Subjective Refraction and Prescribing Glasses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prevention of Traumatic Corneal Ulcer in South East Asia
FROM OUR SOUTH ASIA EDITION Prevention of traumatic corneal ulcer in South East Asia S C AE Srinivasan/ (c)M Country Principal Investigator and Lead Principal Investigator with village health workers in Bhutan Dr. M. Srinivasan ciasis, and leprosy, are declining, and (VVHW) of the Government were utilized Director Emeritus, Aravind Eye Care, soon the majority of corneal blindness will to identify ocular injury and treat corneal Madurai, Tamil Nadu India. be due to microbial keratitis. Most abrasion corneal ulcers occur among agricultural Myanmar: Village Health Workers (VHW) workers in developing countries following of the health department Introduction corneal abrasion. India: paid village volunteers were utilized Corneal ulceration is a leading cause of Several non-randomized prevention visual impairment globally, with a dispro- studies conducted before 2000 Inclusion criteria 2 portionate burden in developing (Bhaktapur Eye Study) and during 2002 • Resident of study area countries. It was estimated that 6 million to 2004 in India, Myanmar, and Bhutan • Corneal abrasion after ocular injury, corneal ulcers occur annually in the ten by World Health Organization(WHO), have confirmed by clinical examination with countries of South East Asia Region suggested that antibiotic ointment fluorescein stain and a blue torch encompassing a total population of 1.6 applied promptly after a corneal abrasion • Reported within 48 hours of the injury billion.1 While antimicrobial treatment is could lower the incidence of ulcers, • Subject aged >5 years of age generally effective in treating infection, relative to neighbouring or historic “successful” treatment is often controls.3-4 Prevention of traumatic Exclusion criteria associated with a poor visual outcome. -

History of Refractive Surgery
History of Refractive Surgery Refractive surgery corrects common vision problems by reshaping the cornea, the eye’s outermost layer, to bend light rays to focus on the retina, reducing an individual’s dependence on eye glasses or contact lenses.1 LASIK, or laser-assisted in situ keratomileusis, is the most commonly performed refractive surgery to treat myopia, hyperopia and astigmatism.1 The first refractive surgeries were said to be the removal of cataracts – the clouding of the lens in the eye – in ancient Greece.2 1850s The first lensectomy is performed to remove the lens 1996 Clinical trials for LASIK begin and are approved by the of the eye to correct myopia.2 Food & Drug Administration (FDA).3 Late 19th 2 Abott Medical Optics receives FDA approval for the first Century The first surgery to correct astigmatism takes place. 2001 femtosecond laser, the IntraLase® FS Laser.3 The laser is used to create a circular, hinged flap in the cornea, which allows the surgeon access to the tissue affecting the eye’s 1978 Radial Keratotomy is introduced by Svyatoslov Fyodorov shape.1 in the U.S. The procedure involves making a number of incisions in the cornea to change its shape and 2002 The STAR S4 IR® Laser is introduced. The X generation is correct refractive errors, such as myopia, hyperopia used in LASIK procedures today.4 and astigmatism.2,3 1970s Samuel Blum, Rangaswamy Srinivasan and James J. Wynne 2003 The FDA approves the use of wavefront technology,3 invent the excimer laser at the IBM Thomas J. Watson which creates a 3-D map of the eye to measure 1980s Research Center in Yorktown, New York. -

