Common Aseptic Validation Protocol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Food Packaging (FS 522 / FS 495) Aseptic Processing and Packaging
Food Packaging (FS 522 / FS 495) Aseptic Processing and Packaging Components of an aseptic processing system Aseptic processing is a thermal process in which the product and container are sterilized separately and brought together in a sterile environment. It involves pumping, deaeration, and sterilization of a food product, followed by holding it for a specified period of time (in a holding tube -- required to have a 1/4" rise per foot length of tube), cooling it, and finally packaging it in a sterile container. The use of high temperature for a short period of time (in comparison with conventional canning) in aseptic processing yields a high quality product. Care should be taken to ensure that all process calculations are performed after the deaeration stage and not based on the initial raw product. Deaeration is accomplished in a vessel maintained at a certain degree of vacuum by means of a vacuum pump. The product is fed into the vessel at 55 - 70 /C through a nozzle at the center of the vessel. Vacuum is controlled to obtain a product flash of about 5 /C. An internal spiral condenser condenses vapors and other condensable gases. The deaerated product is discharged through the bottom and pumped to the heating section. Another important part of an aseptic processing system is the back pressure valve which provides sufficient pressure to prevent boiling of the product at processing temperatures which can be as high as 125-130 /C. An aseptic surge tank provides the means for product to be continuously processed even if the packaging system is not operational due to any malfunction. -

WHO Good Manufacturing Practices for Sterile Pharmaceutical Products
© World Health Organization WHO Technical Report Series, No. 961, 2011 Annex 6 WHO good manufacturing practices for sterile pharmaceutical products Introduction Following implementation of these WHO good manufacturing practices (GMP) guidelines (1) within the context of the WHO Prequalifi cation of Medicines Programme, clarifying, editorial modifi cations have been proposed. These changes were adopted for maintenance purposes. In order to ease reading the full guideline has been reproduced again as an Annex to the current report of the WHO Expert Committee on Specifi cations for Pharmaceutical Preparations. WHO good manufacturing practices for sterile pharmaceutical products 1. General considerations 2. Quality control 3. Sanitation 4. Manufacture of sterile preparations 5. Sterilization 6. Ter minal sterilization 7. Aseptic processing and sterilization by fi ltration 8. Isolator technology 9. Blow/fi ll/seal technology 10. Personnel 11. Premises 12. Equipment 13. Finishing of sterile products References Further reading 261 1. General considerations 1.1 The production of sterile preparations should be carried out in clean areas, entry to which should be through airlocks for personnel and/or for equipment and materials. Clean areas should be maintained to an appropriate standard of cleanliness and supplied with air that has passed through fi lters of the required effi ciency. 1.2 The various operations of component preparation (such as those involving containers and closures), product preparation, fi lling and sterilization should be carried out in separate areas within the clean area. These areas are classifi ed into four grades (see section 4). 1.3 Manufacturing operations are divided here into two categories: —fi rst, those where the product is terminally sterilized; and — second, those which are conducted aseptically at some or all stages. -
![IAC 3/11/09 Pharmacy[657] Ch 13, P.1 CHAPTER 13 STERILE](https://docslib.b-cdn.net/cover/7069/iac-3-11-09-pharmacy-657-ch-13-p-1-chapter-13-sterile-417069.webp)
IAC 3/11/09 Pharmacy[657] Ch 13, P.1 CHAPTER 13 STERILE
IAC 3/11/09 Pharmacy[657] Ch 13, p.1 CHAPTER 13 STERILE COMPOUNDING PRACTICES 657—13.1(124,126,155A) Purpose and scope. These rules establish standards and procedures for the preparation, labeling, and distribution of sterile preparations by licensed pharmacies pursuant to a practitioner’s order or prescription; for sterile product quality and characteristics; for personnel training, environmental quality, and equipment standards; and for pharmaceutical care. Sterile compounding differs from nonsterile compounding primarily by requiring the maintenance of sterility when preparations are compounded exclusively with sterile ingredients and components and by requiring the achievement of sterility when preparations are compounded with nonsterile ingredients and components. The standards and procedures outlined in this chapter apply to pharmacy practice when a preparation: 1. Is prepared according to the manufacturer’s labeled instructions and requires other manipulations that expose the original contents to potential contamination; 2. Contains nonsterile ingredients or employs nonsterile components or devices that must be sterilized before administration; or 3. Is a biologic, diagnostic, drug, or nutrient that possesses characteristics of either “1” or “2” above and includes, but is not limited to, the following preparations that are required to be sterile when they are administered to patients: baths and soaks for live organs and tissues, injections (e.g., colloidal dispersions, emulsions, solutions, and suspensions), aqueous bronchial and -

