Cooking with Care a Toolkit to Support Healthy Eating for Unpaid Older Carers Introduction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Skim Or 1% Milk Gallons
Lenten Seafood Specials See Page 3.. ® Skim or 1% Save 60¢ Milk Gallons ® No Artificial rBST Excellent Source 99Not Valid In The State Growth Hormones Of Calcium Of Maine. SEAFOOD Wild • All Natural 1 Ocean Fresh Swordfish Fresh Veal Cutlets Steaks Thin Sliced Cut Save $1.00lb. Fresh Hand Trimmed Daily Instore $ 99 99 Save 4.50lb. 10 lb. lb. DELI ® Provolone 7 Brown Sorrento or Is Now Sugar Galbani Mozzarella Ham Cheese Save$1.00lb. Save $1.50lb. Sliced Fresh 99 99 At The Deli 3 lb. lb. A Good Source 2 PRODUCE Of Vitamins A,C Florida & Iron Tender 2-LB. Sweet Fresh Green CONT. Asparagus Strawberries Save 70¢ Pasta Save$1.00lb. Save$4.98 •Tortellini 99 99 •Ravioli 8-12 oz. $ •Gnocchi PKG. 1 lb. 3 2 for4 6 PACK 6 PACK 25 Happy Baby Assorted Cuts •Original •Lemon Poland •Organic •Strawberry •Black Cherry Spring •Orange •Lime Whole Milk •Raspberry Lime Sparkling Yogurt Pasta Water Save $5.76 Sale $ Save$1.25 Save 2.00 $ 10 oz. 4for5 $ 16 PROGRESSO $ 16.9 oz. BTLS. for Varieties 16 oz. PKG. for VEGETABLE 5 5 2 3 ® CLASSICS Hearty Steamfresh SOUPS Corn Breads Save Up To $1.24 Save $5.00 Save $1.00 •Peas •Vegetables With Rice ¢ $ •12 Grain •Hearty Nut $ •Oat Nut •100% Wheat FROZEN 10 oz. PKG. 18.5-19 oz. CAN for •Soft Oatmeal 24 oz. for Happy88 Valentine’s5 5 Day2 3 ™ 4 Inch ™ ™ Stick Balloons ™ ™ ™ % ™ ™ ™ ™ 10 Off ™ ¢ ™ ™ Choose From 4 Styles EACH ™ ™ 99 ™ These Select ™ 18 Inch ™ ™ Standard Size ™ Gift Cards ™ ™ Red or Assorted Colors ™ ™ ONE DOZEN With Baby’s Breath & Greens ™ 99™ ™ Choose From 5 Styles EACH ™ Long ™ 1 ™ ™ BAKERY Valentine ™ ™ Cupcakes ™ Stem ™ ™ 99 •Vanilla •Chocolate ™ ™ Roses ™ ™ The Perfect Valentine Gift While supplies last. -

Milk 101 a Discussion on Dairy Fat
milk 101 a discussion on dairy fat There are many different types of milk sold at the grocery store and one difference between them is the amount of fat they contain. The percentages included in the names of milk indicate how much fat is in the milk by weight. The different varieties match the wide range of consumer preferences. MILK 4% milk (whole milk) has the richest, thickest and creamiest taste. 4% It contains about 160 calories and 9 grams of fat per cup. MILK 2% milk (reduced-fat milk) still has a creamy taste but less so than 2% whole milk. It contains about 125 calories and 5 grams of fat per cup. 1% milk (low-fat milk) has a much less creamy taste and a thinner MILK mouthfeel and appearance. It contains about 100 calories and 2.5 1% grams of fat per cup. Fat-free milk (nonfat or skim milk) has no more than 0.2% milk fat, MILK FAT-FREE resulting in the thinnest mouthfeel and appearance. It contains about 80 calories and less than 1 gram of fat per cup. dairy fat science Research supports that whole-milk dairy is just as healthful as lower-fat options, despite its higher fat content. A recent review of the existing research on whole-milk dairy consumption published in the European Journal of Nutrition found that people who eat full-fat dairy are not more likely to develop cardiovascular disease and type 2 diabetes than people who stick to low-fat dairy. Additionally, in 11 of the 16 studies included in the review, people who consumed more high-fat dairy products either weighed less or gained less weight over time. -
ACE Appendix
CBP and Trade Automated Interface Requirements Appendix: PGA August 13, 2021 Pub # 0875-0419 Contents Table of Changes .................................................................................................................................................... 4 PG01 – Agency Program Codes ........................................................................................................................... 18 PG01 – Government Agency Processing Codes ................................................................................................... 22 PG01 – Electronic Image Submitted Codes .......................................................................................................... 26 PG01 – Globally Unique Product Identification Code Qualifiers ........................................................................ 26 PG01 – Correction Indicators* ............................................................................................................................. 26 PG02 – Product Code Qualifiers ........................................................................................................................... 28 PG04 – Units of Measure ...................................................................................................................................... 30 PG05 – Scientific Species Code ........................................................................................................................... 31 PG05 – FWS Wildlife Description Codes ........................................................................................................... -