Hydraulic Cylinder Replacement for Cylinders with 3/8” Hydraulic Hose Instructions
HYDRAULIC CYLINDER REPLACEMENT FOR CYLINDERS WITH 3/8” HYDRAULIC HOSE INSTRUCTIONS INSTALLATION TOOLS: INCLUDED HARDWARE: • Knife or Scizzors A. (1) Hydraulic Cylinder • 5/8” Wrench B. (1) Zip-Tie • 1/2” Wrench • 1/2” Socket & Ratchet IMPORTANT: Pressure MUST be relieved from hydraulic system before proceeding. PRESSURE RELIEF STEP 1: Lower the Power-Pole Anchor® down so the Everflex™ spike is touching the ground. WARNING: Do not touch spike with bare hands. STEP 2: Manually push the anchor into closed position, relieving pressure. Manually lower anchor back to the ground. REMOVAL STEP 1: Remove the Cylinder Bottom from the Upper U-Channel using a 1/2” socket & wrench. FIG 1 or 2 NOTE: For Blade models, push bottom of cylinder up into U-Channel and slide it forward past the Ram Spacers to remove it. Upper U-Channel Upper U-Channel Cylinder Bottom 1/2” Tools 1/2” Tools Ram 1/2” Tools Spacers Cylinder Bottom If Ram-Spacers fall out Older models have (1) long & (1) during removal, push short Ram Spacer. Ram Spacers 1/2” Tools bushings in to hold MUST be installed on the same side Figure 1 Figure 2 them in place. they were removed. Blade Models Pro/Spn Models Need help? Contact our Customer Service Team at 1 + 813.689.9932 Option 2 HYDRAULIC CYLINDER REPLACEMENT FOR CYLINDERS WITH 3/8” HYDRAULIC HOSE INSTRUCTIONS STEP 2: Remove the Cylinder Top from the Lower U-Channel using a 1/2” socket & wrench. FIG 3 or 4 Lower U-Channel Lower U-Channel 1/2” Tools 1/2” Tools Cylinder Top Cylinder Top Figure 3 Figure 4 Blade Models Pro/SPN Models STEP 3: Disconnect the UP Hose from the Hydraulic Cylinder Fitting by holding the 1/2” Wrench 5/8” Wrench Cylinder Fitting Base with a 1/2” wrench and turning the Hydraulic Hose Fitting Cylinder Fitting counter-clockwise with a 5/8” wrench. -

An Introduction to Topology the Classification Theorem for Surfaces by E
An Introduction to Topology An Introduction to Topology The Classification theorem for Surfaces By E. C. Zeeman Introduction. The classification theorem is a beautiful example of geometric topology. Although it was discovered in the last century*, yet it manages to convey the spirit of present day research. The proof that we give here is elementary, and its is hoped more intuitive than that found in most textbooks, but in none the less rigorous. It is designed for readers who have never done any topology before. It is the sort of mathematics that could be taught in schools both to foster geometric intuition, and to counteract the present day alarming tendency to drop geometry. It is profound, and yet preserves a sense of fun. In Appendix 1 we explain how a deeper result can be proved if one has available the more sophisticated tools of analytic topology and algebraic topology. Examples. Before starting the theorem let us look at a few examples of surfaces. In any branch of mathematics it is always a good thing to start with examples, because they are the source of our intuition. All the following pictures are of surfaces in 3-dimensions. In example 1 by the word “sphere” we mean just the surface of the sphere, and not the inside. In fact in all the examples we mean just the surface and not the solid inside. 1. Sphere. 2. Torus (or inner tube). 3. Knotted torus. 4. Sphere with knotted torus bored through it. * Zeeman wrote this article in the mid-twentieth century. 1 An Introduction to Topology 5. -

Binocular Vision and the Stroop Test
1040-5488/16/9302-0194/0 VOL. 93, NO. 2, PP. 194Y208 OPTOMETRY AND VISION SCIENCE Copyright * 2015 American Academy of Optometry REVIEW Binocular Vision and the Stroop Test Franc¸ois Daniel* and ZoB Kapoula† ABSTRACT Purpose. Recent studies report a link between optometric results, learning disabilities, and problems in reading. This study examines the correlations between optometric tests of binocular vision, namely, of vergence and accommodation, reading speed, and cognitive executive functions as measured by the Stroop test. Methods. Fifty-one students (mean age, 20.43 T 1.25 years) were given a complete eye examination. They then performed the reading test L’Alouette and the Stroop interference test at their usual reading distance. Criteria for selection were the absence of significant refractive uncorrected error, strabismus, amblyopia, color vision defects, and other neurologic findings. Results. The results show a correlation between positive fusional vergences (PFVs) at near distance and the interference effect (IE) in the Stroop test: the higher the PFV value is, the less the IE. Furthermore, the subgroup of 11 students presenting convergence insufficiency, according to Scheiman and Wick criteria (2002), showed a significantly higher IE during the Stroop test than the other students (N = 18) who had normal binocular vision without symptoms at near. Importantly, there is no correlation between reading speed and PFV either for the entire sample or for the subgroups. Conclusions. These results suggest for the first time a link between convergence capacity and the interference score in the Stroop test. Such a link is attributable to the fact that vergence control and cognitive functions mobilize the same cortical areas, for example, parietofrontal areas. -

