Chronic Scrotal Content Pain: an Updated Review on Diagnosis and Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urologic Malignancies
Scope • Anatomy •Urologic Malignancies • Trauma • Emergencies • Infections • Lower Urinary Tract Obstruction • Upper Urinary Tract Obstruction • Pediatric Urology • Key Points Emmanuel L. Barcenas Urologist/Urologic Surgeon Urology Specialty Group and Associates • Doctor of Medicine, SWU • Diplomate, Philippine Board of Surgery and the Philippine Board of Urology • Fellow, Philippine Urological Association • Fellow, Philippine College of Surgeons • Member, Philippine Endourological Society • Member, Phillippine Society of Urooncologists Urologic Malignancies Urologic Malignancies •Bladder Cancer •Testicular Cancer •Kidney Cancer •Prostate Cancer Urothelial Tumors of the UB •Transitional cell epithelium lines the urinary tract from the renal pelvis, ureter, urinary bladder, and the proximal two-thirds of the urethra •Tobacco use is the most frequent risk factor (50% in men and 40% in women), followed by occupational exposure to various carcinogenic materials such as automobile exhaust or industrial solvents. Detection of Urothelial Cancer •Painless gross hematuria occurs in 85% of patients & requires a complete evaluation that includes cystoscopy, urine cytology, CT scan, & a PSA. •Recurrent or significant hematuria (>3 RBC’s/HPF on 3 urinalysis, a single urinalysis with >100 RBCs, or gross Hematuria) is associated with significant renal or urologic lesion in 9.1% Detection of Urothelial Cancer • Patients with microscopic hematuria require a full evaluation, but low-risk patients do not require repeat evaluations. • High-risk individuals primarily are those with a smoking history & should be evaluated every 6 months. • The level of suspicion for urogenital neoplasms in patients with isolated painless hematuria and nondysmorphic RBCs increases with age. • White light cystoscopy with random bladder biopsies is the gold standard for tumor detection History & Staging •Low-grade papillary lesions are likely to recur in up to 60% of patients but invade in less than 10% of cases. -

Study of Anatomical Pattern of Lumbar Plexus in Human (Cadaveric Study)
54 Az. J. Pharm Sci. Vol. 54, September, 2016. STUDY OF ANATOMICAL PATTERN OF LUMBAR PLEXUS IN HUMAN (CADAVERIC STUDY) BY Prof. Gamal S Desouki, prof. Maged S Alansary,dr Ahmed K Elbana and Mohammad H Mandor FROM Professor Anatomy and Embryology Faculty of Medicine - Al-Azhar University professor of anesthesia Faculty of Medicine - Al-Azhar University Anatomy and Embryology Faculty of Medicine - Al-Azhar University Department of Anatomy and Embryology Faculty of Medicine of Al-Azhar University, Cairo Abstract The lumbar plexus is situated within the substance of the posterior part of psoas major muscle. It is formed by the ventral rami of the frist three nerves and greater part of the fourth lumbar nerve with or without a contribution from the ventral ramus of last thoracic nerve. The pattern of formation of lumbar plexus is altered if the plexus is prefixed (if the third lumbar is the lowest nerve which enters the lumbar plexus) or postfixed (if there is contribution from the 5th lumbar nerve). The branches of the lumbar plexus may be injured during lumbar plexus block and certain surgical procedures, particularly in the lower abdominal region (appendectomy, inguinal hernia repair, iliac crest bone graft harvesting and gynecologic procedures through transverse incisions). Thus, a better knowledge of the regional anatomy and its variations is essential for preventing the lesions of the branches of the lumbar plexus. Key Words: Anatomical variations, Lumbar plexus. Introduction The lumbar plexus formed by the ventral rami of the upper three nerves and most of the fourth lumbar nerve with or without a contribution from the ventral ramous of last thoracic nerve. -

