Indep Link Beg 2.21.18.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Lee, Blackburn Claim TN Victory
6,250 subscribers www.TML1.org Volume 69, Number 19 Nov. 12, 2018 Lee, Blackburn claim TN victory TML District Meetings Thursday, Nov. 29 District 4 Crossville Friday, Nov. 30 District 3 Collegedale Tuesday, Dec. 4 District 5 Gallatin Wednesday, Dec. 5 District 2 Morristown Thursday, Dec. 6 District 1 Greeneville Monday, Dec. 10 District 7 Henderson Tuesday, Dec. 11 District 8 Millington Friday, Dec 14 District 6 Columbia Mark your calendars and plan to attend! Photos by The Tennessean Tennesseans elected Repub- And I couldn’t be more grateful,” Corker, who after serving two lican Bill Lee as the state’s 50th Lee said during his acceptance terms opted not to run again. governor on Nov. 6, voting into speech. “I’m grateful you placed Blackburn won the seat with office a political newcomer. Lee your trust in us to lead this great 55 percent of the votes to Bre- easily defeated former Nashville state of Tennessee.” desen’s 44 percent. Mayor Karl Dean with 60 percent Lee will be sworn into office Blackburn has served the of the votes to Dean’s 39 percent. on Saturday, Jan. 19, 2019, in 7th Congressional District in the Lee, 59, is a Tennessean busi- Nashville. House of Representatives since nessman and CEO of his family’s Republican Marsha Blackburn 2003. She previously served in the HVAC, plumbing, and electrical defeated former Tennessee Gov- Tennessee Senate from 1999 to business, Lee Company. He cam- ernor Phil Bredesen to become 2003. paigned on a socially and fiscally Tennessee’s first female elected to For a complete results of conservative platform. -

General Election State of Tennessee Tennessee House of Representatives District 1
State of Tennessee November 6, 2012 General Election Tennessee House of Representatives District 1 1 . Jon C. Lundberg - (R) 1 SULLIVAN 17,503 DISTRICT TOTALS 17,503 05-Dec-12 State of Tennessee November 6, 2012 General Election Tennessee House of Representatives District 2 1 . Tony Shipley - (R) 2 . Bruce Dotson - (D) 1 2 SULLIVAN 16,764 7,794 DISTRICT TOTALS 16,764 7,794 05-Dec-12 State of Tennessee November 6, 2012 General Election Tennessee House of Representatives District 3 1 . Timothy Hill - (R) 2 . Leah R. Kirk - (D) 3 . Suzanne Parker - (G) 1 2 3 CARTER 2,747 521 148 JOHNSON 4,300 1,018 238 SULLIVAN 8,963 2,880 449 DISTRICT TOTALS 16,010 4,419 835 05-Dec-12 State of Tennessee November 6, 2012 General Election Tennessee House of Representatives District 4 1 . Thomas Gray - (R) 2 . Kent Williams - (I) 1 2 CARTER 6,334 9,112 UNICOI 3,553 2,361 DISTRICT TOTALS 9,887 11,473 05-Dec-12 State of Tennessee November 6, 2012 General Election Tennessee House of Representatives District 5 1 . David B. Hawk - (R) 2 . Eddie Yokley - (D) 3 . Write-In - Jason Scott Moore 1 2 3 GREENE 11,566 8,292 1 DISTRICT TOTALS 11,566 8,292 1 05-Dec-12 State of Tennessee November 6, 2012 General Election Tennessee House of Representatives District 6 1 . James (Micah) Van Huss - (R) 2 . Michael Clark - (D) 1 2 WASHINGTON 16,391 6,271 DISTRICT TOTALS 16,391 6,271 05-Dec-12 State of Tennessee November 6, 2012 General Election Tennessee House of Representatives District 7 1 . -
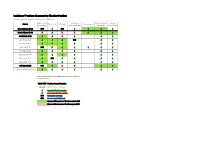
Legislators' Positions Compared to Chamber Positions