Ocular Surface Changes Associated with Ophthalmic Surgery
Journal of Clinical Medicine Review Ocular Surface Changes Associated with Ophthalmic Surgery Lina Mikalauskiene 1, Andrzej Grzybowski 2,3 and Reda Zemaitiene 1,* 1 Department of Ophthalmology, Medical Academy, Lithuanian University of Health Sciences, 44037 Kaunas, Lithuania; [email protected] 2 Department of Ophthalmology, University of Warmia and Mazury, 10719 Olsztyn, Poland; [email protected] 3 Institute for Research in Ophthalmology, Foundation for Ophthalmology Development, 61553 Poznan, Poland * Correspondence: [email protected] Abstract: Dry eye disease causes ocular discomfort and visual disturbances. Older adults are at a higher risk of developing dry eye disease as well as needing for ophthalmic surgery. Anterior segment surgery may induce or worsen existing dry eye symptoms usually for a short-term period. Despite good visual outcomes, ocular surface dysfunction can significantly affect quality of life and, therefore, lower a patient’s satisfaction with ophthalmic surgery. Preoperative dry eye disease, factors during surgery and postoperative treatment may all contribute to ocular surface dysfunction and its severity. We reviewed relevant articles from 2010 through to 2021 using keywords “cataract surgery”, ”phacoemulsification”, ”refractive surgery”, ”trabeculectomy”, ”vitrectomy” in combina- tion with ”ocular surface dysfunction”, “dry eye disease”, and analyzed studies on dry eye disease pathophysiology and the impact of anterior segment surgery on the ocular surface. Keywords: dry eye disease; ocular surface dysfunction; cataract surgery; phacoemulsification; refractive surgery; trabeculectomy; vitrectomy Citation: Mikalauskiene, L.; Grzybowski, A.; Zemaitiene, R. Ocular Surface Changes Associated with Ophthalmic Surgery. J. Clin. 1. Introduction Med. 2021, 10, 1642. https://doi.org/ 10.3390/jcm10081642 Dry eye disease (DED) is a common condition, which usually causes discomfort, but it can also be an origin of ocular pain and visual disturbances. -
A Virtual Try-On System for Prescription Eyeglasses
Feature Article A Virtual Try-On System for Prescription Eyeglasses Qian Zhang and Yu Guo ■ Nanyang Technological University Pierre-Yves Laffont, Tobias Martin, and Markus Gross ■ ETH Zurich ision-correcting eyeglasses have improved We present a system for virtually trying on pre- the lives of millions of people. Eyeglasses scription eyeglasses. Our system acts as a virtual significantly affect the wearer’s appear- mirror, allowing users to try on a variety of eye- Vance, and the selection of new pairs of eyeglasses is glasses with corrective lenses based on their pre- largely based on how the glasses look when wearers scription (see Figure 2). We use an image sequence try them on. However, an often overlooked fact is of the user without eyeglasses as input, along with that corrective lenses introduce distortion caused the user’s eyeglasses prescription and a 3D model by the refraction effect. As Figure 1 illustrates, the of the desired eyeglasses frame. Our system gen- eyes of a person wearing correc- erates a 3D representation of the corrective lenses tive lenses for nearsightedness mounted into the eyeglasses frame and modifies the Corrective lenses introduce appear smaller compared with video sequence to virtually insert the eyeglasses us- distortion caused by the wearing nonprescription lenses, ing image-based rendering. This approach simulates refraction effect, which whereas the eyes of a person the distortion introduced by the prescription lenses changes the wearer’s wearing lenses for farsightedness and gives users a better idea of how they would look appearance. To give users a appear larger. when wearing the new pair of eyeglasses. -

