and unapproved uses/regimens and are provided as references only to the latest treatment strategies. Clinicians must choose and verify treatment options based on the individual patient. REGIMEN DOSING Acute Myeloid Leukemia (AML) Induction Therapy Cytarabine (Cytosar-U; ARA-C) + Days 1–3: An anthracycline (eg, daunorubicin at least 60mg/m2/day IV, an anthracycline idarubicin 10–12mg/m2/day IV, or mitoxantrone 10–12mg/m2/day IV), plus (daunorubicin [Cerubidine], Days 1–7: Cytarabine 100–200mg/m2/day continuous IV infusion. idarubicin [Idamycin], OR mitoxantrone [Novantrone])1, 2 Days 1–3: An anthracycline (eg, daunorubicin 45mg/m2/day IV, idarubicin 12mg/m2/day IV, or mitoxantrone 12mg/m2/day IV), plus Days 1–7: Cytarabine 100mg/m2/day continuous IV infusion. Intermediate-dose cytarabine3 Cycle 1 Days 1–7: Cytarabine 200mg/m2/day continuous IV infusion, plus Days 5–6: Idarubicin 12mg/m2/day IV. Cycle 2 Days 1–6: Cytarabine 1,000mg/m2 continuous IV infusion for 3 hrs twice daily, plus Days 3, 5 and 7: Amsacrine 120mg/m2/day. -

Vidaza, INN-Azacitidine
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Vidaza 25 mg/ml powder for suspension for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each vial contains 100 mg azacitidine. After reconstitution, each ml suspension contains 25 mg azacitidine. For a full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Powder for suspension for injection. White lyophilised powder. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Vidaza is indicated for the treatment of adult patients who are not eligible for haematopoietic stem cell transplantation with: • intermediate-2 and high-risk myelodysplastic syndromes (MDS) according to the International Prognostic Scoring System (IPSS), • chronic myelomonocytic leukaemia (CMML) with 10-29 % marrow blasts without myeloproliferative disorder, • acute myeloid leukaemia (AML) with 20-30 % blasts and multi-lineage dysplasia, according to World Health Organisation (WHO) classification. 4.2 Posology and method of administration Vidaza treatment should be initiated and monitored under the supervision of a physician experienced in the use of chemotherapeutic agents. Patients should be premedicated with anti-emetics for nausea and vomiting. Posology The recommended starting dose for the first treatment cycle, for all patients regardless of baseline haematology laboratory values, is 75 mg/m2 of body surface area, injected subcutaneously, daily for 7 days, followed by a rest period of 21 days (28-day treatment cycle). It is recommended that patients be treated for a minimum of 6 cycles. Treatment should be continued as long as the patient continues to benefit or until disease progression. Patients should be monitored for haematologic response/toxicity and renal toxicities (see section 4.4); a delay in starting the next cycle or a dose reduction as described below may be necessary. -
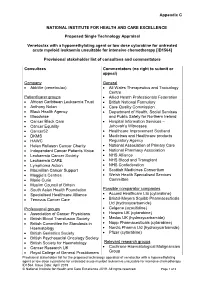
Draft Matrix Post Referral PDF 189 KB
Appendix C NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Proposed Single Technology Appraisal Venetoclax with a hypomethylating agent or low dose cytarabine for untreated acute myeloid leukaemia unsuitable for intensive chemotherapy [ID1564] Provisional stakeholder list of consultees and commentators Consultees Commentators (no right to submit or appeal) Company General • AbbVie (venetoclax) • All Wales Therapeutics and Toxicology Centre Patient/carer groups • Allied Health Professionals Federation • African Caribbean Leukaemia Trust • British National Formulary • Anthony Nolan • Care Quality Commission • Black Health Agency • Department of Health, Social Services • Bloodwise and Public Safety for Northern Ireland • Cancer Black Care • Hospital Information Services – • Cancer Equality Jehovah’s Witnesses • Cancer52 • Healthcare Improvement Scotland • DKMS • Medicines and Healthcare products • HAWC Regulatory Agency • Helen Rollason Cancer Charity • National Association of Primary Care • Independent Cancer Patients Voice • National Pharmacy Association • Leukaemia Cancer Society • NHS Alliance • Leukaemia CARE • NHS Blood and Transplant • Lymphoma Action • NHS Confederation • Macmillan Cancer Support • Scottish Medicines Consortium • Maggie’s Centres • Welsh Health Specialised Services • Marie Curie Committee • Muslim Council of Britain • South Asian Health Foundation Possible comparator companies • Specialised Healthcare Alliance • Accord Healthcare Ltd (cytarabine) • Tenovus Cancer Care • Bristol-Meyers Squibb Pharmaceuticals Ltd -