Legislators' Positions Compared to Chamber Positions Positions of legislators based on voting record and bill sponsors. Right-to-Work Safe Harbor Pregnant Workers Criminal Senator Tobacco Sales Safe Harbor Transpotainment Amendment Conference Report Fairness Act Justice Reform Steve Dickerson (R-20) NVR √ NVR √ √ √ √ Brenda Gilmore (D-19) X √ X X √ √ √ Ferrell Haile (R-18) √ √ √ √ √ √ Joey Hensley (R-28) √ √ √ NVR √ √ Jack Johnson (R-23) √ √ √ √ √ √ Mark Pody (R-17) NVR X √ √ √ √ √ Bill Powers (R-22) √ √ √ √ √ √ Shane Reeves (R-14) √ √ √ √ √ √ Kerry Roberts (R-25) √ PNV √ √ √ √ Dawn White (R-13) √ √ √ √ √ √ Jeff Yarbro (D-21) NVR √ X X √ √ Lt. Governor Randy McNally (R-5) √ √ √ √ √ √ Blank spaces indicate that the legislator did not have an opportunity to vote on the bill. BOLD TEXT Davidson County Delegation UN-BOLD Middle Tennessee delegation √ Supported Chamber position X Opposed to Chamber position PNV Present but not voting NVR No vote recorded (absent) Sponsored/Co-sponsored Chamber-endorsed bill Sponsored/Co-sponsored Chamber-opposed bill ` Legislators' Positions Compared to Chamber Positions Positions of legislators based on voting record and bill sponsors. Right-to-Work Safe Harbor Pregnant Workers Criminal Justice Representative Tobacco Sales Safe Harbor Amendment Conference Report Fairness Act Reform Charie Baum (R-37) √ √ √ √ √ √ Bill Beck (D-51) X √ X X √ √ Clark Boyd (R-46) √ X √ √ √ √ Glen Casada (R-62) √ √ √ √ NVR √ Scott Cepicky (R-64) √ √ √ √ √ √ John Ray Clemmons (D-55) X √ X X √ √ Michael Curcio (R-69) √ X √ X √ √ Vincent Dixie (D-54) X √ PNV X √ √ Bob Freeman (D-56) X √ √ PNV √ √ Johnny Garrett (R-45) √ PNV √ X √ √ Jason Hodges (D-67) X PNV X X √ √ Darren Jernigan (D-60) X √ √ NVR √ √ Curtis Johnson (R-68) √ √ √ X √ √ Sabi Kumar (R-66) √ √ √ NVR √ √ William Lamberth (R-44) √ √ √ X √ X Mary Littleton (R-78) √ √ √ PNV √ √ Harold Love, Jr. -

Tennessee Right to Life Scorecard – Pro-Life Legislation Votes, 2015 Tennessee House of Representatives 109Th General Assembly
PO Box 110765 Nashville, TN 37222-0765 Ph 615.298.5433 [email protected] Facebook.com/groups/tnrtl/ www.tnrtl.org Twitter.com/tnrighttolife Tennessee Right to Life Scorecard – Pro-Life Legislation Votes, 2015 Tennessee House of Representatives 109th General Assembly 1. House Floor Vote on SB1222/HB0977 (Informed Consent for Women and Girls Considering Abortion and a 48-hour Waiting Period), April 21, 2015. (Passed 79-18) 2. House Floor Vote on SB1280/HB1368 (Regulation of Abortion Facilities, requiring inspection and licensure), April 21, 2015 (Passed 80-17) Representative 1 2 X O Score Speaker Beth Harwell (R-Nashville) X X 2 0 100% Raumesh Akbari (R-Winchester) O O 0 2 0% David Alexander (R-Winchester) X X 2 0 100% Joe Armstrong (D-Knoxville) O O 0 2 0% Bill Beck (D-Nashville) A A 0 0 N/A Harry Brooks (R-Knoxville) X X 2 0 100% Kevin Brooks (R-Cleveland) X X 2 0 100% Sheila Butt (R-Columbia) X X 2 0 100% David Byrd (R – Waynesboro) X X 2 0 100% Kent Calfee (R-Kingston) X X 2 0 100% Karen Camper (D-Memphis) O O 0 2 0% Dale Carr (R-Sevierville) X X 2 0 100% Mike Carter (R-Ooltewah) X X 2 0 100% Glen Casada (R-Thompsons Station) X X 2 0 100% John Ray Clemmons (D-Nashville) O O 0 2 0% Jim Coley (R-Bartlett) X X 2 0 100% Barbara Cooper (D-Memphis) O O 0 2 0% Martin Daniel (R-Knoxville) X X 2 0 100% John DeBerry (D-Memphis) X X 2 0 100% Barry Doss (R-Leoma) X X 2 0 100% Kevin Dunlap (D-Rock Island) X X 2 0 100% Bill Dunn (R-Knoxville) X X 2 0 100% Jeremy Durham (R-Franklin) X X 2 0 100% Jimmy Eldridge (R-Jackson) X X 2 0 100% Jeremy Faison (R-Cosby) X X 2 0 100% Andrew Farmer (R-Sevierville) X X 2 0 100% Joanne Favors (D-Chattanooga) O O 0 2 0% Craig Fitzhugh (D-Ripley) O X 1 1 50% John Forgety (R-Athens) X X 2 0 100% Brenda Gilmore (D-Nashville) O O 0 2 0% Tilman Goins (R-Morristown) X X 2 0 100% Marc Gravitt (R-East Ridge) X X 2 0 100% Curtis Halford (R-Dyer) X X 2 0 100% G.A. -