Physical Eye Examination
Physical Eye Examination Kaevalin Lekhanont, MD Department of Ophthalmology Ramathibodi Hospp,ital, Mahidol Universit y Outline • Visual acuity (VA) testing – Distant VA test – Pinhole test – Near VA test • Visual field testing • Record and interpretations Outline • Penlight examination •Swingggping penli ght test • Direct ophthalmoscopy – Red reflex examination • Schiotz tonometry • RdditttiRecord and interpretations Conjunctiva, Sclera Retina Cornea Iris Retinal blood vessels Fovea Pupil AtAnteri or c ham ber Vitreous Aqueous humor Lens Optic nerve Trabecular meshwork Ciliary body Choriod and RPE Function evaluation • Visual function – Visual acuity test – Visual field test – Refraction • Motility function Anatomical evaluation Visual acuity test • Distant VA test • Near VA test Distance VA test Snellen’s chart • 20 ฟุตหรือ 6 เมตร • วัดที่ละขาง ตาขวากอนตาซาย • ออานทละตาานทีละตา แถวบนลงลแถวบนลงลางาง • บันทึกแถวลางสุดที่อานได Pinhole test VA with pinhole (PH) Refractive error emmetitropia myypopia hyperopia VA record 20/200 ผูปวยสามารถอานต ัวเลขทมี่ ี ขนาดใหญขนาดใหญพอทคนปกตพอที่คนปกติ สามารถอานไดจากท ี่ระยะ 200 ฟตฟุต แตแตผผปูปวยอานไดจากวยอานไดจาก ที่ระยะ 20 ฟุต 20/20 Distance VA test • ถาอานแถวบนสุดไไไมได ใหเดินเขาใกล chthart ทีละกาวจนอานได (10/200, 5/200) • Counting finger 2ft - 1ft - 1/2ft • Hand motion • Light projection • Light perception • No light perception (NLP) ETDRS Chart Most accurate Illiterate E chart For children age ≥ 3.5 year Near VA test Near chart •14 นวิ้ หรอื 33 เซนตเมตริ • วัดที่ละขาง ตาขวากอนตาซาย • อานทีละตา แถวบนลงลาง -

Accuracy of Noncycloplegic Retinoscopy, Retinomax Autorefractor, and Suresight Vision Screener for Detecting Significant Refractive Errors
Eye Movements, Strabismus, Amblyopia, and Neuro-Ophthalmology Accuracy of Noncycloplegic Retinoscopy, Retinomax Autorefractor, and SureSight Vision Screener for Detecting Significant Refractive Errors Marjean Taylor Kulp,1 Gui-shuang Ying,2 Jiayan Huang,2 Maureen Maguire,2 Graham Quinn,3 Elise B. Ciner,4 Lynn A. Cyert,5 Deborah A. Orel-Bixler,6 and Bruce D. Moore7 1The Ohio State University College of Optometry, Columbus, Ohio 2University of Pennsylvania, Philadelphia, Pennsylvania 3Children’s Hospital of Pennsylvania, Philadelphia, Pennsylvania 4Pennsylvania College of Optometry at Salus University, Elkins Park, Pennsylvania 5Northeastern State University, Oklahoma College of Optometry, Tahlequah, Oklahoma 6University of California Berkeley School of Optometry, Berkeley, California 7New England College of Optometry, Boston, Massachusettes Correspondence: Marjean Taylor PURPOSE. To evaluate, by receiver operating characteristic (ROC) analysis, the ability of Kulp, The OSU College of Optome- noncycloplegic retinoscopy (NCR), Retinomax Autorefractor (Retinomax), and SureSight try, 338 West Tenth Avenue, Colum- Vision Screener (SureSight) to detect significant refractive errors (RE) among preschoolers. bus, OH 43210; [email protected]. METHODS. Refraction results of eye care professionals using NCR, Retinomax, and SureSight (n 2588) and of nurse and lay screeners using Retinomax and SureSight ( 1452) were Submitted: October 13, 2013 ¼ n ¼ Accepted: January 21, 2014 compared with masked cycloplegic retinoscopy results. Significant RE was defined as hyperopia greater than þ3.25 diopters (D), myopia greater than 2.00 D, astigmatism greater Citation: Kulp MT, Ying G-S, Huang J, than 1.50 D, and anisometropia greater than 1.00 D interocular difference in hyperopia, et al. Accuracy of noncycloplegic greater than 3.00 D interocular difference in myopia, or greater than 1.50 D interocular retinoscopy, Retinomax Autorefractor, and SureSight Vision Screener for difference in astigmatism. -