Aseptic Processing White Paper
WHITE PAPER ASEPTIC PROCESSING WHILE MAINTAINING PRODUCT INTEGRITY Published by Marlen A MARLEN WHITE PAPER: Aseptic Processing While Maintaining Product Integrity INTRODUCTION Aseptic processing and packaging is one of the most dynamic areas of food processing. Although invented in the middle of the twentieth century, recently a panel of food technologists and scientists from the Institute of Food Technologists (IFT) with the intention of identifying leading food processing and packaging achievements advised that “Aseptic processing is the most significant food science development in the last 50 years.” The most basic definition of aseptic processing is the independent sterilization of the product followed by filling and sealing (packaging) in sterile containers in a sterile environment. Also known as high-temperature-short-time (HTST) processing, more and more processors are realizing the benefits of aseptic processing and packaging. Therefore, the number of processors utilizing this technology has significantly increased. With the recent advent of the U.S. Food and Drug Administration approval of aseptic processing of food products containing particulate matter, we expect this method of food processing to explode with activity. Marlen pumps facilitate this and fulfill one of the most critical areas of the process. THE PROBLEM In addition to extending the life of shelf stable products, processors must protect heat-sensitive products such as produce, soups, sauces and baby food from microbial degradation. Until recently, continuous thermal aseptic processing solutions using ultra-high temperatures were not approved by the U.S. Food and Drug Administration, forcing processors to use low acid canned food (LACF) methods that compromised the nutritional and organoleptic properties of the food products. -

Thermal Processing Outline
Thermal Processing Outline 1. Classification of Foods based on pH and aw 2. Microbiology 3. Blanching, Pasteurization, ESL (incl. Ultra- Pasteurization), UHT, Hot Fill, Minimal processing 4. Canning Operations 5. Thermal Processing Equipment 6. Kinetics (D & z values) 7. Process Safety (F value) and Product Quality (C value) 8. Process Optimization 9. Shelf Life 10.Time Temperature Integrator (TTI) 1. Classification of Foods Based on pH & aw Classification of Foods based on pH • Low acid: pH ≥ 4.6; Acid: pH < 4.6 (C. botulinum) • More specific classification – Low acid: pH > 5.3 • Red meat, poultry, seafood, milk, corn, peas, lima beans, potatoes, cauliflower – Medium acid: 4.5 < pH < 5.3 • Spaghetti, soups, sauces, asparagus, beets, pumpkin, spinach, green beans, turnip, cabbage – Acid: 3.7 < pH < 4.5 • Tomato, pear, fig, pineapple, apricot, yogurt, white cheese, beer – High acid: pH < 3.7 • Sauerkraut, pickles, berries, citrus, rhubarb, wine, vinegar, plums, currants, apples, strawberries, peaches Classification of Foods Based on mc or aw • High moisture foods (50+% -- 70-99%) – Fruits, vegetables, juices, raw meat, fish • Intermediate moisture foods (15-50%) – Bread, hard cheeses, sausages • Low moisture foods (0-15%) – Dehydrated vegetables, grains, milk powder, dry soup mixes Importance of aw: Honey at 20% mc is shelf stable, while potato at 20% is not 2. Microbiology Classification of Bacteria • Based on Oxygen – Aerobes (Need oxygen for growth) • Microaerophile: Need only small amount of oxygen for growth – Anaerobes • Obligate: -

