Obesity Hypoventilation Syndrome: Understanding, Diagnosing, and Treating
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Approach to Cyanosis in a Neonate.Pdf
PedsCases Podcast Scripts This podcast can be accessed at www.pedscases.com, Apple Podcasting, Spotify, or your favourite podcasting app. Approach to Cyanosis in a Neonate Developed by Michelle Fric and Dr. Georgeta Apostol for PedsCases.com. June 29, 2020 Introduction Hello, and welcome to this pedscases podcast on an approach to cyanosis in a neonate. My name is Michelle Fric and I am a fourth-year medical student at the University of Alberta. This podcast was made in collaboration with Dr. Georgeta Apostol, a general pediatrician at the Royal Alexandra Hospital Pediatrics Clinic in Edmonton, Alberta. Cyanosis refers to a bluish discoloration of the skin or mucous membranes and is a common finding in newborns. It is a clinical manifestation of the desaturation of arterial or capillary blood and may indicate serious hemodynamic instability. It is important to have an approach to cyanosis, as it can be your only sign of a life-threatening illness. The goal of this podcast is to develop this approach to a cyanotic newborn with a focus on these can’t miss diagnoses. After listening to this podcast, the learner should be able to: 1. Define cyanosis 2. Assess and recognize a cyanotic infant 3. Develop a differential diagnosis 4. Identify immediate investigations and management for a cyanotic infant Background Cyanosis can be further broken down into peripheral and central cyanosis. It is important to distinguish these as it can help you to formulate a differential diagnosis and identify cases that are life-threatening. Peripheral cyanosis affects the distal extremities resulting in blue color of the hands and feet, while the rest of the body remains pinkish and well perfused. -

Chest Pain and the Hyperventilation Syndrome - Some Aetiological Considerations
Postgrad Med J: first published as 10.1136/pgmj.61.721.957 on 1 November 1985. Downloaded from Postgraduate Medical Journal (1985) 61, 957-961 Mechanism of disease: Update Chest pain and the hyperventilation syndrome - some aetiological considerations Leisa J. Freeman and P.G.F. Nixon Cardiac Department, Charing Cross Hospital (Fulham), Fulham Palace Road, Hammersmith, London W6 8RF, UK. Chest pain is reported in 50-100% ofpatients with the coronary arteriograms. Hyperventilation and hyperventilation syndrome (Lewis, 1953; Yu et al., ischaemic heart disease clearly were not mutually 1959). The association was first recognized by Da exclusive. This is a vital point. It is time for clinicians to Costa (1871) '. .. the affected soldier, got out of accept that dynamic factors associated with hyperven- breath, could not keep up with his comrades, was tilation are commonplace in the clinical syndromes of annoyed by dizzyness and palpitation and with pain in angina pectoris and coronary insufficiency. The his chest ... chest pain was an almost constant production of chest pain in these cases may be better symptom . .. and often it was the first sign of the understood if the direct consequences ofhyperventila- disorder noticed by the patient'. The association of tion on circulatory and myocardial dynamics are hyperventilation and chest pain with extreme effort considered. and disorders of the heart and circulation was ackn- The mechanical work of hyperventilation increases owledged in the names subsequently ascribed to it, the cardiac output by a small amount (up to 1.3 1/min) such as vasomotor ataxia (Colbeck, 1903); soldier's irrespective of the effect of the blood carbon dioxide heart (Mackenzie, 1916 and effort syndrome (Lewis, level and can be accounted for by the increased oxygen copyright. -