Wedded to Wasting Time
VIEW FROM THE HILL Wedded to wasting time Is legislative action needed to protect clergy from same- sex nuptials? Experts say no. REALTY CHECK Sliding into P3 a new home If real estate deals had DAVIDSONLedger • WILLIAMSON • SUMNER • CHEATHAM • RUTHERFORD WILSON ROBERTSON • MAURY • DICKSON • MONTGOMERYumpires, • KNOX • ANDERSONthere might •BLOUNT be fewer•SEVIER brushbacks and balks. P3 25 years after hitting rock bottom, July 10 – 16, 2015 The power of information.NASHVILLE Vol. 41 EDITION | a new Nashville has emerged Issue 28 www.TNLedger.com Stories by | FORMERLY WESTVIEW SINCE 1978 Tim Ghianni begin on page 2 Page 13 Dec.: Nashville Public Library, Dec.: Keith Turner, Ratliff, Jeanan Mills Stuart, Resp.: Kimberly Dawn Wallace, Atty: Sheriff FateSpecial Thomas Collections Mary C Lagrone, 08/24/2010, 10P1318 In re: Jeanan Mills Stuart, Princess Angela Gates, Jeanan Mills Stuart, Princess Angela Gates,Dec.: Resp.: Kim Prince Patrick, Angelo Terry Patrick, pleaded guilty to mail Gates, Atty: Monica D Edwards, 08/25/2010, 10P1326 fraud, theft of In re: Keith Turner, TN Dept Of Correction, www.westviewonline.com TN Dept Of Correction, Resp.: Johnny Moore,Dec.: Melinda Atty: Bryce L Tomlinson, Coatney, Resp.: government property Pltf(s): Rodney A Hall, Pltf Atty(s): n/a, 08/27/2010, 10P1336 In re: Kim Patrick, Terry Patrick, Pltf(s): Sandra Heavilon, Resp.: Jewell Tinnon, Atty: Ronald Andre Stewart, 08/24/2010,Dec.: Seton Corp and tax conspiracy on 10P1322 Insurance Company, Dec.: Regions Bank, Resp.: Leigh A Collins, In re: Melinda L Tomlinson, -

TN State Senators and Representatives Contact List 2021
Senators District Name Phone Email Twi4er Facebook 29 Sen. Raumesh Akbari 615.741.1767 [email protected] @SenAkbari h4ps://www.facebook.com/SenAkbari 15 Sen. Paul Bailey 615.741.3978 [email protected] @PaulBaileyforTN h4ps://www.facebook.com/paulbaileyforsenate 9 Sen. Mike Bell 615.741.1946 [email protected] @SenMikeBell h4ps://www.facebook.com/SenMikeBell 16 Sen. Janice Bowling 615.741.6694 [email protected] @Janicebowlingtn h4ps://www.facebook.com/Senator-Janice-Bowling-202797446470765 7 Sen. Richard Briggs 615.741.1766 [email protected] @SenatorBriggs h4ps://www.facebook.com/RichardBriggsTN 20 Sen. Heidi Campbell 615.741.6679 [email protected] @campbellyn20 h4ps://www.facebook.com/campbelltn20 3 Sen. Rusty Crowe 615.741.2468 [email protected] 10 Sen. Todd Gardenhire 615.741.6682 [email protected] @SenGardenhire h4ps://www.facebook.com/VoteGardenhire 19 Sen. Brenda Gilmore 615.741.2453 [email protected] @SenatorGilmore h4ps://www.facebook.com/SenatorGilmore 18 Sen. Ferrell Haile 615.741.1999 [email protected] @HaileforSenate h4ps://www.facebook.com/FerrellHaileTN 28 Sen. Joey Hensley 615.741.3100 [email protected] @joey_senator h4ps://www.facebook.com/SenatorJoeyHensley 27 Sen. Ed Jackson 615.741.1810 [email protected] @SenEdJackson h4ps://www.facebook.com/SenEdJackson 23 Sen. Jack Johnson 615.741.2495 [email protected] @SenJohnson h4ps://www.facebook.com/SenatorJackJohnson 31 Sen. Brian Kelsey 615.741.3036 [email protected] @BrianKelsey h4ps://www.facebook.com/briankelsey 30 Sen. -

Indep Link Beg 2.21.18.Indd