Lower Extremity Focal Neuropathies
LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Arturo A. Leis, MD S.H. Subramony, MD Vettaikorumakankav Vedanarayanan, MD, MBBS Mark A. Ross, MD AANEM 59th Annual Meeting Orlando, Florida Copyright © September 2012 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 Printed by Johnson Printing Company, Inc. 1 Please be aware that some of the medical devices or pharmaceuticals discussed in this handout may not be cleared by the FDA or cleared by the FDA for the specific use described by the authors and are “off-label” (i.e., a use not described on the product’s label). “Off-label” devices or pharmaceuticals may be used if, in the judgment of the treating physician, such use is medically indicated to treat a patient’s condition. Information regarding the FDA clearance status of a particular device or pharmaceutical may be obtained by reading the product’s package labeling, by contacting a sales representative or legal counsel of the manufacturer of the device or pharmaceutical, or by contacting the FDA at 1-800-638-2041. 2 LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Table of Contents Course Committees & Course Objectives 4 Faculty 5 Basic and Special Nerve Conduction Studies of the Lower Limbs 7 Arturo A. Leis, MD Common Peroneal Neuropathy and Foot Drop 19 S.H. Subramony, MD Mononeuropathies Affecting Tibial Nerve and its Branches 23 Vettaikorumakankav Vedanarayanan, MD, MBBS Femoral, Obturator, and Lateral Femoral Cutaneous Neuropathies 27 Mark A. Ross, MD CME Questions 33 No one involved in the planning of this CME activity had any relevant financial relationships to disclose. -

Guidelines on Testicular Cancer
GUIDELINES ON TESTICULAR CANCER (Limited text update March 2015) P. Albers (Chair), W. Albrecht, F. Algaba, C. Bokemeyer, G. Cohn-Cedermark, K. Fizazi, A. Horwich, M.P. Laguna, N. Nicolai, J. Oldenburg Eur Urol 2011 Aug;60(2):304-19 Introduction Compared with other types of cancer, testicular cancer is relatively rare accounting for approximately 1-1.5% of all cancers in men. Nowadays, testicular tumours show excellent cure rates, mainly due to early diagnosis and their extreme chemo- and radiosensitivity. Staging and Classification Staging For an accurate staging the following steps are necessary: Postorchiectomy half-life kinetics of serum tumour markers. The persistence of elevated serum tumour markers after orchiectomy may indicate the presence of disease, while their normalisation does not necessarily mean absence of tumour. Tumour markers should be assessed until they are normal, as long as they follow their half-life kinetics and no metastases are revealed. A chest CT scan should be routinely performed in patients diagnosed with non-seminomatous germ cell tumours (NSGCT), because in up to 10% of cases, small subpleural nodes may be present that are not visible radiologically. 110 Testicular Cancer Recommended tests for staging at diagnosis Test Recommendation GR Serum tumour markers Alpha-fetoprotein A hCG LDH Abdominopelvic CT All patients A Chest CT All patients A Testis ultrasound (bilateral) All patients A Bone scan or MRI columna In case of symptoms Brain scan (CT/MRI) In case of symptoms and patients with meta- static disease with mul- tiple lung metastases and/or high beta-hCG values. Further investigations Fertility investigations: B Total testosterone LH FSH Semen analysis Sperm banking should be offered. -

