National Elective Surgery Urgency Categorisation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Empysema
Surgical Management of Empysema John A Odell MB ChB, FRCS(Ed), FACS Emeritus Professor of Surgery Mayo Clinic College of Medicine Previously Surgical Director Lung Transplantation ©2013 MFMER | slide-1 Problem case. How would you manage? • 64yr male • Previous RLL bullectomy. • Recent left pneumothorax managed elsewhere with chest tube placement. • Because of continued air-leak talc pleurodesis. • Air-leak continues. ©2013 MFMER | slide-2 • On nasal oxygen. Dyspneic on walking • Significant air-leak. More dyspneic when suction applied to chest drain. • FEV1 40% predicted. DLCO 12% predicted. Options? • Thoracotomy and close air leak surgically • Videothoracoscopy and closure of air-leak • Thoracotomy and decortication • Remove chest drain • List for transplantation Historical Treatment of Emphysema • Abdominal compression belts. The stimulus was the observation that emphysematous patients lean forward when breathing. • Pneumoperitoneum. In an attempt to restore diaphragmatic curvature. • Lungs too large for the chest – costochondrectomy or transverse sternotomy to provide more room. Multiple wedge excisions. • Chest grown too large – thoracoplasty • Pleurodesis. Emphysema results from alveolar wall ischemia. • Phrenectomy. Overvigerous inspiration was ripping alveolar walls. • Hilar denervation. To decrease bronchoconstriction and mucous production mediated by the parasympathetic nervous system. • Whole lung irradiation. To increase elastic recoil by inducing fibrosis. ©2013 MFMER | slide-7 Variants of Emphysema that may be Surgically -

Effect of an Indwelling Pleural Catheter Vs Talc Pleurodesis On
This supplement contains the following items: 1. Original protocol, final protocol, summary of changes. 2. Original statistical analysis plan. There were no further changes to the original statistical analysis plan. Downloaded From: https://jamanetwork.com/ on 10/02/2021 The Australasian Malignant Pleural Effusion Trial (AMPLE) A Multicentre Randomized Study Comparing Indwelling Pleural Catheter vs Talc Pleurodesis in Patients with Malignant Pleural Effusions Ethics Registration number 2012-005 Protocol version number 1.0 Protocol date 10/01/2012 Authorised by: Name: Prof YC Gary Lee Role: Chief Investigator Signature: Date: 10/01/2012 Downloaded From: https://jamanetwork.com/ on 10/02/2021 General Information This document describes the Western Australian Randomised Malignant Effusion trial for the purpose of submission for review by the relevant human research and ethics committees. It provides information about procedures for entering patients into the trial and this protocol should not be used as a guide for the treatment of other patients; every care was taken in its drafting, but corrections or amendments may be necessary. Questions or problems relating to this study should be referred to the Chief Investigator or Trial Coordinator. Compliance The trial will be conducted in compliance with this protocol, the National Statement on Ethical Conduct in Human Research, data protection laws and other guidelines as appropriate. It will be registered with the Australia and New Zealand Clinical Trials Registry, once ethical approval is secured. -

Acr–Scbt-Mr–Spr–Str Practice Parameter for the Performance of Thoracic Computed Tomography (Ct)
p The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2018 (Resolution 7)* ACR–SCBT-MR–SPR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF THORACIC COMPUTED TOMOGRAPHY (CT) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