Elasticized Covers Technical Data
ELASTICIZED COVERS TECHNICAL DATA GENERAL DESCRIPTION STERIS Barrier Product Solutions (BPS) offers a comprehensive portfolio of autoclave bags, sterilization pouches, covers, and wrappers manufactured from Tyvek® non-woven spunbonded olefin material1. These products help to maximize efficiencies in production while maintaining a sterility barrier to protect surfaces of critical components and equipment. Customized and unique solutions are designed to save time, increase compliance, and reduce the risk of contamination. Please note that BPS products are not for use in the reprocessing of medical devices. BPS elasticized covers provide a fast, convenient way to protect open containers and parts during preparation for steam sterilization. Made from a flexible, drapeable form of Tyvek material, these covers are readily customized to fit a variety of products. For example, items may range from large, bulky stopper bowls to containers and parts with small openings, such as flasks, beakers, media bottles, valves, pipes, hoses, sanitary fittings, and carboys. The elastic allows the cover to be easily placed and ensures proper fit around the opening. The Tyvek material used in BPS elasticized covers is puncture-resistant, extremely durable, and ideally suited for steam sterilization in an autoclave. During sterilization, the Tyvek material allows for efficient air removal, steam penetration, and drying while serving as an effective microbial barrier. Moreover, after sterilization, these covers can remain in place on the parts up until they are put into use, thereby minimizing the risk of any subsequent contamination. FEATURES BENEFITS Low particulate generation.............................................................. Ideally suited for use in isolators, restricted access barrier systems (RABS), and ISO 5 cleanroom environments Breathable yet hydrophobic .......................................................... -
RTD's: Aseptic Vs. Retort Processing
RTD’s: Aseptic vs. (cooked) using the retort method, while the ahi tuna is fresh and uncooked. Retort Processing Additionally, the liquid in canned shakes are exposed Ready to Drink protein shakes {RTD} are typically made to metal inside of the can. And, when heated, it is possible using one of two processing methods – retort process- that metal residues may leech from the can and into the ing or aseptic processing. The processing method liquid – giving it a “metallic” taste. makes all the difference in the quality of the shake and ultimately, the results you can expect from using it. Aseptic Processing… By contrast, aseptic processing is a relatively Retort Processing… new and innovative food processing method Many protein/nutrition shakes on the market today are that uses the latest in food processing technology. packaged in metal cans – just like soda pop. Canned shakes are made using the retort processing method – a Aseptic processing differs from retort processing in that food processing method that’s over a century old. it involves minimal processing and heat exposure. Retort processing is a method whereby the canned shakes are sterilized by superheating them for 45 minutes at temperatures of up to 300 degrees Fahrenheit. This effectively sterilizes the cans and eliminates any bacteria and contamination. While heating the shakes for a long period of time effectively sterilizes both the metal can and the liquid inside, this excessive heat exposure (overcooking) – also does something else: it denatures the proteins in the shakes. You see, proteins are made of amino acids that link together and form chains called peptides. -

JBT Aseptic Processing & Packaging Solutions
Whats new at JBT? Aseptic Processing & Packaging Solutions JBT has long experience helping processors improve the quality and shelf life of their ambient shelf-stable products. As a matter of fact, more than 50% of the world’s shelf-stable foods are filled, seamed or sterilized using JBT equipment. With several thousand lines in operation worldwide, JBT is the world’s leading supplier of integrated processing solutions for metal, glass and plastic containers. From single machines to complete processing lines, JBT enhances product value and safety. JBT equipment preserves optimum quality, nutrition and taste in food products while producing them at the lowest cost per unit. Up till now JBT processing solutions were mainly geared towards ambient filling, closing and in-container processing. With the acquisition of Dutch company Stork Food & Dairy Systems in 2015, JBT now offers a comprehensive range of aseptic solutions to extend shelf life for more sensitive products. Integration of equipment cuts costs and improves quality, taste and food safety The key to Extended Shelf Life (ESL) and aseptic technology is hygiene. The shelf life of a chilled dairy product or juice, for example, cannot be extended without first raising levels of hygiene across the entire line. Although new processing and filling or packaging systems offer good opportunities for improving the hygiene level, no single piece of equipment will do the trick alone. ESL and aseptic packing is not just about technology and equipment; it is about a system, the success of which depends on the hygienic strength of the entire production and distribution chain. At the end of the production line, the quality and shelf life of products depend on effective processing, filling and packaging. -

Packaging, Storage and Distribution of Processed Milk
04/11/2011 packaging, storage and distribution of … packaging, storage and distribution of processed milk CONTENTS ANIMAL PRODUCTION AND HEALTH PAPER 11 technical requirements and their economic implications by wojciech b. tuszynski meat and milk development service animal production and health division D:/cd3wddvd/NoExe/…/meister10.htm 1/182 04/11/2011 packaging, storage and distribution of … edited by h.s. hall The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. M-26 D:/cd3wddvd/NoExe/…/meister10.htm 2/182 04/11/2011 packaging, storage and distribution of … ISBN 92-5-100566-4 The copyright in this book is vested in the Food and Agriculture Organization of the United Nations. The book may not be reproduced, in whole or in part, by any method or process, without written permission from the copyright holder. Applications for such permission, with a statement of the purpose and extent of the reproduction desired, should be addressed to the Director, Publications Division, Food and Agriculture Organization of the United Nations, Via delle Terme di Caracalla, 00100 Rome, Italy. FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome 1978 © FAO Hyperlinks to non-FAO Internet sites do not imply any official endorsement of or D:/cd3wddvd/NoExe/…/meister10.htm 3/182 04/11/2011 packaging, storage and distribution of … responsibility for the opinions, ideas, data or products presented at these locations, or guarantee the validity of the information provided. -