,QGHSHQGHQW Tennessee Pharmacists Association ZZZWQSKDUPRUJWSD#WQSKDUPRUJ /LQN March 25, 2019 CALL TO ACTION: PBM Reform Hearings TOMORROW, March 26 There are critically important times in a profession when and bring increased transparency within the prescription a massive response from the pharmacy community is drug delivery system. On Tuesday, March 26, the House needed in order to e ect change. TODAY is one of those Insurance Committee is scheduled to hear House Bill times! 786, and the Senate Commerce and Labor Commit- tee is scheduled to hear Senate Bill 650. This legislative Over the past few years, the noise has increasingly grown initiative is critically important to increase prescription louder for prescription drug pricing reform in order to drug pricing transparency to the state and our patients bring down costs for patients. State and federal legisla- in order to drive down prescription drug costs, as well tors and regulators are seeking strategies to bring down as to level the playing ȴ eld between PBMs and pharma- costs for patients in meaningful ways. The rebate system cies. As introduced, this legislation establishes fair con- that has been allowed under our current health care sys- tracting and audit protections for pharmacies, prohibits tem has created opportunities for middlemen like phar- PBMs from utilizing retroactive, non-transparent fees at macy beneȴ ts managers (PBMs) to exert their massive the state level, and requires an audit of all state-funded inȵ uence and gain an incredibly large share of the proȴ t PBMs. This legislation is common-sense reform aimed on prescription drugs, regardless of the overall e ect on at increasing prescription drug pricing transparency and patients and their drug costs. -

Candidates TMA Supported As of June 30, 2016
Candidates TMA Supported as of June 30, 2016: Representative Raumesh Akbari (D-Memphis) Representative David Alexander (R-Winchester) Representative Kevin Brooks (R-Cleveland) Representative Barbara Ward Cooper (D-Memphis) Representative Martin Daniel (R-Knoxville) Representative John DeBerry (D-Memphis) Representative Jimmy Eldridge (R-Jackson) Representative Jeremy Faison (R-Cosby) Representative John Forgety (R-Athens) Senator Delores Gresham (R-Somerville) Representative G.A. Hardaway (D-Memphis) Senator Lee Harris (D-Memphis) Representative David Hawk R-Greeneville) Representative Patsy Hazlewood (R-Signal Mountain) Representative Gary Hicks (R-Rogersville) Representative Dan Howell (R-Georgetown) Representative Bud Hulsey (R-Kingsport) Senator Ed Jackson (R-Jackson) Representative Darren Jernigan (D-Old Hickory) Representative Sherry Jones (D-Nashville) Representative Sabi ''Doc'' Kumar (R-Springfield) Representative William Lamberth (R-Cottontown) Representative Harold M. Love Jr. (D-Nashville) Representative Gerald McCormick (R-Chattanooga) Representative Stephen McManus (R-Cordova) Representative Larry Miller (D-Memphis) Representative Bo Mitchell (D-Nashville) Senator Mark Norris (R-Collierville) Senator Doug Overbey (R-Maryville) Representative Mark Pody (R-Lebanon) Representative Dennis Powers (R-Jacksboro) Representative John Ragan (R-Oak Ridge) Senator Randy McNally (R-Oak Ridge) Representative John Ray Clemmons (D-Nashville) Representative Jay Reedy (R-Erin) Representative Courtney Rogers (R-Goodlettsville) Representative Cameron Sexton (R-Crossville) Representative Johnny Shaw (D-Bolivar) Representative Mike Sparks (R-Smyrna) Representative Curry Todd (R-Collierville) Representative Joe Towns Jr. (D-Memphis) Senator Jim Tracy (R-Shelbyville) Representative Johnnie Turner (D-Memphis) The Committee to Elect Mike Waggoner (R-Chapel Hill) Representative Terry Lynn Weaver (R-Mount Juliet) Representative Ryan William (R-Cookeville) Representative Tim Wirgau (R-Buchanan) . -

Tenncare and Tennessee Real Estate: What Real Estate Professionals Need to Know FIDELITY NATIONAL TITLE GROUP JESSICA WEBB-AYER Introduction to Tenncare
