Mid North Health Service Plan 2011 2020 FINAL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Australia Day 2020 Winners Announced Congratulations to the Following 2020 Australia Day Recipients
Serving Orroroo & Carrieton Region February 2020 Newsletter No. 289 FREE Australia Day 2020 Winners Announced Congratulations to the following 2020 Australia Day Recipients: Citizen of the Year – Kym, Christine & Heather Bertram Community Event of the Year – Orroroo Health Service Centenary Celebration Kym has also been a member of the Black Rock Dirt Circuit Club and has won a State Title representing the Club. Kym was also a member of the Orroroo Area School Governing Council when his children attended the school. Christine has also dedicated many years to the Orroroo Football Club and is still the Ladies representative with the Club’s Executive Committee and kitchen representative for the Football and Netball Clubs. Christine is a founding member of the Orroroo Carols in the Main Committee, assisting with the organisation Joint Citizens of the Year of the event each year which is a large community Christine and Kym Bertram, Mayor Kathie Bowman event in Orroroo each December and has just and Heather Bertram with their Award celebrated its 14th year. Kym, Christine and Heather Bertram of Orroroo have Christine is also the Booleroo Centre Pekina Parish been jointly awarded the District Council of Orroroo Pastoral Council Secretary and has volunteered many Carrieton Citizen of the Year for 2020 for their service hours to many organisations and functions assisting in to the community. catering and helping where she can. Together, Kym, Christine and Heather have operated Heather has been an excellent advocate of tourism the Orroroo Caravan Park since 2003. From that time within the district, encouraging visitors to stay longer and make a return trip. -

Mount Remarkable National Park About
<iframe src="https://www.googletagmanager.com/ns.html?id=GTM-5L9VKK" height="0" width="0" style="display:none;visibility:hidden"></iframe> Mount Remarkable National Park About Check the latest Desert Parks Bulletin (https://cdn.environment.sa.gov.au/parks/docs/desert-parks-bulletin- 30092021.pdf) before visiting this park. Within easy reach of Adelaide, Mount Remarkable National Park is an ideal place to take the family. There’s lots of diverse wildlife and campgrounds with good facilities. The park is a popular destination for bushwalking, with trails for all ages and abilities. There are some incredible views to be had – the 960m high Mount Remarkable Summit presides over the Willochra Plain and looks out to the Spencer Gulf. The Willowie Forest area offers a network of mountain biking and walking trails that meander through foothills of the Mount Remarkable Range. Please note that camping fees are changing in this park from Monday 22 March 2021. Opening hours Open daily. Closures and safety This park is closed on days of Catastrophic Fire Danger and may also be closed on days of Extreme Fire Danger. You can determine the current fire danger rating by checking the Fire Ban District map (https://www.cfs.sa.gov.au/site/bans_and_ratings.jsp) on the CFS website. Check the CFS website (https://www.cfs.sa.gov.au/site/home.jsp) or call the CFS Bushfire Information Hotline 1800 362 361 for: Information on fire bans and current fire conditions (https://www.cfs.sa.gov.au/site/bans_and_ratings.jsp) Current CFS warnings and incidents (https://www.cfs.sa.gov.au/site/warnings_and_incidents.jsp) Information on what to do in the event of a fire (https://www.cfs.sa.gov.au/site/prepare_for_a_fire.jsp). -

Country Housing Map
Country housing map This map shows the country areas in South Australia where public, Aboriginal and community housing is available. Use this map to select the areas you would be prepared to live in. If you want to register your interest in housing cooperatives, find the areas where housing cooperatives are available at www.sa.gov.au/housing SAHA Country Areas MAP Jan 2021 MAP Jan Country Areas SAHA Areas where housing is available are listed below. Some areas only have some types of housing available. Cottage flats are small public housing homes with 1 bedroom or a combined lounge and bedroom. Adelaide Hills region • Balhannah - Area 106 • Nairne - Area 184 • Littlehampton - Area 151 • Woodside - Area 233 • Mount Barker - Area 32 (Aldgate, Bridgewater, Crafers, Macclesfield, Mount Barker) Public housing only: • Brukunga - Area 112 • Lobethal - Area 152 • Hahndorf - Area 134 Community housing only: • Gumeracha - Area 241 • Ironbank - Area 551 Cottage flats only: • Echunga - Area 126 • Meadows - Area 161 Berri region • Barmera - Area 105 • Renmark - Area 206 • Berri - Area 108 • Waikerie - Area 226 • Loxton - Area 154 Public housing only: • Morgan - Area 181 Aboriginal housing only: • Glossop - Area 132 Cottage flats only: • Paringa - Area 193 Ceduna region Public housing only: • Ceduna - Area 115 • Streaky Bay - Area 216 • Thevenard - Area 247 Fleurieu Peninsula region • McCracken - Area 179 Community housing only: • Hayborough - Area 137 • Normanville - Area 187 • McHarg Creek - Area 426 • Port Elliott - Area 199 • Middleton - Area 164 -