A Novel CDK9 Inhibitor Increases the Efficacy of Venetoclax (ABT-199) in Multiple Models of Hematologic Malignancies
Leukemia (2020) 34:1646–1657 https://doi.org/10.1038/s41375-019-0652-0 ARTICLE Molecular targets for therapy A novel CDK9 inhibitor increases the efficacy of venetoclax (ABT-199) in multiple models of hematologic malignancies 1 1 2,3 4 1 5 6 Darren C. Phillips ● Sha Jin ● Gareth P. Gregory ● Qi Zhang ● John Xue ● Xiaoxian Zhao ● Jun Chen ● 1 1 1 1 1 1 Yunsong Tong ● Haichao Zhang ● Morey Smith ● Stephen K. Tahir ● Rick F. Clark ● Thomas D. Penning ● 2,7 3 5 1 4 2,7 Jennifer R. Devlin ● Jake Shortt ● Eric D. Hsi ● Daniel H. Albert ● Marina Konopleva ● Ricky W. Johnstone ● 8 1 Joel D. Leverson ● Andrew J. Souers Received: 27 November 2018 / Revised: 18 October 2019 / Accepted: 13 November 2019 / Published online: 11 December 2019 © The Author(s) 2019 Abstract MCL-1 is one of the most frequently amplified genes in cancer, facilitating tumor initiation and maintenance and enabling resistance to anti-tumorigenic agents including the BCL-2 selective inhibitor venetoclax. The expression of MCL-1 is maintained via P-TEFb-mediated transcription, where the kinase CDK9 is a critical component. Consequently, we developed a series of potent small-molecule inhibitors of CDK9, exemplified by the orally active A-1592668, with CDK selectivity profiles 1234567890();,: 1234567890();,: that are distinct from related molecules that have been extensively studied clinically. Short-term treatment with A-1592668 rapidly downregulates RNA pol-II (Ser 2) phosphorylation resulting in the loss of MCL-1 protein and apoptosis in MCL-1- dependent hematologic tumor cell lines. This cell death could be attenuated by either inhibiting caspases or overexpressing BCL-2 protein. -

Plenary and Platform Abstracts
American Society of Human Genetics 68th Annual Meeting PLENARY AND PLATFORM ABSTRACTS Abstract #'s Tuesday, October 16, 5:30-6:50 pm: 4. Featured Plenary Abstract Session I Hall C #1-#4 Wednesday, October 17, 9:00-10:00 am, Concurrent Platform Session A: 6. Variant Insights from Large Population Datasets Ballroom 20A #5-#8 7. GWAS in Combined Cancer Phenotypes Ballroom 20BC #9-#12 8. Genome-wide Epigenomics and Non-coding Variants Ballroom 20D #13-#16 9. Clonal Mosaicism in Cancer, Alzheimer's Disease, and Healthy Room 6A #17-#20 Tissue 10. Genetics of Behavioral Traits and Diseases Room 6B #21-#24 11. New Frontiers in Computational Genomics Room 6C #25-#28 12. Bone and Muscle: Identifying Causal Genes Room 6D #29-#32 13. Precision Medicine Initiatives: Outcomes and Lessons Learned Room 6E #33-#36 14. Environmental Exposures in Human Traits Room 6F #37-#40 Wednesday, October 17, 4:15-5:45 pm, Concurrent Platform Session B: 24. Variant Interpretation Practices and Resources Ballroom 20A #41-#46 25. Integrated Variant Analysis in Cancer Genomics Ballroom 20BC #47-#52 26. Gene Discovery and Functional Models of Neurological Disorders Ballroom 20D #53-#58 27. Whole Exome and Whole Genome Associations Room 6A #59-#64 28. Sequencing-based Diagnostics for Newborns and Infants Room 6B #65-#70 29. Omics Studies in Alzheimer's Disease Room 6C #71-#76 30. Cardiac, Valvular, and Vascular Disorders Room 6D #77-#82 31. Natural Selection and Human Phenotypes Room 6E #83-#88 32. Genetics of Cardiometabolic Traits Room 6F #89-#94 Wednesday, October 17, 6:00-7:00 pm, Concurrent Platform Session C: 33. -