Paratesticular Metastasis of High Grade Prostate Cancer Clinically
CASE REPORT Urooncology Doi: 10.4274/jus.481 Journal of Urological Surgery, 2017;4:26-28 Paratesticular Metastasis of High Grade Prostate Cancer Clinically Mimicking Hemato/Pyo-hydrocele Paratestiküler Metastazla Presente Olan Yüksek Dereceli Prostat Adenokarsinomu Hikmet Köseoğlu1, Şemsi Altaner2 1Başkent University Faculty of Medicine, Department of Urology, İstanbul, Turkiye 2Başkent University Faculty of Medicine, Department of Pathology, İstanbul, Turkiye Abstract Secondary metastatic lesions of the testicles are very rare and they originate mainly from prostate adenocarcinoma. They are generally diagnosed incidentally, however, they very rarely manifest as a palpable testicular mass. In this paper, we present, a case of paratesticular metastasis from high- grade prostate cancer clinically mimicking pyo-/hemato-/hydrocele. A 75-year-old man, who had been followed up elsewhere for a huge hydrocele based on scrotal Doppler ultrasonography and scrotal magnetic resonance imaging reporting no suspicion for malignancy, but a pyo-/hemato-/ hydrocele was determined to have testicular metastasis originating from prostate adenocarcinoma. Keywords: Hydrocele, testis, neoplasm metastasis, prostate, adenocarcinoma Öz Testisin metastatik lezyonları oldukça nadirdir ve çoğunlukla prostat kanserinden köken almaktadırlar. Genellikle rastlantısal olarak tanı alırlar; ancak çok nadir testiste palpe edilebilen kitle ile belirti verirler. Bu olgu bildirisinde klinik olarak pyo-/hemato-/hidrosel olarak izlenen olguda yüksek dereceli prostat kanseri metastazı -
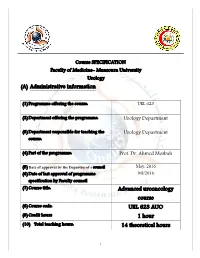
(A) Administrative Information Advanced Urooncology Course URL
Course SPECIFICATION Faculty of Medicine- Mansoura University Urology (A) Administrative information (1) Programme offering the course: URL 623 (2) Department offering the programme: Urology Department (3) Department responsible for teaching the Urology Department course: (4) Part of the programme: Prof. Dr. Ahmed Mosbah (5) Date of approval by the Department`s council May, 2016 (6) Date of last approval of programme 9/8/2016 specification by Faculty council (7) Course title: Advanced urooncology course (8) Course code: URL 623 AUO (9) Credit hours 1 hour (10) Total teaching hours: 14 theoretical hours 1 (B) Professional information (1) Programme Aims: The general aim of the course is to provide postgraduate students with the knowledge, skills and some attitudes necessary to make an essential urologic framework of the urologist including awareness of the common urologic emergencies. 1- Enlist the etiology, pathology, diagnosis and treatment of urologic tumours. 2- Describe emergencies related to urologic oncology and how to deal with it. 3- Define the steps of performing radical nephrectomy, radical cystectomy, radical prostatectomy, high inguinal orchiectomy and penectomy. 4- Practice urologic oncology in the outpatient clinic under supervision by the faculty members. 5- Study how to evaluate the urologic oncology patient. 6- Design a research proposal and how to implement and publish it. 7- Describe different modalities of treatment of urologic tumours other than surgery. (2) Intended Learning Outcomes (ILOs): Intended learning outcomes (ILOs); Are four main categories: knowledge & understanding to be gained, intellectual qualities, professional/practical and transferable skills. On successful completion of the programme, the candidate will be able to: A- Knowledge and Understanding K1 Biological behavior of all urologic tumours. -

The Dissemination of Pelvic Limb Nerves Originating from the Lumbosacral Plexus in the Porcupine (Hystrix Cristata)
Veterinarni Medicina, 54, 2009 (7): 333–339 Original Paper The dissemination of pelvic limb nerves originating from the lumbosacral plexus in the porcupine (Hystrix cristata) A. Aydin Faculty of Veterinary Medicine, Firat University, Elazig, Turkey ABSTRACT: In this study the nerves originating from the plexus lumbosacrales of porcupines (Hystrix cristata) were investigated. Four porcupines (two males and two females) were used. The plexus lumbosacrales of animals were appropriately dissected and dissemination of pelvic limb nerves originating from the plexus lumbosacrales was examined. The nerves originated from the plexus lumbosacrales of porcupines (Hystrix cristata): iliohypogastric nerve from T15, ilioinguinal nerve (on the left side of only one animal) genitofemoral and lateral femoral cutane- ous nerves from T15 and L1, the femoral and obturator nerves from T15, L1, L2 and L3. The femoral nerve divided into two as the common dorsal digital nerve I and II after it branched into motor and skin nerves. The cranial gluteal nerve originated from L3 and L4 in males and from only L3 in females. The caudal gluteal nerve and the caudal femoral cutaneous and sciatic nerves originated from the common root which was formed by the union of L3, L4 and S1 in one animal, and by the union of L3, L4, S1 and S2 in the three other animals. The sciatic nerve divided into the tibial and fibular nerve. The fibular nerve divided into two as the common dorsal digital nerve III and IV, and extended after branching in one direction to extensor muscles. The tibial nerve divided into the common palmares digital nerve I, II, III and IV, and extended after branching into the cutaneous surae caudales nerve and rami muscle distales. -