River Health in the Mid North the Map Provides an Overall Assessment of the Health of Individual Sites in the Region
Mayfly nymph (Koorrnonga inconspicua) Aquatic macroinvertebrates in the Mid North The region is biologically diverse, with over 380 types of aquatic macroinvertebrates having been collected from 1994–1999. The most common members include amphipod crustaceans (e.g. Pseudomoera species and Austrochiltonia australis), blackfly larvae (Simulium ornatipes), oligochaetes (worms), chironomid midge larvae (Chironomus species), molluscs (hydrobiid snails) and nematodes (roundworms). A number of rare and uncommon macroinvertebrates are also found in the region. They include bristle worms (polychaete worms from the family Syllidae) found in the main channel of the Broughton River, as well as from the lower Rocky River and Mary Springs. These worms are normally found in marine and estuarine environments and their widespread presence in the Broughton catchment was unexpected. Other interesting records include horsehair worms (Gordiidae) from Skillogallee Creek, and planorbid snails (Gyraulus species) from the Light River at Mingays Waterhole. There are also three rare blackfly larvae that occur in the region: Austrosimulium furiosum from the Broughton River, Simulium melatum from Mary Springs and Paracnephia species from Belalie Creek. Among the rarer midges in the area are Podonomopsis from Eyre Creek, Apsectrotanypus from the Light River at Kapunda and Harrissius from the Wakefield River. Mayflies such as Offadens sp. 5 and Centroptilum elongatum, from the Broughton River and Mary Springs respectively, were unusual records, as were the presence of several caddisflies (e.g. Apsilochorema gisbum, Taschorema evansi, Orphninotrichia maculata and Lingora aurata) from Skillogallee and Eyre creeks, Mary Springs and the lower Broughton River. Mayfly nymphs (e.g. Koorrnonga inconspicua) have flattened bodies that allow them to cling to rocks in flowing streams. -

Department for Education and Child Development Preschools/Kindergartens
2017 Little Big Book Club Reading Packs - list of supporting services distributing the TODDLER READING PACK Department for Education and Child Development Preschools/Kindergartens Name of Preschool/Centre/Organisation Tel Address1 Address2 Suburb Pcode Napperby Preschool (1561) DECD (08) 8634 4309 c/- Napperby Primary Oaks Road Napperby 5540 School St Raphael’s School DECD 8272 2368 114 Glen Osmond Road Parkside 5063 Kangaroo Inn Preschool (1685) DECD (08) 8734 3046 c/- Kangaroo Inn Area 2329 Beachport Penola Road Kangaroo Inn 5280 School Elliston RSL Memorial CC (6616) DECD (08) 8687 9113 30 Memorial Drive Elliston 5670 Karoonda Preschool (1589) DECD (08) 8578 1120 c/- Karoonda Area School North Terrace Karoonda 5307 Rendelsham Preschool (6561) DECD (08) 8735 4237 Nilsson Street Rendelsham 5280 Miltaburra Children's Centre (6678) DECD (08) 8626 8086 c/- Miltaburra Area RSD 70 Miltaburra Road Streaky Bay 5680 School Wudinna RSL Memorial Kindergarten (6680) DECD (08) 8680 2252 Oswald Street Wudinna 5652 Kirinari Kindergarten (6540) DECD (08) 8738 7323 Sewarts Road Allendale East 5291 Barmera Kindergarten (6503) DECD (08) 8588 2210 Amy Street Barmera 5345 Berri Community Preschool (6505) DECD (08) 8582 1880 1A Fiedler Street Berri 5343 Booleroo Centre & District Kgtn (6608) DECD (08) 8667 2055 26 Campbell Street Booleroo Centre 5482 Renown Park Preschool (1450) DECD (08) 8346 4306 132 West Street Brompton 5007 Bute and District Kindergarten (6604) DECD (08) 8826 2230 4 Third Street Bute 5560 Callington Kindergarten (6560) DECD (08) 8538 -