2019 Coding and Payment Information Pleural Effusions and Ascites Management
2019 coding and payment information Pleural effusions and ascites management The information contained in this document, including Reimbursement rates shown are Medicare national the codes supplied, is provided for informational payments for 2019 and do not reflect actual payments purposes only. BD makes no statement, promise or made to individual providers, as payments are adjusted guarantee concerning the appropriateness of any codes specific to particular geographic regions. for a particular procedure, actual levels of All information is subject to change without notice. In reimbursement, payment or charge or that addition, payers or local carriers may have their own reimbursement will be made. coding and billing requirements. Consult your payer This is not intended to be a comprehensive guide to all organization with regard to local reimbursement policies. coding and payment information. 2019 Medicare outpatient facility rates CPT® 2019 APC OPPS 2019 ASC Description APC Status code base rate* base rate Pleural catheter procedures 32550 Insertion of indwelling tunneled pleural catheter 5341 J1 $2,947 $1,790 32552 Removal of indwelling tunneled pleural catheter with cuff 5181 Q2 $620 $319 32560 Instillation via chest tube/catheter, agent for pleurodesis 5181 T $620 N/A 32650 Thoracoscopy, surgical, with pleurodesis (e.g., mechanical or chemical) N/A; inpatient procedure Peritoneal catheter procedures Insertion of tunneled intraperitoneal catheter (e.g., dialysis, intraperitoneal chemotherapy instillation, management of ascites), 49418 -
FAQ Document
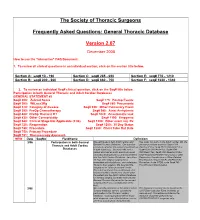
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -
Update in Anaesthesia
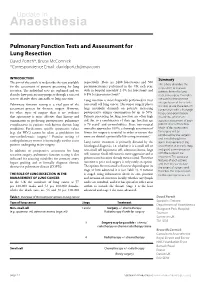
Update in Anaesthesia Pulmonary Function Tests and Assessment for Lung Resection David Portch*, Bruce McCormick *Correspondence Email: [email protected] INTRODUCTION Summary respectively. There are 2400 lobectomies and 500 The aim of this article is to describe the tests available This article describes the for the assessment of patients presenting for lung pneumonectomies performed in the UK each year, steps taken to evaluate resection. The individual tests are explained and we with in-hospital mortality 2-4% for lobectomy and patients’ fitness for lung 4 describe how patients may progress through a series of 6-8% for pneumonectomy. resection surgery. Examples tests to identify those amenable to lung resection. Lung resection is most frequently performed to treat are used to demonstrate interpretation of these tests. Pulmonary function testing is a vital part of the non-small cell lung cancer. This major surgery places It is vital to use these tests in assessment process for thoracic surgery. However, large metabolic demands on patients, increasing conjunction with a thorough for other types of surgery there is no evidence postoperative oxygen consumption by up to 50%. history and examination that spirometry is more effective than history and Patients presenting for lung resection are often high in order to achieve an examination in predicting postoperative pulmonary risk due to a combination of their age (median age accurate assessment of each complications in patients with known chronic lung is 70 years)5 and co-morbidities. Since non-surgical patient’s level of function. conditions. Furthermore specific spirometric values mortality approaches 100%, a thorough assessment of Much of this assessment (e.g. -

Agenda Item 5
List A (O) Respiratory system treatments and procedures. (1) Biopsy and/or excision (removal) of lesion of larynx, vocal cords, trachea (A) Loss or change of voice. (B) Swallowing or breathing difficulties. (C) Perforation (hole) or fistula (connection) in esophagus (tube from throat to stomach). (2) Rhinoplasty (surgery to change the shape of the nose) or nasal reconstruction with or without septoplasty A) Deformity of skin, bone or cartilage. (B) Creation of new problems, such as perforation of the nasal septum (hole in wall between the right and left halves of the nose) or breathing difficulty. (3) Submucous resection of nasal septum or nasal septoplasty (surgery to remove blockage in or straighten the nose) (A) Persistence, recurrence or worsening of the obstruction. (B) Perforation of nasal septum (hole in wall between the right and left halves of the nose) with dryness and crusting. (C) External deformity of the nose. (4) Sinus surgery/endoscopic sinus surgery (A) Spinal fluid leak (B) Visual loss or other eye injury (C) Numbness in front teeth and palate (D) Loss or reduction in sense of taste or smell (E) Recurrence of disease (F) Empty Nose Syndrome (sensation of nasal congestion, sensation of not being able to take in adequate air through nose) (G) Injury to tear duct causing drainage of tears down the cheek (H) Brain injury and/or infection (I) Injury to nasal septum (J) Nasal obstruction (5) Lung biopsy (A) Air leak with pneumothorax (leak of air from lung to inside of chest causing the lung to collapse) with need for insertion of chest drainage tube into space between lung and chest wall or repeat surgery. -