What Every Clinician Should Know About Polysomnography
What Every Clinician Should Know About Polysomnography Susheel P Patil MD PhD Introduction Electrical Concepts Current, Voltage, Resistance Capacitance, Inductance, and Impedance Differential Amplifiers Polarity Common Mode Rejection Amplifier Gain, Sensitivity, and Type Patient Ground, Electrical Ground, and Electrical Safety Filters and Filtering Low-Frequency Filters High-Frequency Filters Notch Filters Aspects Unique to Digital Polysomnography Sampling Rate and Aliasing Bit Resolution and Input Voltage Monitor Aliasing Artifacts Updates in Polysomnography Scoring Visual Rules for Sleep Changes in the Scoring of Sleep Under the AASM Manual Comparison of the AASM Manual and R&K Sleep Staging Rules Scoring Reliability of Sleep Staging Under the AASM Manual Scoring of Arousals Movement Rules Scoring of Respiratory Events Summary Polysomnography studies are an essential tool for the sleep physician and aid in the diagnosis and treatment of sleep disorders. Polysomnography refers to the recording, analysis, and interpretation of multiple physiologic signals collected simultaneously. Rapid advancements in technology have transformed the field from a time when analog studies were collected on paper to computer-assisted collection of digitally transformed studies. Sleep clinicians, whether physicians, respiratory thera- pists, or sleep technologists, must therefore have an understanding of a broad array of principles underlying the collection of the various signals. In addition, an understanding of basic technical rules in the evaluation of polysomnography studies is necessary for both the scoring and interpre- tation of such studies. The American Academy of Sleep Medicine published a new manual for the scoring of sleep and associated events in 2007. These changes included modifications to the visual scoring of sleep, the scoring of sleep-disordered breathing events, and movement disorders during sleep. -
Diagnostic Testing for Sleep Disorders
Diagnostic Testing for Sleep Disorders LISA CUTCHEN MD ASSISTANT PROFESSOR UNIVERSITY OF NEW MEXICO HOSPITALS SLEEP DISORDERS CENTER NOVEMBER 11, 2016 Objectives of Talk • Describe the most common types of sleep tests • Explain how and why we test for sleep disorders • Briefly review the most common sleep disorders that require testing Diagnostic Tests for Sleep Disorders • Polysomnography (PSG, Sleep Study) • Overnight Oximetry • Actigraphy • Multiple Sleep Latency Test (MSLT) • Maintenance of Wakefulness Test (MWT)f Diagnostic Tests for Sleep Disorders Sleep Test Quality Measured Polysomnography Simultaneous recording of multiple biophysiological signals to study and characterize sleep and sleep disorders. Overnight oximetry Monitor oxygen saturation and heart rate in bed overnight. Actigraphy Measure sleep/wake patterns over long periods of time by monitoring body movements. Multiple Sleep Latency Test Test ability to fall asleep during the day when permitted and whether REM sleep appears earlier than usual. Maintenance of Wakefulness Test Test ability to stay awake with low levels of stimulation without resorting to extraordinary measures. Polysomnography • 4 Levels of Polysomnograms • Conducted during the patient’s Level I Full PSG, in-lab, attended typical sleep time Level II Full PSG, unattended • Varying levels of complexity Partial PSG, ≥4 • # of signals recorded cardiorespiratory Level III simultaneously parameters, unattended, • Whether attended by a sleep typically done at home technologist Partial PSG, 1-2 cardiorespiratory -

Polysomnography
Sleep Medicine Department 888 S. King St. Honolulu, HI 96813 Ph: (808) 522-4448 Fax: (808) 522-3048 POLYSOMNOGRAPHY What is it? Polysomnography is a sleep study that involves monitoring various bodily functions during sleep, usually during regular nighttime sleeping hours. It allows detection of changes that only occur or are altered during sleep. When the sleep study is evaluated, appropriate diagnoses can be made, allowing treatment to be tailored to the specific problems identified. Some of the problems that can be evaluated by a polysomnography are excessive daytime sleepiness, breathing difficulties during sleep, and periodic leg movements. You will be asked to arrive before your regular bedtime to allow for preparation time. Expect to remain until a full night's sleep activity has been recorded. Sensors are placed on the scalp and other areas to monitor brain waves, eye movements, muscle tension, respiration, heart rate and oxygen levels in the blood using a photo-light sensor. Once all the sensors are in place, you go to bed and are allowed to sleep until morning. You may be offered a treatment trial of nasal CPAP if your recording indicates that you have many obstructive sleep apneas. A specially trained technician will explain all the procedures and answer questions. The technician will be present throughout the night to monitor the recording and to assist you with any questions. If you have questions about the polysomnogram, please call the Sleep Medicine Department at 522-4448. Our office hours are Monday to Friday from 8am-4pm and closed from 12:30pm-1:30pm for lunch. -
Somnology-Jr-Book.Pdf
1 To Grace Zamudio and Zoe Lee-Chiong. 2 Preface Carpe noctem. Teofilo Lee-Chiong MD Professor of Medicine Division of Sleep Medicine National Jewish Health Denver, Colorado University of Colorado Denver School of Medicine Denver, Colorado Chief Medical Liaison Philips Respironics Murrysville, Pennsylvania 3 Abbreviations AHI Apnea-hypopnea index BPAP Bi-level positive airway pressure CPAP Continuous positive airway pressure CSA Central sleep apnea ECG Electrocardiography EEG Electroencephalography EMG Electromyography EOG Electro-oculography FEV1 Forced expiratory volume in 1 second GABA Gamma-aminobutyric acid N1 NREM stage 1 sleep N2 NREM stage 2 sleep N3 NREM stages 3 (and 4) sleep NREM Non-rapid eye movement O2 Oxygen OSA Obstructive sleep apnea PaCO2 Partial pressure of arterial carbon dioxide PaO2 Partial pressure of arterial oxygen REM Rapid eye movement sleep SaO2 Oxygen saturation SOREMP Sleep onset REM period 4 Table of contents Introduction 15 Neurobiology of sleep 16 Neural systems generating wakefulness 16 Neural systems generating NREM sleep 16 Neural systems generating REM sleep 16 Main neurotransmitters 17 Acetylcholine 17 Adenosine 17 Dopamine 17 Gamma-aminobutyric acid 17 Glutamate 17 Glycine 17 Histamine 18 Hypocretin 18 Melatonin 18 Norepinephrine 18 Serotonin 18 Physiology during sleep 19 Autonomic nervous system 19 Respiratory system 19 Respiratory patterns 19 Cardiovascular system 19 Gastrointestinal system 20 Renal and genito-urinary systems 20 Endocrine system 20 Growth hormone 20 Thyroid stimulating hormone -