Yorke and Mid North Regional Roadmap
Yorke and Mid North Regional Roadmap August 2014 1 Contents Page Message from the Chair ……………………………………………………………………………… 3 Executive Summary ……………………………………………………………………………… 4 How to Use this Roadmap ……………………………………………………………………………… 5 Our Vision for the Region ……………………………………………………………………………… 6 Analysis of the Region ……………………………………………………………………………… 9 Regional Priorities ……………………………………………………………………………… 45 Our Activities ……………………………………………………………………………… 48 Sources ……………………………………………………………………………… 67 2 Message from the Chair Regional Development Australia Yorke and Mid North (RDAYMN) was formed in February 2010 to support informed regional planning; consult and engage with stakeholders to identify and resolve critical issues; liaise with local governments and local communities about the best, most appropriate programs and services to support regional development; and contribute to business growth and investment plans, environmental solutions and social inclusion strategies. To achieve these objectives RDAYMN has identified six ‘Pillars of Strength and Support’ that we believe are essential to enhance our region’s development: 1. Economic Enhancement and Growth; 2. Infrastructure for the Future; 3. Growing a Vibrant Community with a Positive Future; 4. People Power: Developing Education, Knowledge and Skills; 5. Environmental Sustainability; 6. Regional Cohesion. One of our main activities is to work with Federal, State and Local Government partners as well as key stakeholders in the Yorke and Mid North region of South Australia to develop a comprehensive -

Australia Day 2019 Winners Announced
Serving Orroroo & Carrieton Region February 2019 Free Newsletter No. 279 Australia Day 2019 Winners Announced The traditional community breakfast attracted more than 150 people to celebrate Australia Day on January 26th at the Orroroo Lions Park. A beautiful sunny morning welcomed the crowd to the park, which was shaded by the many red gums - providing cool relief following a fortnight of extreme heat throughout the area. With stomachs filled, it was time for master of ceremonies Dylan Strong to commence with the program. In the official Australia Day address, Councillor Chairman Kathie Bowman reflected on resilience and the importance of recognition of community members. “Today here in Orroroo, we celebrate all that is good about this place and its people, even after a tough year”, “We celebrate what people, individuals and groups, have given this community over so very many years, and how fortunate we are to have benefited from their endeavours,” she said. Guest speaker and Australia Day Ambassador Peter Goers joined the festivities and entertained the crowd by recollecting his own experiences in the area. Mr Goers also assisted Chairman Bowman in in presenting the Australian Day awards to this year’s winners. Mr Malcolm Byerlee, flanked by his family, accepted the award for Citizen of the Year. Kate Case was the recipient of the Young Citizen of the Year, while the Paint Orroroo Pink event was awarded the Community Event of the Year. A special presentation to close the official proceedings included a Lighthorse display, by Mick Batchelor. Orroroo Carrieton Council CEO Dylan Strong cited the success of the event, which attracted a large crowd from across the district. -

Mid North Region Plan a Volume of the South Australian Planning Strategy
Mid North Region Plan A volume of the South Australian Planning Strategy May 2011 Mid North Region Plan A volume of the South Australian Planning Strategy This document is the Mid North Region Plan. The document has been prepared by the South Australian Government, through the Department of Planning and Local Government, as a volume of the South Australian Planning Strategy pursuant to section 22 of the Development Act 1993 and is subject to change. For further information Please visit www.dplg.sa.gov.au or telephone the Department of Planning and Local Government on 08 8303 0600. Disclaimer While every reasonable effort has been made to ensure that this document is correct at the time of publication, the Minister for Urban Development, Planning and the City of Adelaide, the State of South Australia, its agencies, instrumentalities, employees and contractors disclaim any and all liability to any person in respect to anything or the consequence of anything done or omitted to be done in reliance upon the whole or any part of this document. © Government of South Australia. Published 2011. All rights reserved. ISBN 978-0-7590-0138-1 FIS 23121 iii MiNiSteR foR URban DevelopmeNt, PlanniNg and the City of ADelAiDe South Australia’s Mid North is a diverse region, with some of the state’s most appealing tourist destinations and an economy underpinned by primary production and processing. The region is known for the wines of the Clare Valley, the rich history of towns like Burra, the agriculture that drives centres like Crystal Brooke and Peterborough, and the industry of Port Pirie. -