Core Curriculum for Surgical Technology Sixth Edition
Core Curriculum for Surgical Technology Sixth Edition Core Curriculum 6.indd 1 11/17/10 11:51 PM TABLE OF CONTENTS I. Healthcare sciences A. Anatomy and physiology 7 B. Pharmacology and anesthesia 37 C. Medical terminology 49 D. Microbiology 63 E. Pathophysiology 71 II. Technological sciences A. Electricity 85 B. Information technology 86 C. Robotics 88 III. Patient care concepts A. Biopsychosocial needs of the patient 91 B. Death and dying 92 IV. Surgical technology A. Preoperative 1. Non-sterile a. Attire 97 b. Preoperative physical preparation of the patient 98 c. tneitaP noitacifitnedi 99 d. Transportation 100 e. Review of the chart 101 f. Surgical consent 102 g. refsnarT 104 h. Positioning 105 i. Urinary catheterization 106 j. Skin preparation 108 k. Equipment 110 l. Instrumentation 112 2. Sterile a. Asepsis and sterile technique 113 b. Hand hygiene and surgical scrub 115 c. Gowning and gloving 116 d. Surgical counts 117 e. Draping 118 B. Intraoperative: Sterile 1. Specimen care 119 2. Abdominal incisions 121 3. Hemostasis 122 4. Exposure 123 5. Catheters and drains 124 6. Wound closure 128 7. Surgical dressings 137 8. Wound healing 140 1 c. Light regulation d. Photoreceptors e. Macula lutea f. Fovea centralis g. Optic disc h. Brain pathways C. Ear 1. Anatomy a. External ear (1) Auricle (pinna) (2) Tragus b. Middle ear (1) Ossicles (a) Malleus (b) Incus (c) Stapes (2) Oval window (3) Round window (4) Mastoid sinus (5) Eustachian tube c. Internal ear (1) Labyrinth (2) Cochlea 2. Physiology of hearing a. Sound wave reception b. Bone conduction c. -

Post-Pneumonectomy Bronchopleural Fistula
9 Review Article Page 1 of 9 Complications of thoracic surgery: post-pneumonectomy bronchopleural fistula Anuj Wali1, Andrea Billè1,2 1Thoracic Surgery Department, Guy’s Hospital, London, UK; 2Division of Cancer Studies, King’s College London Faculty of Life Sciences & Medicine at Guy’s, Kings College and St. Thomas’ Hospitals, London, UK Contributions: (I) Conception and design: All authors; (II) Administrative support: A Billè; (III) Provision of study materials or patients: A Wali; (IV) Collection and assembly of data: A Wali; (V) Data analysis and interpretation: A Wali; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Andrea Billè. Thoracic Surgery Department, Guy’s Hospital, 6th Floor, Borough Wing, London SE1 9RT, UK. Email: [email protected]. Abstract: Bronchopleural fistula (BPF) describes an abnormal connection between a bronchus (main, lobar or segmental) and the pleural cavity. BPF is a recognized complication after pneumonectomy and is associated with significant morbidity and mortality. The risk of post-pneumonectomy BPF (PP-BPF) is greater in right sided operations, male patients, residual tumor, barotrauma, previous TB and active infection. If suspected, diagnosis of BPF should be made expeditiously with computed tomography scanning and bronchoscopy. The management depends on the timing of presentation, the size of the fistula and the clinical status of the patient. All patients require drainage of the infected pleural space and intravenous antibiotics. In early presentations, re-do thoracotomy followed by stump closure and reinforcement with a pedicled muscle flap is recommended. If the fistula is small (<5 mm) or the patient is not fit enough for major surgery, bronchoscopic repair using fibrin glue application, stents or closure devices can be attempted. -