Surgicaltechniques
OBGM_0806_Hatch.final 7/21/06 11:06 AM Page 17 SURGICALTECHNIQUES THE RETROPERITONEAL SPACE Keeping vital structures out of harm’s way Knowledge of the retroperitoneal space is critical, to avoid unnecessary blood loss and injury of the ureter, bladder, bowel, and nerves he accomplished gynecologic sur- Kenneth D. Hatch, MD The “landmark” Professor, Department geon must know the anatomy of of Obstetrics and Gynecology, T the retroperitoneal space in order umbilical ligament Arizona Health Sciences Center Tucson, Ariz to avoid damage to normal structures, as® Dowden Health Media well as remove pathology. Many disease The umbilical ligament was the umbilical processes involve the pelvic peritoneum, artery in fetal life and courses along the uterosacral ligaments, rectosigmoidCopyrightFor or edgepersonal of the bladder use to theonly anterior abdom- ovarian pedicles, and require the surgeon inal wall up to the umbilicus. It is a useful to enter the retroperitoneal space to iden- guide into the perivesicle space. Lateral to it tify the ureters and blood vessels and are the iliac vessels, and medial is the blad- keep them out of harm’s way. The chal- der. It is also a good marker for finding the IN THIS ARTICLE lenges are complex: right spot to open the round ligament. • Badly distorted anatomy and the ante- ❙ Endometriosis may rior and posterior cul-de-sac necessi- imperil the ureter tate mobilization of the rectosigmoid Page 20 and bladder. • Intraligamentous fibroids require ❙ Preventing ureteral knowledge of the blood supply in the retroperitoneal space. Malignant disor- injury ders mandate that the lymph nodes be Page 23 dissected to determine extent of disease and as part of treatment. -

Castrating Pedophiles Convicted of Sex Offenses Against Children: New Treatment Or Old Punishment
SMU Law Review Volume 51 Issue 2 Article 4 1998 Castrating Pedophiles Convicted of Sex Offenses against Children: New Treatment or Old Punishment William Winslade T. Howard Stone Michele Smith-Bell Denise M. Webb Follow this and additional works at: https://scholar.smu.edu/smulr Recommended Citation William Winslade et al., Castrating Pedophiles Convicted of Sex Offenses against Children: New Treatment or Old Punishment, 51 SMU L. REV. 349 (1998) https://scholar.smu.edu/smulr/vol51/iss2/4 This Article is brought to you for free and open access by the Law Journals at SMU Scholar. It has been accepted for inclusion in SMU Law Review by an authorized administrator of SMU Scholar. For more information, please visit http://digitalrepository.smu.edu. CASTRATING PEDOPHILES CONVICTED OF SEX OFFENSES AGAINST CHILDREN: NEW TREATMENT OR OLD PUNISHMENT? William Winslade* T. Howard Stone** Michele Smith-Bell*** Denise M. Webb**** TABLE OF CONTENTS I. INTRODUCTION ........................................ 351 II. PEDOPHILIA AND ITS TREATMENT ................. 354 A. THE NATURE OF PEDOPHILIA ......................... 355 1. Definition of Pedophilia ........................... 355 2. Sex Offenses and Sex Offenders ................... 357 a. Incidence of Sex Offenses ..................... 357 b. Characteristics of and Distinctions Among Sex O ffenders ..................................... 360 B. ETIOLOGY AND TREATMENT .......................... 364 1. Etiology and Course of Pedophilia................. 364 2. Treatment ......................................... 365 a. Biological of Pharmacological Treatment ...... 366 * Program Director, Program on Legal & Ethical Issues in Correctional Health, In- stitute for the Medical Humanities, James Wade Rockwell Professor of Philosophy of Medicine, Professor of Preventive Medicine & Community Health, and Professor of Psy- chiatry & Behavioral Sciences, University of Texas Medical Branch, Galveston, Texas; Dis- tinguished Visiting Professor of Law, University of Houston Health Law & Policy Institute. -