GRDC Southern Region Scoping Study
CSIRO AGRICULTURE AND FOOD GRDC Southern Region scoping study: Available soil information to support prediction of PAWC Output 3 Project CSP00210 Mark Thomas, Uta Stockmann, Kirsten Verburg, Jenet Austin, Mark Glover 31 May 2018 Prepared for Grains Research and Development Corporation Kaara Klepper, Manager Agronomy, Soils and Farming Systems - North Citation Thomas M, Stockmann U, Verburg K, Austin J, Glover M (2018) GRDC Southern Region scoping study: Available soil information to support prediction of PAWC. CSIRO, Australia. Copyright © Commonwealth Scientific and Industrial Research Organisation 2018. To the extent permitted by law, all rights are reserved and no part of this publication covered by copyright may be reproduced or copied in any form or by any means except with the written permission of CSIRO. Important disclaimer CSIRO advises that the information contained in this publication comprises general statements based on scientific research. The reader is advised and needs to be aware that such information may be incomplete or unable to be used in any specific situation. No reliance or actions must therefore be made on that information without seeking prior expert professional, scientific and technical advice. To the extent permitted by law, CSIRO (including its employees and consultants) excludes all liability to any person for any consequences, including but not limited to all losses, damages, costs, expenses and any other compensation, arising directly or indirectly from using this publication (in part or in whole) and any information or material contained in it. CSIRO is committed to providing web accessible content wherever possible. If you are having difficulties with accessing this document please contact [email protected]. -