Hyperbaric Medicine Center During the Actual Questions About the Treatment Process Are Treatment Process, for All Patients’ Confidentiality, No Always Welcomed
Patient Label / Name HBO - HYPERBARIC OXYGEN PATIENT EDUCATION - Page | 1 FAQs HBO is a medical treatment which enhances the body’s natural healing process by inhalation of 100% oxygen in a total body chamber, where atmospheric pressure is WHAT IS HBO? increased and controlled. It is used for a wide variety of treatments usually as an adjunctive part of an overall HBO or HBOT stands for: Hyperbaric Oxygen Therapy medical care plan that can be done on an inpatient or WHAT DOES IT DO? outpatient basis. HBO or HBOT, simply, HBOT is a means of providing WAIT! CAN YOU TELL ME MORE ABOUT THE additional oxygen to your body tissues. “ENTIRELY CLOSED PRESSURE CHAMBER”? HOW DOES IT WORK? Your entire body will go in a closely monitored, TRANSPARENT, 100% ACRYLIC topped, sealed chamber. By exposing the Most patients have plenty of room to get comfortable entire body to and can enjoy their 1.5-2 hour treatments while watching oxygen under TV (installed on each chamber with internal speakers) or increased napping. atmospheric A highly qualified Hyperbaric Tech will be in the room pressure. with you at all times during your treatment, and you will be closely monitored before, during and after all HBO The patient is entirely enclosed in a pressure chamber Treatments. breathing 100% oxygen (O2) at greater than one atmosphere HBO Chambers have microphones that allow your HBO (atm) pressure. Tech to hear you without need to push any buttons. SO, HOW DOES THAT HELP? Simply call out and you will be heard. If you should need to cut your treatment short or want to get out at any HBO therapy serves 4 PRIMARY FUNCTIONS: time, your HBO Tech is always right there to safely decompress the chamber and help you out and call for 1. -
Both Left Upper Lobectomy and Left Pneumonectomy Are Risk Factors For
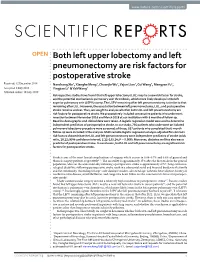
www.nature.com/scientificreports OPEN Both left upper lobectomy and left pneumonectomy are risk factors for postoperative stroke Received: 12 December 2018 Nanchang Xie1, Xianghe Meng1, Chuanjie Wu2, Yajun Lian1, Cui Wang3, Mengyan Yu1, Accepted: 8 July 2019 Yingjiao Li1 & Yali Wang1 Published: xx xx xxxx Retrospective studies have found that left upper lobectomy (LUL) may be a new risk factor for stroke, and the potential mechanism is pulmonary vein thrombosis, which more likely develops in the left superior pulmonary vein (LSPV) stump. The LSPV remaining after left pneumonectomy is similar to that remaining after LUL. However, the association between left pneumonectomy, LUL, and postoperative stroke remains unclear. Thus, we sought to analyze whether both LUL and left pneumonectomy are risk factors for postoperative stroke. We prospectively included consecutive patients who underwent resection between November 2016 and March 2018 at our institution with 6 months of follow-up. Baseline demographic and clinical data were taken. A logistic regression model was used to determine independent predictors of postoperative stroke. In our study, 756 patients who underwent an isolated pulmonary lobectomy procedure were screened; of these, 637 patients who completed the 6-month follow-up were included in the analysis. Multivariable logistic regression analysis adjusted for common risk factors showed that the LUL and left pneumonectomy were independent predictors of stroke (odds ratio, 18.12; 95% confdence interval, 2.12–155.24; P = 0.008). Moreover, diabetes mellitus also was a predictor of postoperative stroke. In conclusion, both LUL and left pneumonectomy are signifcant risk factors for postoperative stroke. Stroke is one of the most feared complications of surgery, which occurs in 0.08–0.7% and 0.6% of general and thoracic surgery patients, respectively1–3. -

Treatment of Post Pneumonectomy Pleural Empyema by Open Window Thoracostomy
Eur Respir J 1989, 2, 853-855 Treatment of post pneumonectomy pleural empyema by open window thoracostomy P.E. Postmus*, J.M. Kerstjens,* W.J. de Boer*, J.N. Homan van der Heide*, G.H. KoE:Her* Treatmenl of post pneumonectomy pleural empyema by open window thora Dcpts of Pulmonary Diseases' , and Thoracic costomy. P.E. Postmus, J.M. Kerstjens, W.J. de Boer, JN. Homan van der Surgery "· University Hospital, Groningen, The Heide, GH. Koiiter. Netherlands. ABSTRACT: In 13 patients an open window thoracostomy (OWT) was Correspondence: P.E. Postmus, Dept of Pulmonol· performed for post pneumonectomy pleural empyema. The operation, and ogy, University Hospital, 59 Oostersingel, 9713 EZ life with an OWT cavity, were tolerated well. Early closure of an OWT Groningen, The Netherlands. is not advisable because of a high chance of recurrence of the infection and, In lung cancer patients also the risk of tumour relapse within two Keywords: Emphyema: pneumonectomy; window years after tumour surgery. thoracostomy. Eur Respir J., 1989, 2, 853-855 Received: November 14, 1988; accepted after revi sion February 2, 1989. Post pneumonectomy empyema with or without a Subsequenlly the cavity is thoroughly cleaned from bronchopleural fistula represents a rare but, without debris and necrotic tissue, whereupon the edges of the doubt, serious complication of thoracic surgery. skin are sutured onto Ll1e edges of the parietal pleura. In the majority of patients the infection will resolve After a check for bronchopleural fistulae and filling of after systemic antibiotics, adequate tube drainage and ir the cavity with moist gauze pads, the patient is extu rigation with or without lavage [I) and/or local instil bated.