FY 2015 Burma Country Operational Plan (COP) the Following Elements
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
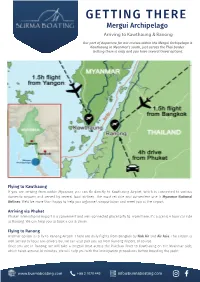
GETTING THERE Mergui Archipelago Arriving to Kawthaung & Ranong
GETTING THERE Mergui Archipelago Arriving to Kawthaung & Ranong Our port of departure for our cruises within the Mergui Archipelago is Kawthaung in Myanmar’s south, just across the Thai border. Getting there is easy and you have several travel options. Flying to Kawthaung If you are arriving from within Myanmar, you can fly directly to Kawthaung Airport, which is connected to various domestic airports and served by several local airlines. The most reliable and convenient one is Myanmar National Airlines. We’d be more than happy to help you organise transportation and meet you at the airport. Arriving via Phuket Phuket International Airport is a convenient and well-connected place to fly to. From there, it’s a scenic 4 hour car ride to Ranong. We can help you to book a car & driver. Flying to Ranong Another option is to fly to Ranong Airport. There are daily flights from Bangkok by Nok Air and Air Asia. The airport is well served by local taxi drivers but we can also pick you up from Ranong Airport, of course. Once you are in Ranong, we will take a longtail boat across the Pakchan River to Kawthaung on the Myanmar side, which takes around 30 minutes. We will help you with the immigration procedures before boarding the yacht. www.burmaboating.com +66 2 1070 445 [email protected] GETTING THERE Mergui Archipelago Crossing the Thai-Myanmar border In the case you arrive through the Thailand side and doesn’t want our assistance, here is a quick step by step instruction to cross the border between the 2 countries. -

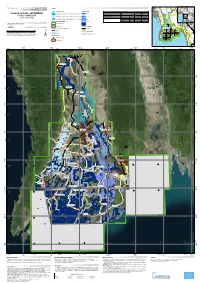
Usg Humanitarian Assistance to Burma
USG HUMANITARIAN ASSISTANCE TO BURMA RANGOON CITY AREA AFFECTED AREAS Affected Townships (as reported by the Government of Burma) American Red Cross aI SOURCE: MIMU ASEAN B Implementing NGO aD BAGO DIVISION IOM B Kyangin OCHA B (WEST) UNHCR I UNICEF DG JF Myanaung WFP E Seikgyikanaunglo WHO D UNICEF a WFP Ingapu DOD E RAKHINE b AYEYARWADY Dala STATE DIVISION UNICEF a Henzada WC AC INFORMA Lemyethna IC TI Hinthada PH O A N Rangoon R U G N O I T E G AYEYARWADY DIVISION ACF a U Zalun S A Taikkyi A D ID F MENTOR CARE a /DCHA/O D SC a Bago Yegyi Kyonpyaw Danubyu Hlegu Pathein Thabaung Maubin Twantay SC RANGOON a CWS/IDE AC CWS/IDE AC Hmawbi See Inset WC AC Htantabin Kyaunggon DIVISION Myaungmya Kyaiklat Nyaungdon Kayan Pathein Einme Rangoon SC/US JCa CWS/IDE AC Mayangone ! Pathein WC AC Î (Yangon) Thongwa Thanlyin Mawlamyinegyun Maubin Kyauktan Kangyidaunt Twantay CWS/IDE AC Myaungmya Wakema CWS/IDE Kyauktan AC PACT CIJ Myaungmya Kawhmu SC a Ngapudaw Kyaiklat Mawlamyinegyun Kungyangon UNDP/PACT C Kungyangon Mawlamyinegyun UNICEF Bogale Pyapon CARE a a Kawhmu Dedaye CWS/IDE AC Set San Pyapon Ngapudaw Labutta CWS/IDE AC UNICEF a CARE a IRC JEDa UNICEF a WC Set San AC SC a Ngapudaw Labutta Bogale KEY SC/US JCa USAID/OFDA USAID/FFP DOD Pyinkhayine Island Bogale A Agriculture and Food Security SC JC a Air Transport ACTED AC b Coordination and Information Management Labutta ACF a Pyapon B Economy and Market Systems CARE C !Thimphu ACTED a CARE Î AC a Emergency Food Assistance ADRA CWS/IDE AC CWS/IDE aIJ AC Emergency Relief Supplies Dhaka IOM a Î! CWS/IDE AC a UNICEF a D Health BURMA MERLIN PACT CJI DJ E Logistics PACT ICJ SC a Dedaye Vientiane F Nutrition Î! UNDP/PACT Rangoon SC C ! a Î ACTED AC G Protection UNDP/PACT C UNICEF a Bangkok CARE a IShelter and Settlements Î! UNICEF a WC AC J Water, Sanitation, and Hygiene WC WV GCJI AC 12/19/08 The boundaries and names used on this map do not imply official endorsement or acceptance by the U.S. -