Priority Towns Excerpt from the Health Workforce Needs Assessment
Priority Towns Excerpt from the Health Workforce Needs Assessment MMM SA3 Town MMM 5 Yorke Kadina PRIORITY 1 MMM 5 Barossa Kapunda MMM 7 Eyre & SW Wudinna MMM 5 Lower North Eudunda MMM 6 Eyre & SW Cowell MMM 4 Outback Port Augusta MMM 6 Eyre & SW Kimba MMM 4 Mid North Port Pirie MMM 6 Murray Lameroo MMM 3 Eyre Whyalla MMM 6 Murray Pinnaroo MMM 6 Eyre & SW Streaky Bay PRIORITY 3 MMM 5 Mid North Booleroo Centre MMM 6 Eyre & SW Coffin Bay MMM 5 Mid North Orroroo MMM 6 Eyre & SW Port Lincoln MMM 5 Outback Quorn MMM 5 Mid North Peterborough MMM 5 Murray Tailem Bend MMM 5 Mid North Jamestown MMM 5 Limestone Keith MMM 5 Limestone Naracoorte MMM 5 Limestone Penola MMM 5 Murray Barmera MMM 5 Murray Karoonda Aboriginal Community Controlled Health Services MMM 5 Murray Loxton MMM 6 ACCHS Port Lincoln MMM 5 Murray Mannum MMM 4 ACCHS Port Augusta MMM 5 Murray Renmark MMM 3 ACCHS Mount Gambier MMM 5 Yorke Ardrossan MMM 7 ACCHS Ceduna MMM 5 Yorke Maitland MMM 3 ACCHS Murray Bridge MMM 5 Yorke Minlaton MMM 6 ACCHS APY Lands MMM 5 Yorke Moonta MMM 3 ACCHS Whyalla MMM 5 Yorke Wallaroo MMM 7 ACCHS Oak Valley MMM 5 Lower Nth Burra MMM 3 ACCHS Mount Gambier MMM 5 Lower Nth Port Broughton MMM 4 ACCHS Port Augusta MMM 5 Lower Nth Riverton MMM 6 ACCHS Port Lincoln MMM 5 Lower Nth Balaklava MMM 7 ACCHS Yalata MMM 5 Lower Nth Clare MMM 7 ACCHS Coober Pedy MMM 5 Lower Nth Hamley Bridge MMM 5 Lower Nth Snowtown PRIORITY 2 MMM 5 Fleurieu Strathalbyn MMM 7 Outback Coober Pedy MMM 5 Fleurieu Yankalilla MMM 7 Eyre & SW Ceduna MMM 5 Barossa Angaston MMM 7 Eyre & SW Elliston -
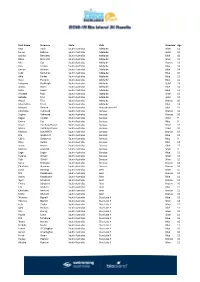
First Name Surname State Club Standard Age Mya Axon South
First Name Surname State Club Standard Age Mya Axon South Australia Adelaide Silver 11 Daniel Babovic South Australia Adelaide Gold 12 Jacinta Bennetts South Australia Adelaide Blue 16 Blake Bennetts South Australia Adelaide Silver 15 Mia Cox South Australia Adelaide Bronze 13 Ben Craven South Australia Adelaide Blue 16 Declan Hillman South Australia Adelaide Blue 14 Luke Kernahan South Australia Adelaide Blue 15 Alfie Parker South Australia Adelaide Blue 11 Tiara Pullinen South Australia Adelaide Blue 11 Indyanna Rashleigh South Australia Adelaide Gold 13 Ariana Ravell South Australia Adelaide Blue 14 Mika Ravell South Australia Adelaide Blue 11 Annabel Ryan South Australia Adelaide Silver 12 Isabelle Tran South Australia Adelaide Gold 12 Alyssa Tran South Australia Adelaide Bronze 10 Maximillian Trask South Australia Adelaide Blue 14 Mahaila Denton South Australia Alma Broken Hill Blue 13 Charlotte Ashmead South Australia Barossa Bronze 12 Sophie Ashmead South Australia Barossa Bronze 10 Kegan Coulter South Australia Barossa Gold 9 Emmy Cox South Australia Barossa Blue 9 Keian Curthoys-Davies South Australia Barossa Silver 12 Miella Curthoys-Davies South Australia Barossa Gold 10 Makayla DOCHERTY South Australia Barossa Bronze 13 Ella Goldsmith South Australia Barossa Blue 12 Claire Goldsmith South Australia Barossa Blue 9 Riley Hallett South Australia Barossa Blue 13 Saxon Kearns South Australia Barossa Blue 12 Matilda Lewcock South Australia Barossa Silver 9 Sage Logan South Australia Barossa Blue 11 Kyrene O'Neill South Australia -

Mid North and Yorke Peninsula
Mid North and Yorke Peninsula The region has a diverse industry structure, which has grown from a primary production base. Its natural and heritage assets offer potential for growth in tourism. Key infrastructure issues are ensuring transport access and water reliability to support social and economic development throughout the region. MID NORTH AND YORKE PENINSULA At a glance Area 33,009 km2 (3.36% of SA) Population 54,902 in 2001 (3.74% of SA) Aged < 15 20.72% against SA average of 19.57% Aged > 65 18.80% against SA average of 14.40% Demographic trends 2016 projection: 54,386 or 3.41% of SA Down 0.94% from 2001 Natural Resources Coastal and marine resources, diversity of mineral reserves, areas dedicated to national and conservation parks, arable land Key Industries Agriculture, wine, manufacturing, tourism, aquaculture and fishing, mining Sea ports Export ports at Ardrossan, Port Giles, Klein Point, Wallaroo 38 BUILDING SOUTH AUSTRALIA - INFRASTRUCTURE Principal Industries Tourism Agriculture The region features natural and built attractions including the wine industry, heritage sites, local produce, extensive Mid North And Yorke Peninsula The region produces grain (high protein wheat, malting coastline, numerous conservation parks and a wide variety barley), livestock (cattle feedlotting and fine wool), grapes, of recreational opportunities from diving to hiking, all within wine and vegetables. The viticuture and wine industry is close proximity of Adelaide. worth $159 million p.a. and expected to grow to $250 million p.a. over the next few years. The Mid North has mine heritage sites at Burra and includes the export-oriented Clare Valley region with its world-famous An increasing number of value-adding manufacturing vineyards and wineries.