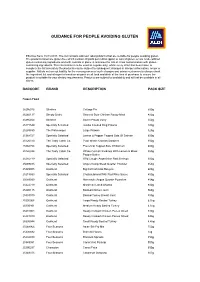
Guidance for People Avoiding Gluten
GUIDANCE FOR PEOPLE AVOIDING GLUTEN Effective from: 15/11/2017. The list contains Aldi own label products that are suitable for people avoiding gluten. The products listed are gluten free which contain 20 parts per million (ppm) or less of gluten, or are made without gluten-containing ingredients and with controls in place to minimise the risk of cross contamination with gluten- containing ingredients. This information is to be used as a guide only; whilst every effort has been taken to complete the list accurately the products may be subject to subsequent changes in allergen information, recipe or supplier. Aldi do not accept liability for the consequences of such changes and advise customers to always check the ingredient list and allergen information on pack on all food and drink at the time of purchase to ensure the product is suitable for your dietary requirements. Products are subject to availability and will not be available in all stores. BARCODE BRAND DESCRIPTION PACK SIZE Frozen Food 25295016 Slimfree Cottage Pie 500g 25260137 Simply Bistro Sweet & Sour Chicken Ready Meal 400g 25295054 Slimfree Sweet Potato Curry 550g 25171549 Specially Selected Jumbo Cooked King Prawns 180g 25288650 The Fishmonger Large Prawns 325g 25368727 Specially Selected Lemon & Pepper Topped Side Of Salmon 600g 25126310 The Tasty Catch Co. Plain Whole Cornish Sardines 350g 25368758 Specially Selected Provencal Topped Side Of Salmon 600g 25126334 The Tasty Catch Co. Whole Cornish Sardines With Lemon & Black 350g Pepper Butter 25282719 Specially Selected -

Ready for a Skyr Game Changer? Ready for a Skyr Game Changer?
INTERNATIONAL May 2020 PROCESSING INGREDIENTS PACKAGING IT LOGISTICS www.international-dairy.com Ready for a skyr game changer? Ready for a skyr game changer? Would you like to produce a skyr with a superior in-mouth experience on your separator processing line? At Arla Foods Ingredients, we have developed Nutrilac® YO-4575 which allows you to produce skyr effi ciently on your separator processing line. Based on natural whey proteins, our tailored ingredient delivers a delicious mouthfeel, texture and taste time aft er time. Editorial ¦ IDM Months are lost World dairy trade will continue to suffer At the moment this commentary is being written, everything revolves around how the world, people and, above all, economy can return to normal life from the rigidity of pandemic con- tainment without causing further damage. A further lockdown, which would undoubtedly be imposed if the infection figures were to flare up again, would in all probability be the death knell for large parts of industry and the economy. But even so, there will be enormous upheavals when the world awakens from isolation. The threat of millions of jobs being lost or already lost will not exactly encourage people to spend money. People will have to economize on consumption and, by force, on every- thing else. In addition, global milk exports will fall, because the oil-producing countries in Roland Sossna particular are short of money due to the drop in oil prices and will be unable to act develop Editor IDM significant demand for the time being. International Dairy Magazine [email protected] Incidentally, milk processors are affected by the pandemic in very different ways. -

Download the Guide
ONTARIO 2021 DAIRY GUIDE ONTARIO DAIRY GUIDE 1 Whether crafted by hand or at scale, Ontario dairy products are all inspired by a single delicious, sustainable and local ingredient: EVERYDAY MILK… DID YOU KNOW? • As a result of continuous investments in sustainability LOCAL MILK WHOLE MILK and production practices, 65% fewer cows produce Barista milk! Whole (3.25% milk fat) milk is lighter than cream but the same volume of milk needed to nourish all of Producing the fresh, local milk that elevates an incredible range of high-quality adds a luxurious smoothness to coffee beverages and dishes. Canada as compared with 50 years ago. Ontario dairy products is a tradition based on the values that have shaped dairy LOCAL MILK LOCAL farming for generations. While the know-how and craft have been preserved, the PARTLY-SKIMMED & SKIMMED MILK • It takes the same amount of land resources quality and potential of the ingredient has grown and evolved, making Ontario one Partly-skimmed (1-2% milk fat) milk perfectly versatile, used in (about 1.7 square metres) to produce either a litre of the most unique dairy regions in the country and around the world. baking, cooking or enjoyed on its own. Skimmed milk (0.1% milk fat) of milk or a loaf of bread. is nearly fat-free and extremely refreshing. • A single serving of milk contains more absorbable BUTTERMILK calcium than any other natural food. LOCAL BY NATURE. Perfected. Pasteurization eliminates bacteria and The inimitable tanginess of buttermilk is the result of a specialized Milk is a hyper local food, travelling from the farm to grocery homogenization ensures a smooth and consistent milk bacterial culture added to regular milk. -

Yogurt Consumption & Improved Lactose Digestion
Yogurt Consumption & Improved Lactose Digestion Yogurt, kefir and other fermented foods contain health promoting bacteria that influence the gut microbe and contribute to overall health.1 A systematic review published in Nutrition Reviews2 evaluated the impact of fermented dairy food consumption, specifically yogurt, kefir and other fermented milks, on gastrointestinal and cardiovascular health, cancer risk, weight management, diabetes and metabolic health, and bone density.* Among the positive findings, a direct and causal relationship was found between yogurt consumption and lactose digestion and tolerance. This review affirms the beneficial role of yogurt consumption on improved lactose digestion and tolerance. * The review included 47 clinical trials, 6 case control trials, 16 cross-sectional studies and 39 prospective studies (108 studies in total) published between 1979 and 2017. Fermented milk consumption was also consistently associated with: • Reduced risk of breast & colorectal cancer • Reduced risk of type 2 diabetes • Improved weight maintenance • Improved cardiovascular health • Improved bone health • Improved gastrointestinal health2 Did you know? • Yogurt provides 7 essential nutrients including: protein, calcium, phosphorus, vitamin B12, pantothenic acid, riboflavin & zinc.3 • The live and active cultures found in yogurt helps to break down lactose, which may make it easier for people with lactose intolerance to digest yogurt.3 • Fermented foods like yogurt are a good sources of nutrients that are important for normal immune function and may help reduce chronic inflammation.3 National Dairy Council’s (NDC) mission it to bring to life the dairy community’s shared vision of a healthy, happy, sustainable world with science as our foundation. On behalf of America’s dairy farmers and importers, NDC strives to help people thrive across the lifespan through science-based information on dairy’s contributions to nutrition, health and sustainable food systems. -

The Importance of (Dairy) Protein for Maintenance of Muscle Mass During Aging & Rehabilitation
The importance of (dairy) protein for maintenance of muscle mass during aging & rehabilitation METTE HANSEN, Associated Professor INSTITUTE OF PUBLIC HEALTH SECTION OF SPORT SCIENCE AARHUS UNIVERSITY DENMARK [email protected] AARHUS UNIVERSITY 2013 EU: THE PORPORTION OF ELDERLY GROW AARHUS UNIVERSITY 2013 SOCIETY: FOR HOW LONG CAN THEY REMAIN INDEPENDENT OF HELP ? $$$ INDIVIDUAL: CAN I DO WHAT I WANT TO DO? AARHUS UNIVERSITY 2013 DAILY ACTIVITIES WALKING STAIR CLIMBING CHAIR RISING Physical function of the muscle skeletal system › Flexibility › Coordination / balance › Muscle endurance capacity › Muscle strength › Muscle power Muscle mass & Neural factors AARHUS UNIVERSITY 2013 REDUCTION IN: STRENGTH MUSCLE MASS Reduced by 0.5-2% /yr from 50-80 yrs Reduced by 1-1.5% /yr from 60-65 yrs Muscle fiber Maximal Isometric strength Loss of muscle fiber Smaller muscle fiber Vandervoort & McComas 1986, Spirdoso 1995 Spirduso, Physical dimensions of Ageing, 1995 Parise & Yarasheski, Curr Opin Clin Nutr Metab Care, 2000 AARHUS UNIVERSITY 2013 MUSCLE PROTEIN BALANCE Muscle Muscle Synthesis Breakdown AARHUS UNIVERSITY 2013 MUSCLE PROTEIN BALANCE Immobilization & disease Muscle Muscle Synthesis Breakdown Reduced energy & protein intake AARHUS UNIVERSITY 2013 ELECTIVE ABDOMINAL SURGERY DEPRESSES MUSCLE PROTEIN SYNTHESIS AND ACCELERATE MUSCLE LOSS 21 days, n=13 Body weight ↓11.8 kg Fat free mass ↓11.5 kg Arm- & leg muscles ↓5.3 kg Heart muscle Dage Petersson et al 1990 AARHUS It is difficult for elderly patients to UNIVERSITY 2013 regain muscle strength -

Let's Make Some Skyr!
Ever had trouble keeping your skyr at the right temperature? Us too! To help you get that Let's make tangy skyr flavour we’ve worked with some skyr! designers and created a Mad Millie double- 1 2 5 6 walled, stainless steel Technically skyr is a cheese, however the way fermenting flask. it's eaten is more recognisable as a yoghurt. Heat the milk to 40oC Once milk is at Pour the Skyr into Pull the corners of the Whatever you want to call it, the culture rich (105oF). 40oC (105oF) a muslin cloth lined muslin cloth together This is the easiest way to product has the same great nutritional value. sprinkle in the culture. colander to drain and hang to drain the maintain temperatures When made well, Skyr is so thick and creamy, the whey. Skyr for 2 – 6 hours of 30 - 40ºC it won’t fall off an upside-down spoon! depending on preferred (86 - 105ºF) overnight thickness. and allow cultures to work their magic. ICELANDIC YOGURT (SKYR) Other options are a Prep time: 30 mins Ready in: 11 hours warmed up and turned Makes approx. 400 g (14 oz) off oven, a warm water bath or wrapping your Ingredients jar in towels and placing Store in the refrigerator for up to 2 weeks it in a warm spot. 1 L (1 US qt) of skim/low fat milk in a sealed container. 1 sachet Dairy Free Yoghurt Culture 3 4 1/2 tablet of vegetarian rennet diluted in 2 Tbsp (30 mL) of cool, Add your diluted rennet Maintain the milk at Enjoy your Skyr at breakfast, lunch or dinner. -
The Local Dairy Issue
FREE! SUMMER 2019 the local dairy issue IN THE SPOTLIGHT Larson Farm & Creamery BETWEEN THE ROWS Mighty Mulch THE DEEP DISH Real Organic Dairy FOOD FETISH Yogurt...Savoring the Sweetness of Sour Milk Mercy Larson Larson Farm and Creamery under the sun QUARTERLY SUMMER 2019 2 CO-OP CONVERSATIONS OPEN 8:00AM TO 7:00PM EVERYDAY A Letter From Glenn, GM 9 WASHINGTON STREET MIDDLEBURY, VERMONT (802)388-7276 middlebury.coop EVERYONE WELCOME! 3 A WORD FROM THE BOARD Meeting Satoyama WHY DOES THE CO-OP EXIST? 5 IN THE SPOTLIGHT The Co-op exists to help our member-owners Larson Farm & Creamery customers and the community benefit from: • HEALTHY FOODS BETWEEN THE ROWS • VIBRANT LOCAL ECONOMY 7 • ENVIRONMENTALLY SUSTAINABLE & Mighty Mulch ENERGY EFFICIENT PRACTICES • COOPERATIVE DEMOCRATIC OWNERSHIP 9 CENTERFOLD • LEARNING ABOUT THESE VALUES Economic Impact of Organic Dairy in VT WHAT IS OUR BUYING CRITERIA? Middlebury Natural Foods Co-op strives to select products that are local, organic, and free of: 11 THE INSIDE SCOOP • ARTIFICIAL PRESERVATIVES, COLORS, FLAVORS Meet Caroline, Dairy Buyer • ADDED HORMONES AND ANTIBIOTICS • TRANSFATS • PARABENS 13 THE DEEP DISH • HIGH FRUTOSE CORN SYRUP Real Organic Dairy • ANIMAL TESTING 16 RALLY FOR CHANGE To contact the Board of Directors: Living Well Residence [email protected] (802) 388-7276 17 FOOD FETISH Yogurt...Savoring the Sweetness of If you would like to receive an electronic Sour Milk copy of this newsletter, or if you have any questions or comments please contact: Karin Mott [email protected] (802) 388-7276 x307 BECOME A MEMBER! DISCOUNTS AT LOCAL BUSINESSES MEMBER DEALS PATRONAGE REFUND A VOICE AND A VOTE CONTRIBUTORS [email protected] Shannon Foster Emily Landenberger Glenn Lower Karin Mott Tam Stewart 1 When I think of the Vermont landscape, I think of the Green Mountains, maple trees, Lake Champlain and the farms in Addison County. -