46399E642.Pdf
PGDS in DOS Myanmar Atlas Map Population and Geographic Data Section As of January 2006 Division of Operational Support Email : [email protected] ((( Yüeh-hsi ((( ((( Zayü ((( ((( BANGLADESHBANGLADESH ((( Xichang ((( Zhongdian ((( Ho-pien-tsun Cox'sCox's BazarBazar ((( ((( ((( ((( Dibrugrh ((( ((( ((( (((Meiyu ((( Dechang THIMPHUTHIMPHU ((( ((( ((( Myanmar_Atlas_A3PC.WOR ((( Ningnan ((( ((( Qiaojia ((( Dayan ((( Yongsheng KutupalongKutupalong ((( Huili ((( ((( Golaghat ((( Jianchuan ((( Huize ((( ((( ((( Cooch Behar ((( North Gauhati Nowgong (((( ((( Goalpara (((( Gauhati MYANMARMYANMAR ((( MYANMARMYANMAR ((( MYANMARMYANMAR ((( MYANMARMYANMAR ((( MYANMARMYANMAR ((( MYANMARMYANMAR ((( Dinhata ((( ((( Gauripur ((( Dongch ((( ((( ((( Dengchuan ((( Longjie ((( Lalmanir Hat ((( Yanfeng ((( Rangpur ((( ((( ((( ((( Yuanmou ((( Yangbi((( INDIAINDIA ((( INDIAINDIA ((( INDIAINDIA ((( INDIAINDIA ((( INDIAINDIA ((( INDIAINDIA ((( ((( ((( ((( ((( ((( ((( Shillong ((((( Xundia ((( ((( Hai-tzu-hsin ((( Yongping ((( Xiangyun ((( ((( ((( Myitkyina ((( ((( ((( Heijing ((( Gaibanda NayaparaNayapara ((((( ((( (Sha-chiao(( ((( ((( ((( ((( Yipinglang ((( Baoshan TeknafTeknaf ButhidaungButhidaung (((TeknafTeknaf ((( ((( Nanjian ((( !! ((( Tengchong KanyinKanyin((( ChaungChaung !! Kunming ((( ((( ((( Anning ((( ((( ((( Changning MaungdawMaungdaw ((( MaungdawMaungdaw ((( ((( Imphal Mymensingh ((( ((( ((( ((( Jiuyingjiang ((( ((( Longling 000 202020 404040 BANGLADESHBANGLADESH((( 000 202020 404040 BANGLADESHBANGLADESH((( ((( ((( ((( ((( Yunxian ((( ((( ((( ((( -

The Government of the Republic of the Union of Myanmar
THE GOVERNMENT OF THE REPUBLIC OF THE UNION OF MYANMAR MINISTRY OF ELECTRICITY AND ENERGY NATIONAL ELECTRIFICATION PROJECT SPECIFIC PROCUREMENT NOTICE Date : 20th November, 2018 Invitation for Bids IDA, Credit No : 5727-MM Contract Title : Installation of Distribution Lines and Transformers for Mandalay and Adaptation Villages in Sagaing, Magway, Rakhine, Shan(North), Shan(South), Kayah, Bago(East), Bago(West), Naypyitaw, Mon, Kayin, Ayeyarwaddy and Yangon for National Electrification Project Reference No: MOEE-NEP/C1-W9/18 & MOEE-NEP/C1-W12/18 1. The Republic of the Union of Myanmar has received financing from the World Bank towards the cost of the National Electrification Project, and intends to apply part of the proceeds towards payments under the contract for Installation of Distribution Lines and Transformers MOEE- NEP/C1-W9/18 for Mandalay and MOEE-NEP/C1-W12/18 for Adaptation Villages in Sagaing, Magway, Rakhine, Shan (North), Shan (South), Kayah, Bago (East), Bago (West), Naypyitaw, Mon, Kayin, Ayeyarwaddy and Yangon. 2. The Ministry of Electricity and Energy now invites sealed bids from eligible bidders for Installation of Distribution Lines and Transformers MOEE-NEP/C1-W9/18 for Mandalay and MOEE-NEP/C1-W12/18 for Adaptation Villages in Sagaing, Magway, Rakhine, Shan (North), Shan (South), Kayah, Bago (East), Bago (West), Naypyitaw, Mon, Kayin, Ayeyarwaddy and Yangon in the following locations. The number and identification of lots comprising this installation bidding MOEE-NEP/C1-W9 /18 process for Mandalay is: Lot 1:Mandalay/Kyaukse/PyinOoLwin -

Bilin, Thaton, Kyaikto and Hpa- an Townships, September to November 2014