TennCare and Tennessee Real Estate: What Real Estate Professionals Need to Know FIDELITY NATIONAL TITLE GROUP JESSICA WEBB-AYER Introduction to TennCare TennCare is a program that provides health insurance to people who are eligible for Medicaid and to certain other people who lack access to insurance. A managed care model is used for delivering program benefits. In order to qualify for this benefit program, you must be: ◦ A resident of the state of Tennessee; and ◦ A U.S. citizen or qualified alien. TennCare Qualifications To qualify for TennCare, you must also be: ◦ Pregnant; ◦ A child under age 19; ◦ A parent or relative caretaker of a dependent child or children under age 21; ◦ Disabled; ◦ Elderly; or ◦ Uninsurable. Financial Eligibility ◦ Individuals must also meet the financial eligibility criteria that go with each category. ◦ Generally, an individual’s financial situation would be characterized as either low income or very low income. ◦ In order to qualify, the individual must have an annual household income (before taxes) that is below a certain amount. History of Medicaid ◦ To understand TennCare completely, we need to have a history lesson and take a look at Medicaid. ◦ In 1965, President Lyndon B. Johnson signed Medicare and Medicaid into law. ◦ Medicare v. Medicaid ◦ Medicare is supposed to help with short-term needs rather than long-term care. It provides health insurance and other medical needs to elderly and disabled U.S. citizens. ◦ Medicaid is supposed to help low-income earners with long-term health services and support costs they could not afford by themselves. Medicaid: A Federal and State PrograM Because Medicaid is such an expensive and comprehensive program: ◦ Under the Social Security Act, it was designed as a joint federal and state insurance program. -

Knoxville One of 20 Finalists in $9 Million Bloomberg Challenge
1-TENNESSEE TOWN & CITY/NOV. 12, 2012 www.TML1.org 6,250 subscribers www.TML1.org Volume 63, Number 17 November 12, 2012 Obama re-elected; TN incumbents return to U.S. Congress; GOP wins supermajority in Legislature BY CAROLE GRAVES TML Communications Director In a hard-fought battle, Presi- dent Barack Obama earned his sec- ond term in the White House, win- ning 303 electoral votes and 50 per- cent of the popular vote in one of the most expensive presidential cam- paigns in history. In defeating former Massachu- setts Gov. Mitt Romney, the presi- dent carried the battleground states of Ohio, Wisconsin, Iowa, New Hampshire, Colorado, and Virginia. Overall, Obama won 25 states and the District of Columbia. Rom- Photo: Chris Carlson/AP ney won 24 states. The outcome in President Barack Obama and first lady Michelle Obama wave at his Florida is still pending. election night party in Chicago. President Obama defeated Republican Photo: Larry McCormack/Tennessean Tennessee overwhelmingly challenger former Massachusetts Gov. Mitt Romney. U.S. Sen. Bob Corker, flanked by his wife Elizabeth, is congratulated went to Romney with 59.5 percent of by Gov. Bill Haslam on his reelection to a second term. the vote. And despite what happened Hawk, who beat former Democratic Corker easily cruised to a second on the national scene, it was a big Rep. Eddie Yokley in District 5. In six-year term with 65 percent of the night for Republicans in Tennessee, House District 33, Republican John vote. winning their first supermajority in Ragan beat back a challenge former The state's eight congressional both chambers of the Tennessee Rep. -
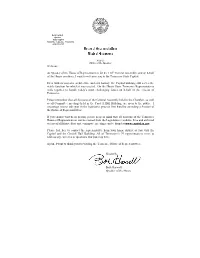
Welcome: As Speaker of the House of Representatives for the 110Th