High Expression of an Unknown Long Noncoding RNA RP11-290L1.3 from GDM Macrosomia and Its Effect on Preadipocyte Differentiation
ID: 20-0584 10 2 Y Lin, Y Zhand, L Xu et al. RP11 enhanced preadipocyte 10:2 191–204 differentiation RESEARCH High expression of an unknown long noncoding RNA RP11-290L1.3 from GDM macrosomia and its effect on preadipocyte differentiation Yu Lin1,*, Yingying Zhang1,*, Lei Xu2,*, Wei Long1, Chunjian Shan1, Hongjuan Ding1, Lianghui You1, Chun Zhao1 and Zhonghua Shi1 1State Key Laboratory of Reproductive Medicine, Women’s Hospital of Nanjing Medical University, Nanjing Maternity and Child Health Care Hospital, Nanjing, People’s Republic of China 2Maternal and Child Health Care Hospital of Dongchangfu District, Liaocheng, People’s Republic of China Correspondence should be addressed to C Zhao or Z Shi: [email protected] or [email protected] *(Y Lin, Y Zhang and L Xu contributed equally to this work) Abstract Aims: Gestational diabetes mellitus (GDM)-induced macrosomia is predominantly Key Words characterized by fat accumulation, which is closely related to adipocyte differentiation. f long noncoding RNA An unknown long noncoding RNA RP11-290L1.3, referred to as RP11, was identified to f GDM be dramatically upregulated in the umbilical cord blood of women with GDM-induced f preadipocyte macrosomia in our previous study. We conducted this study to identify the function of differentiation RP11 in GDM-induced macrosomia. f macrosomia Methods: The effects of RP11 gain- and loss-of-function on HPA-v (human preadipocytes- f fat accumulation visceral) adipogenesis were determined with lentivirus mediated cell transduction. The mRNA and protein expression levels of adipogenesis makers were evaluated by qPCR/Western blot. Then, we performed the microarray and pathway analysis to explore the possible mechanisms by which RP11 regulates adipogenesis. -

Azacytidine Sensitizes Acute Myeloid Leukemia Cells to Arsenic Trioxide By
Chau et al. Journal of Hematology & Oncology (2015) 8:46 DOI 10.1186/s13045-015-0143-3 JOURNAL OF HEMATOLOGY & ONCOLOGY RESEARCH ARTICLE Open Access Azacytidine sensitizes acute myeloid leukemia cells to arsenic trioxide by up-regulating the arsenic transporter aquaglyceroporin 9 David Chau1†, Karen Ng1†, Thomas Sau-Yan Chan1, Yuen-Yee Cheng1,3, Bonnie Fong2, Sidney Tam2, Yok-Lam Kwong1 and Eric Tse1* Abstract Background: The therapeutic efficacy of arsenic trioxide (As2O3) in acute myeloid leukemia (AML) is modest, which is partly related to its limited intracellular uptake into the leukemic cells. As2O3 enters cells via the transmembrane protein aquaglyceroporin 9 (AQP9). Azacytidine, a demethylating agent that is approved for the treatment of AML, has been shown to have synergistic effect with As2O3. We tested the hypothesis that azacytidine might up-regulate AQP9 and enhances As2O3-mediated cytotoxicity in AML. Methods: Arsenic-induced cytotoxicity, the expression of AQP9, and the intracellular uptake of As2O3 were determined in AML cell lines and primary AML cells with or without azacytidine pre-treatment. The mechanism of AQP9 up-regulation was then investigated by examining the expression of transcription factors for AQP9 gene and the methylation status of their gene promoters. Results: As2O3-induced cytotoxicity in AML cell lines was significantly enhanced after azacytidine pre-treatment as a result of AQP9 up-regulation, leading to increased arsenic uptake and hence intracellular concentration. Blocking AQP9-mediated As2O3 uptake with mercury chloride abrogated the sensitization effect of azacytidine. AQP9 promoter does not contain CpG islands. Instead, azacytidine pre-treatment led to increased expression of HNF1A, a transcription activator of AQP9, through demethylation of HNF1A promoter. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase