Perkinelmer New Coronavirus Nucleic Acid Detection Kit and Decrease Sensitivity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Network Chromatography Interface 901/902 Operator's Manual
Network Chromatography Interface 901/902 Operator’s Manual Release History Part Number Release Publication Date N515-6030 A April 2001 Any comments about the documentation for this product should be addressed to: User Assistance PerkinElmer Instruments LLC 710 Bridgeport Avenue Shelton, Connecticut 06484-4794 U.S.A Or emailed to: [email protected] Notices The information contained in this document is subject to change without notice. PerkinElmer makes no warranty of any kind with regard to the material, including, but not limited to, the implied warranties of merchantability and fitness for a particular purpose. PerkinElmer shall not be liable for errors contained herein for incidental consequential damages in connection with furnishing, performance or use of this material. NOTE: TotalChrom is the updated version of the software previously marketed as Turbochrom. This product is compatible with TotalChrom and Turbochrom version 6.1.x. The term TotalChrom has been used throughout this document to denote either system. Copyright Information This document contains proprietary information that is protected by copyright. All rights are reserved. No part of this publication may be reproduced in any form whatsoever or translated into any language without the prior, written permission of PerkinElmer Instruments LLC. Copyright © 2001 PerkinElmer Instruments LLC. Trademarks Registered names, trademarks, etc. used in this document, even when not specifically marked as such, are protected by law. PerkinElmer is a registered trademark of PerkinElmer, Inc. Network Chromatography Interface, NCI, Access*Chrom, TotalChrom, TotalChrom Client/Server, and TotalChrom Workstation are trademarks of PerkinElmer Inc. Turbochrom is a trademark of Applera Corporation. Table of Contents Chapter 1 Introduction.............................................................................................1 NCI 901 Operates on Channel A Only ...................................................................................... -

Applied Biosystems 3730 and 3730Xl DNA Analyzers
SPECIFICATION SHEET 3730 and 3730xl DNA Analyzers Applied Biosystems 3730 and 3730xl DNA Analyzers Introduction Applied Biosystems 3730 & 3730xl DNA Analyzers were developed to meet the growing needs of institutions ranging from core and research labs in academia, government, and medicine to biotechnology, pharmaceuticals, and genome centers. These high-throughput instruments couple advances in automation and optics with proprietary Applied Biosystems reagents and software to support a diverse range Key Features Key Benefits of genetic analysis projects. By • Dual-side capillary illumination • Highest-quality DNA sequencing data dramatically improving data quality, at lowest cost • Backside-thinned CCD significantly reducing total cost per – POP-7™ Polymer separation matrix sample, and enabling more runs per • Integrated auto-sampler and sample increases read length and reduces day, 3730/3730xl DNA Analyzers make plate stacker run time it quicker and easier for investigators • Onboard piercing station to get meaningful results in evolving – Multiple run modules provide options genomic applications. Whether your • Internal barcode reader for targeted length of read lab is involved in de novo sequencing, • Onboard polymer for up to 100 runs – High optical sensitivity reduces DNA resequencing, microsatellite-based and reagent consumption fragment analysis, or SNP genotyping, • Automated basecalling and quality 3730/3730xl DNA Analyzers are the value assignment – In-capillary detection consumes ideal platform for better, faster, cheaper • -

SIRION Biotech to Be Acquired by Perkinelmer Torreya Advised SIRION on the Transaction Munich, Germany, June 22, 2021
SIRION Biotech to be acquired by PerkinElmer Torreya advised SIRION on the transaction Munich, Germany, June 22, 2021 PerkinElmer, Inc. announced it has entered into an agreement to acquire SIRION Biotech GmbH (“SIRION”), a global provider of viral vector-based technologies that drive improved delivery performance for cell and gene therapies. The acquisition is expected to close during the third quarter of 2021. Founded in 2005, SIRON is a leading commercial supplier of viral vector technologies for gene and cell therapy as well as vaccine development. SIRION develops novel therapeutic viral vectors and uses proprietary technology platforms based on lenti-, adeno-, and adenoassociated viruses, to expedite its customers’ advances in drug development. Additionally, SIRION has established a strong licensing portfolio leveraged by over a dozen major pharmaceutical and biotech players researching more than twenty-five diseases and conditions. The addition of SIRION’s offerings will complement PerkinElmer’s Horizon Discovery portfolio which includes gene editing and modulation tools for CRISPR, CRISPRi and RNAi, custom cell lines for bioproduction and base editing technologies. SIRION will benefit from becoming part of the PerkinElmer portfolio, with increased access to genomics analysis, gene editing and base editing technologies, as well as a strong global infrastructure and reach. Torreya advised SIRION on the transaction, which highlights both Torreya’s expertise in the bioproduction space and deep relationships within the biotech community. -

Automated DNA Sequencing
Automated DNA Sequencing Chemistry Guide ©Copyright 1998, The Perkin-Elmer Corporation This product is for research purposes only. ABI PRISM, MicroAmp, and Perkin-Elmer are registered trademarks of The Perkin-Elmer Corporation. ABI, ABI PRISM, Applied Biosystems, BigDye, CATALYST, PE, PE Applied Biosystems, POP, POP-4, POP-6, and Primer Express are trademarks of The Perkin-Elmer Corporation. AmpliTaq, AmpliTaq Gold, and GeneAmp are registered trademarks of Roche Molecular Systems, Inc. Centricon is a registered trademark of W. R. Grace and Co. Centri-Sep is a trademark of Princeton Separations, Inc. Long Ranger is a trademark of The FMC Corporation. Macintosh and Power Macintosh are registered trademarks of Apple Computer, Inc. pGEM is a registered trademark of Promega Corporation. Contents 1 Introduction. 1-1 New DNA Sequencing Chemistry Guide . 1-1 Introduction to Automated DNA Sequencing . 1-2 ABI PRISM Sequencing Chemistries . 1-5 PE Applied Biosystems DNA Sequencing Instruments . 1-7 Data Collection and Analysis Settings . 1-12 2 ABI PRISM DNA Sequencing Chemistries . 2-1 Overview . 2-1 Dye Terminator Cycle Sequencing Kits . 2-2 Dye Primer Cycle Sequencing Kits . 2-8 Dye Spectra . 2-12 Chemistry/Instrument/Filter Set Compatibilities . 2-13 Dye/Base Relationships for Sequencing Chemistries . 2-14 Choosing a Sequencing Chemistry. 2-15 3 Performing DNA Sequencing Reactions . 3-1 Overview . 3-1 DNA Template Preparation . 3-2 Sequencing PCR Templates . 3-10 DNA Template Quality. 3-15 DNA Template Quantity. 3-17 Primer Design and Quantitation . 3-18 Reagent and Equipment Considerations. 3-20 Preparing Cycle Sequencing Reactions . 3-21 Cycle Sequencing . 3-27 Preparing Extension Products for Electrophoresis . -
Document Title: Development and Evaluation of a Whole Genome Amplification Method for Accurate Multiplex STR Genotyping of Compromised Forensic Casework Samples
The author(s) shown below used Federal funds provided by the U.S. Department of Justice and prepared the following final report: Document Title: Development and Evaluation of a Whole Genome Amplification Method for Accurate Multiplex STR Genotyping of Compromised Forensic Casework Samples Author: Tracey Dawson Cruz, Ph.D. Document No.: 227501 Date Received: July 2009 Award Number: 2005-DA-BX-K002 This report has not been published by the U.S. Department of Justice. To provide better customer service, NCJRS has made this Federally- funded grant final report available electronically in addition to traditional paper copies. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice. This document is a research report submitted to the U.S. Department of Justice. This report has not been published by the Department. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice. FINAL TECHNICAL REPORT Development and Evaluation of a Whole Genome Amplification Method for Accurate Multiplex STR Genotyping of Compromised Forensic Casework Samples NIJ Award #: 2005-DA-BX-K002 Author: Tracey Dawson Cruz 1 This document is a research report submitted to the U.S. Department of Justice. This report has not been published by the Department. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. -
List of SARS-Cov-2 Diagnostic Test Kits and Equipments Eligible For
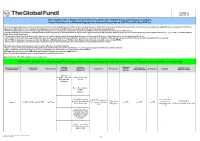
Version 33 2021-09-24 List of SARS-CoV-2 Diagnostic test kits and equipments eligible for procurement according to Board Decision on Additional Support for Country Responses to COVID-19 (GF/B42/EDP11) The following emergency procedures established by WHO and the Regulatory Authorities of the Founding Members of the GHTF have been identified by the QA Team and will be used to determine eligibility for procurement of COVID-19 diagnostics. The product, to be considered as eligible for procurement with GF resources, shall be listed in one of the below mentioned lists: - WHO Prequalification decisions made as per the Emergency Use Listing (EUL) procedure opened to candidate in vitro diagnostics (IVDs) to detect SARS-CoV-2; - The United States Food and Drug Administration’s (USFDA) general recommendations and procedures applicable to the authorization of the emergency use of certain medical products under sections 564, 564A, and 564B of the Federal Food, Drug, and Cosmetic Act; - The decisions taken based on the Canada’s Minister of Health interim order (IO) to expedite the review of these medical devices, including test kits used to diagnose COVID-19; - The COVID-19 diagnostic tests approved by the Therapeutic Goods Administration (TGA) for inclusion on the Australian Register of Therapeutic Goods (ARTG) on the basis of the Expedited TGA assessment - The COVID-19 diagnostic tests approved by the Ministry of Health, Labour and Welfare after March 2020 with prior scientific review by the PMDA - The COVID-19 diagnostic tests listed on the French -

Rutgers Clinical Genomics Laboratory Taqpath SARS-Cov-2 Assay EUA Summary
Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay EUA Summary ACCELERATED EMERGENCY USE AUTHORIZATION (EUA) SUMMARY SARS-CoV-2 ASSAY (Rutgers Clinical Genomics Laboratory) For in vitro diagnostic use Rx only For use under Emergency Use Authorization (EUA) Only (The Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay will be performed in the Rutgers Clinical Genomics Laboratory, a Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. §263a certified high-complexity laboratory, per the Instructions for Use that were reviewed by the FDA under this EUA). INTENDED USE The Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay is a real-time reverse transcription polymerase chain reaction (rRT-PCR) test intended for the qualitative detection of nucleic acid from SARS-CoV-2 in oropharyngeal (throat) swab, nasopharyngeal swab, anterior nasal swab, mid-turbinate nasal swab, and bronchoalveolar lavage (BAL) fluid from individuals suspected of COVID-19 by their healthcare provider. This test is also for use with saliva specimens that are self-collected at home or in a healthcare setting by individuals using the Spectrum Solutions LLC SDNA-1000 Saliva Collection Device when determined to be appropriate by a healthcare provider. Testing is limited to Rutgers Clinical Genomics Laboratory (RCGL) at RUCDR Infinite Biologics – Rutgers University, Piscataway, NJ, that is a Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. §263a certified high-complexity laboratory. Results are for the detection and identification of SARS-CoV-2 RNA. The SARS- CoV-2 RNA is generally detectable in respiratory specimens during the acute phase of infection. -

Onesource Multi-Vendor Service
qualifyMaintain all of your and and GC,GC/MS HPLC, systems LC/MS, Multi-Vendor Service One contract One contact One solution You depend on your GC, HPLC, LC/MS • Which manufacturer do you call when your chromatography system goes down? or GC/MS to work reliably, day • How do you get the rapid and effective response you need? after day. But maintenance and • How do you ensure each component is in compliance with FDA regulations and that the overall system is in compliance? compliance can be a real challenge Now you can reduce downtime, increase your lab’s productivity and enhance if your total analysis system has compliance with the help of OneSource® Multi-Vendor Service. components from different Rely on ONE expert PerkinElmer Service Engineer who can provide customized preventative maintenance, repair and qualification services for your entire chromatography manufacturers. chromatography system, regardless of manufacturer. Focus on the science. We handle the rest. One proven, cost-effective solution can keep your chromatography systems at peak performance. That’s OneSource Multi-Vendor Service. • One point of service contact — • Dedicated multi-vendor support • Standardized reporting and total system approach to maintenance, team — takes ownership of your issues: documentation — provides enhanced repair and qualification: - Ensures rapid deployment of traceability of system maintenance - Eliminates multiple service visits, your local Service Engineer. and repair history; improves regulatory saving you time and money. - Provides parts sourcing over the compliance. - Reduces service contract lifetime of your equipment. • Maximum system uptime and administration costs. • One expert Service Engineer — equipment availability —no - Reduces time lab personnel are on our highly trained PerkinElmer engineers downtime due to multiple vendors’ lack the phone with multiple service can provide customized preventative of total system understanding, thus providers. -

DNA Fragment Analysis by Capillary Electrophoresis User Guide
USER GUIDE DNA Fragment Analysis by Capillary Electrophoresis Publication Number 4474504 Revision B For Research Use Only. Not intended for use in diagnostic procedures. For Research Use Only. Not intended for use in diagnostic procedures. The information in this guide is subject to change without notice. DISCLAIMER LIFE TECHNOLOGIES CORPORATION AND/OR ITS AFFILIATE(S) DISCLAIM ALL WARRANTIES WITH RESPECT TO THIS DOCUMENT, EXPRESSED OR IMPLIED, INCLUDING BUT NOT LIMITED TO THOSE OF MERCHANTABILITY, FITNESS FOR A PARTICULAR PURPOSE, OR NON-INFRINGEMENT. TO THE EXTENT ALLOWED BY LAW, IN NO EVENT SHALL LIFE TECHNOLOGIES AND/OR ITS AFFILIATE(S) BE LIABLE, WHETHER IN CONTRACT, TORT, WARRANTY, OR UNDER ANY STATUTE OR ON ANY OTHER BASIS FOR SPECIAL, INCIDENTAL, INDIRECT, PUNITIVE, MULTIPLE OR CONSEQUENTIAL DAMAGES IN CONNECTION WITH OR ARISING FROM THIS DOCUMENT, INCLUDING BUT NOT LIMITED TO THE USE THEREOF. TRADEMARKS All trademarks are the property of Thermo Fisher Scientific and its subsidiaries unless otherwise specified. AmpErase, AmpliTaq, AmpliTaq Gold, and TaqMan are registered trademarks of Roche Molecular Systems, Inc. AFLP is a registered trademark of Keygene N.V. Millipore is a registered trademark of Merck KGaA. © 2014 Thermo Fisher Scientific Inc. All rights reserved. Contents About This Guide . 13 Revision history . 13 Purpose . 13 Prerequisites . 13 Structure of this guide . 14 ■ CHAPTER 1 Introduction to Fragment Analysis . 15 Fragment analysis versus sequencing…what is the difference? . 15 Fragment analysis . 15 Sequencing . 16 What can I do with fragment analysis? . 16 Types of applications . 16 Applications described in this guide . 17 What is capillary electrophoresis? . 18 Fragment analysis workflow . 19 ■ CHAPTER 2 Experimental Design . -

Supporting Information Supplementary Methods
Supporting Information Supplementary methods This appendix was part of the submitted manuscript and has been peer reviewed. It is posted as supplied by the authors. Appendix to: Caly L, Druce J, Roberts J, et al. Isolation and rapid sharing of the 2019 novel coronavirus (SAR-CoV-2) from the first patient diagnosed with COVID-19 in Australia. Med J Aust 2020; doi: 10.5694/mja2.50569. Supplementary methods 1.1 Generation of SARS-CoV-2 cDNA 200μL aliquots from swab (nasopharyngeal in VTM), sputum, urine, faeces and serum samples were subjected to RNA extraction using the QIAamp 96 Virus QIAcube HT Kit (Qiagen, Hilden, Germany) and eluted in 60μL. Reverse transcription was performed using the BioLine SensiFAST cDNA kit (Bioline, London, United Kingdom), total reaction mixture (20μL), containing 10μL RNA extract, 4μL 5x TransAmp buffer, 1μL reverse transcriptase and 5μL nuclease-free water. The reactions were incubated at 25°C for 10 min, 42°C for 15 min and 85°C for 5 min. 1.2 Nested SARS-CoV-2 RT-PCR and Sanger sequencing A PCR mixture containing 2μL cDNA, 1.6 μl 25mM MgCl2, 4μL 10x Qiagen Taq Buffer, 0.4μL 20mM dNTPs, 0.3μL Taq polymerase (Qiagen, Hilden, Germany) and 2μL of 10 μM primer pools as described2. Briefly, first round included the forward (5'-GGKTGGGAYTAYCCKAARTG-3') and reverse (5'-GGKTGGGAYTAYCCKAARTG-3') primers. Cycling conditions were 94°C for 10min, followed by 30 cycles of 94°C for 30s, 48°C for 30s and 72°C for 40s, with a final extension of 72°C for 10 min. -

Complete Listing of All Statewide Contracts
Procurement Services All Term Contracts by Group Number Contract Contract Contractor Group Description Period Award# MB/WB No. Name / SB 01600 MILK (FLUID) (STATEWIDE) 9/21/2015 - 9/20/2021 22773 PC67026 CREAM-O-LAND DAIRIES LLC 01600 MILK (FLUID) (STATEWIDE) 9/21/2015 - 9/20/2021 22773 PC67027 UPSTATE NIAGARA COOPERATIVE INC 01600 MILK (FLUID) (STATEWIDE) 9/21/2015 - 9/20/2021 22773 PC68955 HUDSON VALLEY FRESH DAIRY LLC 01600 MILK (FLUID) (STATEWIDE) 9/21/2015 - 9/20/2021 22773 PC68964 UPSTATE FARMS DAIRY LLC 01800 ROAD SALT, TREATED SALT & EMERGENCY STANDY SALT 9/1/2018 - 8/31/2022 23134 PC68227 AMERICAN ROCK SALT COMPANY LLC 01800 ROAD SALT, TREATED SALT & EMERGENCY STANDY SALT 9/1/2018 - 8/31/2022 23134 SB PC68228 APALACHEE LLC 01800 ROAD SALT, TREATED SALT & EMERGENCY STANDY SALT 9/1/2018 - 8/31/2022 23134 SB PC68229 ATLANTIC SALT INC 01800 ROAD SALT, TREATED SALT & EMERGENCY STANDY SALT 9/1/2018 - 8/31/2022 23134 PC68230 CARGILL INC SALT ROAD SAFETY 01800 ROAD SALT, TREATED SALT, & EMERGENCY STANDBY SALT (STATEWIDE) 9/1/2019 - 8/31/2022 23175 PC68889 AMERICAN ROCK SALT COMPANY LLC 01800 ROAD SALT, TREATED SALT, & EMERGENCY STANDBY SALT (STATEWIDE) 9/1/2019 - 8/31/2022 23175 SB PC68890 APALACHEE LLC 01800 ROAD SALT, TREATED SALT, & EMERGENCY STANDBY SALT (STATEWIDE) 9/1/2019 - 8/31/2022 23175 SB PC68891 ATLANTIC SALT INC 01800 ROAD SALT, TREATED SALT, & EMERGENCY STANDBY SALT (STATEWIDE) 9/1/2019 - 8/31/2022 23175 PC68892 CARGILL INC SALT ROAD SAFETY 01800 ROAD SALT, TREATED SALT & EMERGENCY STANDBY SALT 9/18/2020 - 8/31/2022 23212 -

Applied Biosystems 3130 and 3130Xl Genetic Analyzers
System Profile Applied Biosystems 3130 and 3130xl Genetic Analyzers. System Profile Applied Biosystems 3130 and 3130xl Genetic Analyzers Table of Contents A Powerful Blend of Flexibility and Performance 1 Ease-of-Use 1 Key Features 2 Capillary Electrophoresis 2 Automated Polymer Delivery System 2 Enhanced Thermal Control 2 High-Perfomance Capillaries and Electro-osmotic Flow Suppression (EOF) Polymers 2 Detection Method Designed for Sensitivity 3 Spectral Array Detection 3 Application Flexibility 4 Complete System Optimized for Multiple Applications 4 One Polymer, One Array, Maximum Performance 4 System Software Suite 5 Results 6 Summary 9 References 10 www.appliedbiosystems.com 16-capillary 3130xl Genetic Analyzer: High-performance workhorse. With 16-capillary throughput and advanced automation capabilities, the 3130xl system is flexible enough to meet the throughput needs of the busiest core facility or research group. The streamlined set-up and 24-hour unattended operation make it an ideal choice for low or medium throughput laboratories. Ease-of-Use Complete automation. At every scale, Applied Biosystems genetic analyzers are known for their advanced automation and “hands-free” operation. The Automated Polymer Delivery System A Powerful Blend of Flexibility and Performance eliminates manual washing and filling of polymer syringes, Applied Biosystems has a long tradition of providing significantly reducing the time required for instrument set- excellence in life science instruments, reagents, and software. up and maintenance. All steps are automated, including This tradition of pioneering and innovation in the field polymer loading, sample injection, separation and detection, of genetic analysis continues with the introduction of and data analysis. After placing plates on the autosampler Applied Biosystems next-generation systems, the 3130 and importing sample information, just select the “Start and 3130xl Genetic Analyzers.