Situation Update February 10, 2015 / KHRG #14-101-S1 Thaton Situation Update: Bilin, Thaton, Kyaikto and Hpa- an townships, September to November 2014 This Situation Update describes events occurring in Bilin, Thaton, Kyaikto and Hpa-an townships, Thaton District during the period between September to November 2014, including armed groups’ activities, forced labour, restrictions on the freedom of movement, development activities and access to education. th • On October 7 2014, Border Guard Force (BGF) Battalion #1014 Company Commander Tin Win from Htee Soo Kaw Village ordered A---, B---, C--- and D--- villagers to work for one day. Ten villagers had to cut wood, bamboo and weave baskets to repair the BGF army camp in C--- village, Hpa-an Township. • In Hpa-an Township, two highways were constructed at the beginning of 2013 and one highway was constructed in 2014. Due to the construction of the road, villagers who lived nearby had their land confiscated and their plants and crops were destroyed. They received no compensation, despite reporting the problem to Hpa-an Township authorities. • In the academic year of 2013-2014 more Burmese government teachers were sent to teach in Karen villages. Villagers are concerned as they are not allowed to teach the Karen language in the schools. Situation Update | Bilin, Thaton, Kyaikto and Hpa-an townships, Thaton District (September to November 2014) The following Situation Update was received by KHRG in December 2014. It was written by a community member in Thaton District who has been trained by KHRG to monitor local human rights conditions. It is presented below translated exactly as originally written, save for minor edits for clarity and security.1 This report was received along with other information from Thaton District, including one incident report.2 This report concerns the situation in the region, the villagers’ feelings, armed groups’ activities, forced labour, development activities, support to villagers and education problems occurring between the beginning of September and November 2014. -

Military Brotherhood Between Thailand and Myanmar: from Ruling to Governing the Borderlands
1 Military Brotherhood between Thailand and Myanmar: From Ruling to Governing the Borderlands Naruemon Thabchumphon, Carl Middleton, Zaw Aung, Surada Chundasutathanakul, and Fransiskus Adrian Tarmedi1, 2 Paper presented at the 4th Conference of the Asian Borderlands Research Network conference “Activated Borders: Re-openings, Ruptures and Relationships”, 8-10 December 2014 Southeast Asia Research Centre, City University of Hong Kong 1. Introduction Signaling a new phase of cooperation between Thailand and Myanmar, on 9 October 2014, Thailand’s new Prime Minister, General Prayuth Chan-o-cha took a two-day trip to Myanmar where he met with high-ranked officials in the capital Nay Pi Taw, including President Thein Sein. That this was Prime Minister Prayuth’s first overseas visit since becoming Prime Minister underscored the significance of Thailand’s relationship with Myanmar. During their meeting, Prime Minister Prayuth and President Thein Sein agreed to better regulate border areas and deepen their cooperation on border related issues, including on illicit drugs, formal and illegal migrant labor, including how to more efficiently regulate labor and make Myanmar migrant registration processes more efficient in Thailand, human trafficking, and plans to develop economic zones along border areas – for example, in Mae 3 Sot district of Tak province - to boost trade, investment and create jobs in the areas . With a stated goal of facilitating border trade, 3 pairs of adjacent provinces were named as “sister provinces” under Memorandums of Understanding between Myanmar and Thailand signed by the respective Provincial governors during the trip.4 Sharing more than 2000 kilometer of border, both leaders reportedly understood these issues as “partnership matters for security and development” (Bangkok Post, 2014). -