Effects of Nd:YAG Laser Capsulotomy in Posterior Capsular Opacification
Original Research Article Effects of Nd:YAG laser capsulotomy in posterior capsular opacification Praveen Kumar G S1, Lavanya P2*, Raviprakash D3 1Assistant Professor, 2Associate Professor, 3Professor & HOD, Department of Ophthalmology, Shridevi institute of Medical Sciences and Research Hospital, Sira Road, NH-4 Bypass Road, Tumkur- 572106, INDIA. Email: [email protected] Abstract Background: Posterior capsular opacification (PCO) is the most common long-term complication of cataract surgery in both phacoemulsification and extracapsular cataract extraction (ECCE). The overall incidence of PCO and the incidence of neodymium-doped yttrium–aluminum–garnet (Nd:YAG) laser posterior capsulotomy has decreased from 50% in the 1980s and early 1990s to less than 10% today. Reported complications of Nd:YAG laser posterior capsulotomy include elevated intraocular pressure, iritis, corneal damage, intraocular lens (IOL) damage, cystoids macular edema, disruption of the anterior hyaloid surface, increased risk of retinal detachment, and IOL movement or dislocation. In some patients, a refraction change is noticed after Nd:YAG laser posterior capsulotomy, but proving this remains difficult. Materials and Methods: Nd; YAG LASER capsulotomy was performed in 200 eyes of 200 patients, some with pseudophakia and some with aphakia at Kurnool medical college, Kurnool. They were followed up between October 2008 and September 2010. Results: Elevation of IOP has been well documented after anterior segment laser procedures. The IOP rise after YAG laser posterior capsulotomy is of short duration starting about 1 hr after laser procedure and lasting for 24 hrs. In this study, in 1case IOP came down to normal level after 3 days and in another case after 7 days. -
Intraocular Lenses and Spectacle Correction
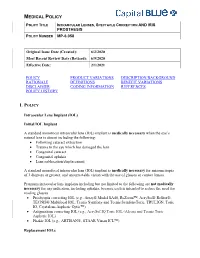
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -

And Minus Cylinder Subjective Refraction Techniques for Clinicians January 2016
Mark E Wilkinson, OD Plus and Minus Cylinder Subjective Refraction Techniques for Clinicians January 2016 General Refraction Techniques Prior to starting your refraction, baseline visual acuities (OD, OS and OU) must be determined. For individuals with near vision complaints, and all presbyopes, near acuity should also be documented using M notation, with the testing distance documented if different than 16 inches (40 centimeters). Accurately assessing visual acuity is important for many reasons. It allows the clinician to: § Determine best corrected acuity with refraction § Monitor the effect of treatment and/or progression of disease § Estimate the dioptric power of optical devices necessary for reading regular size print § Verify eligibility for tasks such as driving § Verify eligibility as “legally blind” When measuring distance acuity, there is no longer a need to measure visual acuity in a darkened room. In the past, when projected charts were used, the room lights had to be lowered for better contrast on the chart. Now, with high definition LCD monitor acuity charts and ETDRS charts, contrast is no longer an issue. Additionally, for some patients, particularly those with difficulties adjusting to lower lighting conditions, taking them from a normally lit waiting room into a darkened clinic or work up room will artificially lower their acuity, because they do not have enough time for their eyes to adjust to the lower light conditions. Because clinical decisions are based on these acuity measurements, accurate assessment of each person’s acuity is critically important. With this in mind, all acuity testing should be done with the overhead lights on in the exam or work up room.