Insomnia in Adults
New Guideline February 2017 The AASM has published a new clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults. These new recommendations are based on a systematic review of the literature on individual drugs commonly used to treat insomnia, and were developed using the GRADE methodology. The recommendations in this guideline define principles of practice that should meet the needs of most adult patients, when pharmacologic treatment of chronic insomnia is indicated. The clinical practice guideline is an essential update to the clinical guideline document: Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(2):307–349. SPECIAL ARTICLE Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults Sharon Schutte-Rodin, M.D.1; Lauren Broch, Ph.D.2; Daniel Buysse, M.D.3; Cynthia Dorsey, Ph.D.4; Michael Sateia, M.D.5 1Penn Sleep Centers, Philadelphia, PA; 2Good Samaritan Hospital, Suffern, NY; 3UPMC Sleep Medicine Center, Pittsburgh, PA; 4SleepHealth Centers, Bedford, MA; 5Dartmouth-Hitchcock Medical Center, Lebanon, NH Insomnia is the most prevalent sleep disorder in the general popula- and disease management of chronic adult insomnia, using existing tion, and is commonly encountered in medical practices. Insomnia is evidence-based insomnia practice parameters where available, and defined as the subjective perception of difficulty with sleep initiation, consensus-based recommendations to bridge areas where such pa- duration, consolidation, or quality that occurs despite adequate oppor- rameters do not exist. -

Validation of Oximetry for Diagnosing Obstructive Sleep Apnea in a Clinical Setting
Article Validation of Oximetry for Diagnosing Obstructive Sleep Apnea in a Clinical Setting Kazuki Ito 1,2, Masahiro Uetsu 3 and Hiroshi Kadotani 1,3,* 1 Department of Sleep and Behavioral Sciences, Shiga University of Medical Science, Seta Tsukinowa-cho, Otsu, Shiga 520-2192, Japan; [email protected] 2 Department of Anesthesiology, Shiga University of Medical Science, Seta Tsukinowa-cho, Otsu, Shiga 520-2192, Japan 3 Sleep Outpatient Unit for Sleep Apnea Syndrome, Nagahama City Hospital, 313 Ohinui-cho, Nagahama, Shiga 526-0043, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-775483632 Received: 28 July 2020; Accepted: 27 August 2020; Published: 29 August 2020 Abstract: A large epidemiological study using oximetry to analyze obstructive sleep apnea (OSA) and metabolic comorbidities was performed in Japan; however, reliability and validity of oximetry in the Japanese population remains poorly understood. In this study, oximetry data from the epidemiological study were compared with data from clinically performed polysomnography (PSG) and out-of-center sleep testing (OCST) in epidemiological study participants who later attended our outpatient units. The oxygen desaturation index (ODI) from oximetry showed a moderate positive relationship (correlation coefficient r = 0.561, p < 0.001) with apnea/hypopnea data from PSG/OCST. The area under the receiver operating characteristic curve showed moderate accuracy of this method in the detection of moderate-to-severe or severe OSA. However, the optimal ODI thresholds to detect moderate-to-severe OSA and severe OSA were the same (ODI > 20.1). Oximetry may be a useful tool for screening moderate-to-severe or severe sleep apnea. -