Myanmar | Content | 1 Putao
ICS TRAVEL GROUP is one of the first international DMCs to open own offices in our destinations and has since become a market leader throughout the Mekong region, Indonesia and India. As such, we can offer you the following advantages: Global Network. Rapid Response. With a centralised reservations centre/head All quotation and booking requests are answered office in Bangkok and 7 sales offices. promptly and accurately, with no exceptions. Local Knowledge and Network. Innovative Online Booking Engine. We have operations offices on the ground at every Our booking and feedback systems are unrivalled major destination – making us your incountry expert in the industry. for your every need. Creative MICE team. Quality Experience. Our team of experienced travel professionals in Our goal is to provide a seamless travel experience each country is accustomed to handling multi- for your clients. national incentives. Competitive Hotel Rates. International Standards / Financial Stability We have contract rates with over 1000 hotels and All our operational offices are fully licensed pride ourselves on having the most attractive pricing and financially stable. All guides and drivers are strategies in the region. thoroughly trained and licensed. Full Range of Services and Products. Wherever your clients want to go and whatever they want to do, we can do it. Our portfolio includes the complete range of prod- ucts for leisure and niche travellers alike. ICS TRAVEL ICSGROUPTRAVEL GROUP Contents Introduction 3 Tours 4 Cruises 20 Hotels 24 Yangon 24 Mandalay 30 Bagan 34 Mount Popa 37 Inle Lake 38 Nyaung Shwe 41 Ngapali 42 Pyay 45 Mrauk U 45 Ngwe Saung 46 Excursions 48 Hotel Symbol: ICS Preferred Hotel Style Hotel Boutique Hotel Myanmar | Content | 1 Putao Lahe INDIA INDIA Myitkyina CHINA CHINA Bhamo Muse MYANMAR Mogok Lashio Hsipaw BANGLADESHBANGLADESH Mandalay Monywa ICS TRA VEL GR OUP Meng La Nyaung Oo Kengtung Mt. -
Irrawaddy Delta - MYANMAR Flooded Area Delineation 11/08/2015 11:46 UTC River R
Nepal (!Loikaw GLIDE number: N/A Activation ID: EMSR130 I Legend r n r India China e Product N.: 16IRRAWADDYDELTA, v2, English Magway a Rakhine w Bangladesh e a w l d a Vietnam Crisis Information Hydrology Consequences within the AOI on 09, 10, 11/08/2015 d Myanmar S Affected Total in AOI y Nay Pyi Taw Irrawaddy Delta - MYANMAR Flooded Area delineation 11/08/2015 11:46 UTC River R ha 428922,1 i v Laos Flooded area e ^ r S Flood - 01/08/2015 Flooded Area delineation 10/08/2015 23:49 UTC Stream Estimated population Inhabitants 4252141 11935674 it Bay of ( to Settlements Built-up area ha 35491,8 75542,0 A 10 Bago n Bengal Thailand y g Delineation Map e Flooded Area delineation 09/08/2015 11:13 UTC Lake y P Transportation Railways km 26,0 567,6 a Cambodia r i w Primary roads km 33,0 402,1 Andam an n a Gulf of General Information d Sea g Reservoir Secondary roads km 57,2 1702,3 Thailand 09 y Area of Interest ) Andam an Cartographic Information River Sea Missing data Transportation Bay of Bengal 08 Bago Tak Full color ISO A1, low resolution (100 dpi) 07 1:600000 Ayeyarwady Yangon (! Administrative boundaries Railway Kayin 0 12,5 25 50 Region km Primary Road Pathein 06 04 11 12 (! Province Mawlamyine Grid: WGS 1984 UTM Zone 46N map coordinate system Secondary Road 13 (! Tick marks: WGS 84 geographical coordinate system ± Settlements 03 02 01 ! Populated Place 14 15 Built-Up Area Gulf of Martaban Andaman Sea 650000 700000 750000 800000 850000 900000 950000 94°10'0"E 94°35'0"E 95°0'0"E 95°25'0"E 95°50'0"E 96°15'0"E 96°40'0"E 97°5'0"E N " 0 ' 5 -