PQRI Aseptic Processing Working Group -Final Report
PQRI Aseptic Processing Working Group -Final Report- Aseptic Processing Work Group -Final Report- The PQRI Aseptic Processing Working Group has completed their work in accordance with the December 23rd, 2002 approved work plan. The working group completed its activities on March 10, 2003, 110 days from the date of it’s formation. The working group, comprised of 41 members, did an outstanding job of focusing on the specified topics and goals set forth in the work plan. Not all areas of the FDA’s concept paper “Sterile Drug Products Produced by Aseptic Processing” were discussed in this activity, but rather several specific areas that where identified as needing additional scientific input. As part of the work plan an industry survey was conducted to gather specific information regarding aseptic filling practices. The responses from over 45 aseptic filling sites were received and collated for use by the team. Since that date several additional surveys have been received. The complete survey results, including the additional surveys received, will be submitted for publication in the near future. The 8 clarifications and 10 recommendation developed by the working group are presented in this document and were developed based on the expert knowledge of the work group members, survey results, and publications where applicable. As Chairman of the Aseptic Processing Working Group, I would like to recognize, on behalf of PQRI, the outstanding dedication and contributions made by each one of the FDA, Industry, and Academia working group members. In addition, I would like to recognize and thank the working group members from the DMPQ in Office of Compliance at FDA, for their willingness to bring this topic into the PQRI framework and for their efforts to make this activity a success. -
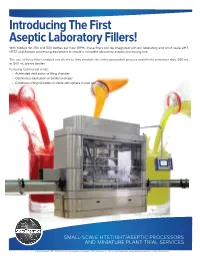
Introducing the First Aseptic Laboratory Fillers!
Introducing The First Aseptic Laboratory Fillers! With models for 250 and 500 bottles per hour (BPH), these fillers can be integrated with our laboratory and small scale UHT, HTST and Aseptic processing equipment to create a complete laboratory aseptic processing line. The use of these fillers enables our clients to truly simulate the entire production process and fill into consumer style 250 mL or 500 mL plastic bottles. Featuring Commercial Grade: • Automated sterilization of filling chamber • Continuous sterilization of bottles and caps • Continuous filling of bottles in sterile atmosphere in your lab! 500 bottle/hr. model shown SMALL-SCALE HTST/UHT/ASEPTIC PROCESSORS AND MINIATURE PLANT TRIAL SERVICES © MicroThermics 2016. MicroThermics is the registered trademark of MicroThermics, Inc. Aseptia and Aseptiwave are registered trademarks of Aseptia Corporation. MicroThermics, Inc. is proud to announce that we are the exclusive distributor of the X250 and X500 aseptic laboratory bottle fillers. Just like in production, these fillers go through a pre-process SIP procedure to fully sterilize the filling chamber, product lines, and X250 Aseptic Laboratory Filler filling heads. After the SIP, the process conditions are changed to Type Linear your product conditions, and the filler is started. It then sterilizes Approximate Cycle Time (App. Secs.) 15 and fills the bottle with your product directly from the processor. After processing, the filler is CIP cleaned with the processor. Bottles Per Hour (BPH) 250 Bottle Size* (mLs) 250 or 500 Finally- -
Success with Manual Aseptic Processing
12/6/16 Save the Date PDA Metro Chapter Day Symposium Tuesday, March 28, 2017 Auditing - 2017 Details soon at PDA.org, Chapters, Metro Success with Manual Aseptic Processing Jim Agalloco Agalloco & Associates Commercial Aseptic Filling © - Agalloco & Associates - 2016 1 12/6/16 Sterility by Design Best practice in aseptic processing is the application of a ‘Sterility By Design’ concept where the design & controls needed for success are selected to minimize the contamination risk. This is more difficult with manual aseptic ppgrocessing because the op pperator performs nearly all of the process and the ability to separate the operator from the sterile materials and surfaces is limited. Influences on Aseptic Processing Equipment API & Raw & Utensils Materials Containers &Cl& Closures Environment Product Procedures Air Supply People © - Agalloco & Associates - 2016 2 12/6/16 Aseptic Processing Definition “Handling sterile materials in a controlled environment, in which the air supply, facility, materials, equipment and personnel are regulated to control microbial and particulate contamination to acceptblltable level s.” PDA, TR# 22, 2011 revision Personnel & Contamination “It is useful to assume that the operator is always contaminated while operating in the aseptic area. If the procedures are viewed from this perspective, those practices which are exposing the product to contamination are more easily identified.” Hank Avallone – 1988 © - Agalloco & Associates - 2016 3 12/6/16 Manual Aseptic Processing Differs Aseptic processing on a commercial scale evolved substantially over the last 100 years. Thh’dhlle operator’s adverse impact has largely been mitigated by technological advances primarily in the areas of automation (reducing the need for operator intervention) and sepp(paration (the operator is moved farther away from sterile items).