N E W S L E T T E R February 2014 XLVI:Ii
The Icelandic Canadian Club of British Columbia N E W S L E T T E R February 2014 XLVI:ii The Icelandic Canadian Club of British Columbia cordially invites you to þorrablót Saturday, March 1, 2014 Time: Cocktail Hour 6 p.m.; Dinner 7 p.m.; Dancing 9 p.m. Scandinavian Centre, 6540 Thomas Street, Burnaby, BC, 604-294-2777 Forréttir (Appetizers) Waiters will circulated with appetizers during the Cocktail Hour, 6-7 pm Reyktur lax með sinnepssósu á rúgbrauði; Lifrarkæfa ófan á kex; Flatkökur með marineraði síld; Tartalettur með aspas, osti og skinku; Rúlllapylsa á rugbrauði Sampling Table with: lifrapylsa, blóðmör, rúllupylsa, hákarl, harðfisk, sviðasulta, hrútspungar Buffet Multigrain Rolls & Butter; Mixed Greens with Strawberries, Basil and Pear; Balsamic – Maple Dressing; Kale, Arugula, Beets, Goat Cheese and Candied Pecans; Italian Dressing AAA Roast Beef Carved at the Table, Beef Jus and Spicy Horseradish; Hangikjöt (Smoked Lamb); Pan Roasted Chicken Breast; Choice of Sauce: BBQ, Lemon Garlic, or Mediterranean; Beef, Cheese or Mushroom Ravioli; Marinara or Alfredo Cream Sauce; Herbed Baby Potatoes, Mashed Potatoes or Jasmine Rice; Grilled Seasonal Vegetables Dessert: Vínarterta, Pönnukökur, Kleinur Beverage: Coffee, Tea After dinner Entertainment Dancing to a 6 piece band, Pizzazz 50/50 Draw Dress: Semi-Formal Cost: $4000 Students: $2500 Tickets: Leif Erickson 604-581-9767; Nina Jobin 604-277-0143. Reserve by Wednesday morning, February 26. No ticket sales at the door. Encourage your young adults to come. Good food and a real live band! All tables will be reserved. We will arrange for those who wish to sit together at the same table, or at adjoining tables, to be able to do so. -

Crafted with Tradition, Baked with Passion!
Crafted with tradition, baked with passion! MINI SKYR CAKES ORIGINAL PRODUCT Skyr is an Icelandic cultured dairy product. It has the consistency of strained yogurt/ greek yogurt but a much milder flavor. It has been a part of Icelandic cuisine for Nordics over a thousand years. It is traditionally served with cold milk and a topping of sugar. Dawn Foods Germany GmbH Riedstraße 6, 64295 Darmstadt Germany The Chef’s twist Skyr used in baked cheese cake. Combined with several trendy taste combinations. WWW.DAWNFOODS.COM For more insights and solutions, contact us at +420602775022 Nordics_02 Nordics_02MINI SKYR CAKES Skyr Cheese Cake SkyrCOMPOSITION Cheese Cake PROCESSING for 12 mini cakes Ø 7 cm , high 7 cm Mix Dawn Creme Cake Base Plain CL and butter until a nice crumble structure and Belnap 600 g Crumble press the mixture into a loose-bottomed tin about 1 cm layer 1200 g Skyr base Belnap Pipe MangoVanilla Skyr fruitfilling onto crumble base BASIC RECIPES Mix all ingredients with a flatbeater for a skyr base, pipe onto the crumble base Vanilla Skyr Crumble and bakeCrumble 1000 g Dawn Creme Cake Base Plain CL Crumble 250 g Butter TEMPERATURE: 175 °C Chocolate Crumble TIME: 30 - 35 minutes 1000 g Dawn Creme Cake Base Chocolate CL 250 g Butter Decorate see picture above Skyr Cheese Cake SkyrSkyr Cheese Base Cake 1000 g Skyr 350 g Dawn Cheese Cake Easy 175 g Eggs Item Code Product name Packaging 0.02336.487 Dawn Creme Cake Base Plain CL Bag 12,5 kg 75 g Sugar BelnapBelnap 70 g Vegetable oil 0.02336.502 Dawn Creme Cake Base Chocolate CL Bag