Members of Parliament-Elect, Myanmar/Burma
To: Hon. Mr. Ban Ki-moon Secretary-General United Nations From: Members of Parliament-Elect, Myanmar/Burma CC: Mr. B. Lynn Pascoe, Under-Secretary-General, United Nations Mr. Ibrahim Gambari, Under-Secretary-General and Special Adviser to the Secretary- General on Myanmar/Burma Permanent Representatives to the United Nations of the five Permanent Members (China, Russia, France, United Kingdom and the United states) of the UN Security Council U Aung Shwe, Chairman, National League for Democracy Daw Aung San Suu Kyi, General Secretary, National League for Democracy U Aye Thar Aung, Secretary, Committee Representing the Peoples' Parliament (CRPP) Veteran Politicians The 88 Generation Students Date: 1 August 2007 Re: National Reconciliation and Democratization in Myanmar/Burma Dear Excellency, We note that you have issued a statement on 18 July 2007, in which you urged the State Peace and Development Council (SPDC) (the ruling military government of Myanmar/Burma) to "seize this opportunity to ensure that this and subsequent steps in Myanmar's political roadmap are as inclusive, participatory and transparent as possible, with a view to allowing all the relevant parties to Myanmar's national reconciliation process to fully contribute to defining their country's future."1 We thank you for your strong and personal involvement in Myanmar/Burma and we expect that your good offices mandate to facilitating national reconciliation in Myanmar/Burma would be successful. We, Members of Parliament elected by the people of Myanmar/Burma in the 1990 general elections, also would like to assure you that we will fully cooperate with your good offices and the United Nations in our effort to solve problems in Myanmar/Burma peacefully through a meaningful, inclusive and transparent dialogue. -

India-Myanmar-Bangladesh Border Region
MyanmarInform ationManage mUnit e nt India-Myanmar-Banglade shBord eRegion r April2021 92°E 94°E 96°E Digboi TaipiDuidam Marghe rita Bom dLa i ARUN ACHALPRADESH N orthLakhimpur Pansaung ARUN ACHAL Itanagar PRADESH Khonsa Sibsagar N anyun Jorhat INDIA Mon DonHee CHINA Naga BANGLA Tezpur DESH Self-Administered Golaghat Mangaldai Zone Mokokc hung LAOS N awgong(nagaon) Tuensang Lahe ASSAM THAILAND Z unhe boto ParHtanKway 26° N 26° Hojai Dimapur N 26° Hkamti N AGALAN D Kachin Lumd ing Kohima State Me huri ChindwinRiver Jowai INDIA LayShi Maram SumMaRar MEGHALAYA Mahur Kalapahar MoWaing Lut Karimganj Hom alin Silchar Imphal Sagaing ShwePyi Aye Region Kalaura MAN IPUR Rengte Kakc hing Myothit Banmauk MawLu Churachandpur Paungbyin Indaw Katha Thianship Tamu TRIPURA Pinlebu 24° N 24° W untho N 24° Cikha Khampat Kawlin Tigyaing Aizawal Tonzang Mawlaik Rihkhawdar Legend Ted im Kyunhla State/RegionCapital Serc hhip Town Khaikam Kalewa Kanbalu Ge neralHospital MIZORAM Kale W e bula TownshipHospital Taze Z e eKone Bord eCrossing r Falam Lunglei Mingin AirTransport Facility Y e -U Khin-U Thantlang Airport Tabayin Rangamati Hakha Shwebo TownshipBoundary SaingPyin KyaukMyaung State/RegionBoundary Saiha Kani BANGLA Budalin W e tlet BoundaryInternational Ayadaw MajorRoad Hnaring Surkhua DESH Sec ondaryRoad Y inmarbin Monywa Railway Keranirhat SarTaung Rezua Salingyi Chaung-U Map ID: MIMU1718v01 22° N 22° Pale Myinmu N 22° Lalengpi Sagaing Prod uctionApril62021 Date: Chin PapeSize r A4 : Projec tion/Datum:GCS/WGS84 Chiringa State Myaung SourcData Departme e : ofMe nt dService ical s, Kaladan River Kaladan TheHumanitarian ExchangeData Matupi Magway BasemMIMU ap: PlaceName General s: Adm inistrationDepartme (GAD)and field nt Cox'sBazar Region sourcTransliteration e s. -