An Overview of the Management of Post-Vasectomy Pain Syndrome Male Fertility
[Downloaded free from http://www.ajandrology.com on Thursday, March 31, 2016, IP: 208.78.175.61] Asian Journal of Andrology (2016) 18, 1–6 © 2016 AJA, SIMM & SJTU. All rights reserved 1008-682X www.asiaandro.com; www.ajandrology.com Open Access INVITED REVIEW An overview of the management of post-vasectomy pain syndrome Male Fertility Wei Phin Tan, Laurence A Levine Post-vasectomy pain syndrome remains one of the more challenging urological problems to manage. This can be a frustrating process for both the patient and clinician as there is no well-recognized diagnostic regimen or reliable effective treatment. Many of these patients will end up seeing physicians across many disciplines, further frustrating them. The etiology of post-vasectomy pain syndrome is not clearly delineated. Postulations include damage to the scrotal and spermatic cord nerve structures via inflammatory effects of the immune system, back pressure effects in the obstructed vas and epididymis, vascular stasis, nerve impingement, or perineural fibrosis. Post-vasectomy pain syndrome is defined as at least 3 months of chronic or intermittent scrotal content pain. This article reviews the current understanding of post-vasectomy pain syndrome, theories behind its pathophysiology, evaluation pathways, and treatment options. Asian Journal of Andrology (2016) 18, 1–6; doi: 10.4103/1008-682X.175090; published online: 4 March 2016 Keywords: epididymectomy; microdenervation; orchalgia; post-vasectomy pain management; post-vasectomy pain syndrome; testicular pain; vasectomy reversal; vaso-vasostomy INTRODUCTION to PVPS using the Mesh Words “Post-vasectomy Pain Syndrome,” Vasectomies are one of the most common urological procedures performed “Post Vasectomy Pain Syndrome,” “Microdenervation of Spermatic by urologists worldwide. -

The Anatomy and Clinical Implications of the Obturator Nerve and Its Branches
The anatomy and clinical implications of the obturator nerve and its branches by Zithulele Nkosinathi Tshabalala Dissertation submitted in full fulfilment of the requirements for the degree Master of Science in Anatomy In the Faculty of Health Science University of Pretoria Supervisor: Dr A-N van Schoor Co-supervisor: Mrs R Human-Baron Co-supervisor: Mrs S van der Walt 2015 DECLARATION OF ORIGINALITY UNIVERSITY OF PRETORIA The Department of Anatomy places great emphasis upon integrity and ethical conduct in the preparation of all written work submitted for academic evaluation. While academic staff teach you about referencing techniques and how to avoid plagiarism, you too have a responsibility in this regard. If you are at any stage uncertain as to what is required, you should speak to your lecturer before any written work is submitted. You are guilty of plagiarism if you copy something from another author’s work (e.g. a book, an article or a website) without acknowledging the source and pass it off as your own. In effect you are stealing something that belongs to someone else. This is not only the case when you copy work word-for-word (verbatim), but also when you submit someone else’s work in a slightly altered form (paraphrase) or use a line of argument without acknowledging it. You are not allowed to use work previously produced by another student. You are also not allowed to let anybody copy your work with the intention of passing if off as his/her work. Students who commit plagiarism will not be given any credit for plagiarised work. -

A Retrospective Study of Cryptorchidectomy in Horses: Diagnosis, Treatment, Outcome and Complications in 70 Cases
animals Article A Retrospective Study of Cryptorchidectomy in Horses: Diagnosis, Treatment, Outcome and Complications in 70 Cases Paola Straticò, Vincenzo Varasano, Giulia Guerri * , Gianluca Celani , Adriana Palozzo and Lucio Petrizzi Faculty of Veterinary Medicine, University of Teramo, Località Piano D’Accio, 64100 Teramo, Italy; [email protected] (P.S.); [email protected] (V.V.); [email protected] (G.C.); [email protected] (A.P.); [email protected] (L.P.) * Correspondence: [email protected] Received: 26 November 2020; Accepted: 17 December 2020; Published: 21 December 2020 Simple Summary: Cryptorchidism is the failure of one or both testes to descend into the scrotum and is considered to be one of the most common developmental disorders in horses. The aim of the study was to review medical records of horses referred for uni- or bilateral cryptorchidism. It was observed that the Western Riding horse breeds were the most affected, and that left abdominal and right inguinal retentions were the most frequent. Transabdominal ultrasound was the most reliable diagnostic tool to localize the retained testis. Standing laparoscopic and open inguinal cryptorchidectomy were elected as the surgical treatment of choice, in case of abdominal retention and inguinal retention respectively. For incomplete abdominal retention, laparoscopy was the preferred treatment, even though an open inguinal approach was a viable option for the concurrent removal of the descended testis. Abstract: The aim of the study was to investigate the breed predisposition and the diagnostic and surgical management of horses referred for cryptorchidism. The breed, localization of retained testis, diagnosis, type of surgical treatment and complications were analyzed.