Beth Harwell Speaker State Capitol Nashville, Tennessee 37243-0104 (615)741-0709 Nashville Office of the Speaker Welcome: As Speaker of the House of Representatives for the 110 th General Assembly, and on behalf of the House members, I want to welcome you to the Tennessee State Capitol. Even with its majestic architecture and rich history, the Capitol building still serves the viable function for which it was erected. On the House floor, Tennessee Representatives work together to handle today’s most challenging issues on behalf of the citizens of Tennessee. Please remember that all Sessions of the General Assembly held in the Chamber, as well as all Committee meetings held in the Cordell Hull Building, are open to the public. I encourage you to take part in the legislative process first hand by attending a Session of the House of Representatives. If you cannot visit us in person, please keep in mind that all sessions of the Tennessee House of Representatives can be viewed from the Legislature’s website. Live and archived videos of all House floor and committee meetings can be found at www.capitol.tn.gov . Please feel free to contact the representative from your home district as you visit the Capitol and the Cordell Hull Building. All of Tennessee’s 99 representatives serve to address any concerns or questions that you may have. Again, I want to thank you for visiting the Tennessee House of Representatives. Sincerely, Beth Harwell Speaker of the House TENNESSEE House of Representatives 110 th General Assembly Beth Harwell , Speaker of the House Curtis Johnson , Speaker Pro Tempore Steve K. -

1 2016 U.S. Political Contribution and Expenditure Policy and Statement
2016 U.S. Political Contribution and Expenditure Policy and Statement The Company’s policy is to participate in public policymaking by informing government officials about our positions on issues significant to the Company and our customers. These issues are discussed in the context of existing and proposed laws, legislation, regulations, and policy initiatives, and include, for example, Internet commerce, sales tax, intellectual property rights, trade, data privacy, and web services. Relatedly, the Company constructively and responsibly participates in the U.S. political process. The goal of the Company’s political contributions and expenditures is to promote the interests of the Company and our customers, and the Company makes such decisions in accordance with the processes described in this political contribution and expenditure policy and statement, without regard to the personal political preferences of the Company’s directors, officers, or employees. Approval Process The Company’s Vice President of Public Policy reviews and approves each political contribution and expenditure made with Company funds or resources to, or in support of, any political candidate, political campaign, political party, political committee, or public official in any country, or to any other organization for use in making political expenditures, to ensure that it is lawful and consistent with the Company’s business objectives and public policy priorities. The Company’s Senior Vice President for Corporate Affairs and the Senior Vice President and General Counsel review all political expenditures. In addition, the Audit Committee of the Board of Directors annually reviews this political contribution and expenditure policy and statement and a report on all of the Company’s political contributions and expenditures, including any contributions made to trade associations or 501(c)(4) social welfare organizations.