Gulf of Mottama Management Plan
GULF OF MOTTAMA MANAGEMENT PLAN PROJECT IMPLEMTATION AND COORDINATION UNIT – PCIU COVER DESIGN: 29, MYO SHAUNG RD, TAUNG SHAN SU WARD, MAWLAMYINE, NYANSEIK RARMARN MON STATE, MYANMAR KNOWLEDGE MANAGEMENT AND COMMUNICATION OFFICER GULF OF MOTTAMA PROJECT (GOMP) Gulf of Mottama Management Plan, May 2019 GULF OF MOTTAMA MANAGEMENT PLAN Published: 16 May 2019 This management plan is endorsed by Mon State and Bago Regional Governments, to be adopted as a guidance document for natural resource management and sustainable development for resilient communities in the Gulf of Mottama. 1 Gulf of Mottama Management Plan, May 2019 This page is intentionally left blank 2 Gulf of Mottama Management Plan, May 2019 Gulf of Mottama Project (GoMP) GoMP is a project of Swiss Agency for Development and Cooperation (SDC) and is implemented by HELVETAS Myanmar, Network Activities Group (NAG), International Union for Conservation of Nature (IUCN), and Biodiversity and Nature Conservation Association(BANCA). 3 Gulf of Mottama Management Plan, May 2019 ACKNOWLEDGEMENTS The drafting of this Gulf of Mottama Management Plan started early 2016 with an integrated meeting on May 31 to draft the first concept. After this initial workshop, a series of consultations were organized attended by different people from several sectors. Many individuals and groups actively participated in the development of this management plan. We would like to acknowledge the support of the Ministries and Departments who have been actively involved at the Union level which more specifically were Ministry of Natural Resource and Environmental Conservation, Ministry of Agriculture, Livestock and Irrigation, Forest Department, Department of Agriculture, Department of Fisheries, Department of Rural Development and Environmental Conservation Department. -

Mimu866v01 120525 3W Education South East Region(Pie) A3
Myanmar Information Management Unit 3W South East of Myanmar Education Border and Country Based Organizations Presence by Township Budalin 94°23'EKani 96°4'E Kyaukme 97°45'E Pangsang 99°26'E 101°7'E Thantlang Ayadaw Wetlet Mongyai Hakha Madaya Nawnghkio Yinmabin SAGAING Hsipaw Tangyan Gangaw Monywa Sagaing Mandalay Pale Myinmu Salingyi .! Pyinoolwin Mongyang Madupi Sagaing .! Mongkaung Kyethi Monghsu Matman CHINA Ngazun Tilin Tada-U 1 2 1 CHIN Lawksawk 1 Mongkhet Myaing Yesagyo Kyaukse Myingyan 1 Mongla Mindat Pauk Natogyi Myittha Ywangan Laihka Kengtung 2 Mongyawng Pakokku 1 Hopong Saw Taungtha Kunhing 2 Wundwin Mongping Ü Seikphyu Nyaung-U Mahlaing Loilen Pindaya Monghpyak 21°6'N Paletwa Kanpetlet 1 2 21°6'N MANDALAY 1 2 Nansang 1 Thazi Taunggyi 1 SHAN (EAST) Kyaukpadaung Meiktila Tachileik Chauk Kalaw .!Taunggyi Salin Monghsat 2 Pyawbwe 3 2 1 Mongnai 2 Minbya Sidoktaya Yenangyaung Natmauk Nyaungshwe SHAN (SOUTH) Yamethin Pwintbyu Hsihseng 2 1 Mongton MAGWAY 2 1 Sittwe Pinlaung 2 LAOS Magway Myothit Nay Pyi Mawkmai Mongpan Minbu .! Taw-Tatkon 3 Langkho Myebon Magway 1 1 Ngape Nay Pyi Taw Taungdwingyi Ann Loikaw [(! Pekon Loikaw Minhla Nay Pyi .! 1 Nay Pyi Taw-Pyinmana 4 Sinbaungwe 5 Taw-Lewe Demoso Shadaw RAKHINE 1 1 1 Thayet Mindon Hpruso 19°25'N Aunglan 19°25'N Yedashe 1 1 KAYAH Thandaunggyi Bawlakhe Ramree Taungoo Toungup Kamma 2 2 Paukkhaung 2 Hpasawng Pyay Htantabin 1 Oktwin 1 2 Mese Padaung Thegon Nattalin BAGO (EAST)1 Phyu Kyaukkyi BAGO (WEST) 1 Thandwe 3 Kyangin Kyauktaga Hpapun Okpho 2 Myanaung 2 2 Shwegyin Minhla 3 Ingapu