Central Hypoventilation with PHOX2B Expansion Mutation Presenting in Adulthood S Barratt, a H Kendrick, F Buchanan, a T Whittle
919 CASE REPORT Thorax: first published as 10.1136/thx.2006.068908 on 1 October 2007. Downloaded from Central hypoventilation with PHOX2B expansion mutation presenting in adulthood S Barratt, A H Kendrick, F Buchanan, A T Whittle ................................................................................................................................... Thorax 2007;62:919–920. doi: 10.1136/thx.2006.068908 suggested cardiac enlargement and an ECG showed right heart Congenital central hypoventilation syndrome most commonly strain. Oxygen saturation by pulse oximetry (SpO2) on air was presents in neonates with sleep related hypoventilation; late 80% and arterial blood gas analysis on 24% fractional inspired onset cases have occurred up to the age of 10 years. It is oxygen showed hypercapnic respiratory failure (pH 7.21, associated with mutations in the PHOX2B gene, encoding a oxygen tension 8.6 kPa, carbon dioxide tension 10.3 kPa). He transcription factor involved in autonomic nervous system was polycythaemic with haematocrit 64%. He was treated with development. The case history is described of an adult who antibiotics, diuretics, controlled oxygen therapy and face mask presented with chronic respiratory failure due to PHOX2B non-invasive positive pressure ventilation (NIV). mutation-associated central hypoventilation and an impaired From day 2 his daytime oxygenation was satisfactory on low response to hypercapnia. flow oxygen without ventilatory support; he remained on nocturnal NIV. Two attempts to record overnight oximetry without ventilatory support failed: his SpO2 fell below 50% due ongenital central hypoventilation syndrome (CCHS, to apnoea within 30 min of sleep onset and the nursing staff ‘‘Ondine’s Curse’’) classically presents in neonates with recommenced NIV on each occasion. Overnight oximetry on air Csleep-dependent hypoventilation. -

Apnea of Prematurity
www.jpnim.com Open Access eISSN: 2281-0692 Journal of Pediatric and Neonatal Individualized Medicine 2013;2(2):e020213 doi: 10.7363/020213 Advance publication: 2013 Aug 20 Review Apnea of prematurity Piermichele Paolillo, Simonetta Picone Neonatology Department, Neonatal Pathology, Neonatal Intensive Care Unit, Policlinico Casilino Hospital, Rome, Italy Proceedings Proceedings of the 9th International Workshop on Neonatology · Cagliari (Italy) · October 23rd-26th, 2013 · Learned lessons, changing practice and cutting-edge research Abstract Apnea of prematurity (AOP) is one of the most frequent pathologies in the Neonatal Intensive Care Unit, with an incidence inversely related to gestational age. Its etiology is often multi factorial and diagnosis of idiopathic forms requires exclusion of other underlying diseases. Despite being a self- limiting condition which regresses with the maturation of the newborn, possible long-term effects of recurring apneas and the degree of desaturation and bradycardia who may lead to abnormal neurological outcome are not yet clarified. Therefore AOP needs careful evaluation of its etiology and adequate therapy that can be both pharmacological and non-pharmacological. Keywords Apnea of prematurity, idiopathic and secondary apnea, caffeine. Corresponding author Piermichele Paolillo, Neonatology Department, Neonatal Pathology, Neonatal Intensive Care Unit, Ospedale Policlinico Casilino, Rome, Italy; email: [email protected]. How to cite Paolillo P, Picone S. Apnea of Prematurity. J Pediatr Neonat Individual Med. 2013;2(2):e020213. doi: 10.7363/020213. Definition and pathophysiology Apnea of prematurity (AOP) is defined as the cessation of breathing for over 15-20 seconds and is accompanied by oxygen desaturation (SpO2 less than or equal to 80% for ≥ 4 seconds) and/or bradycardia (HR < 2/3 of the basic HR for ≥ 4 seconds) in neonates with a gestational age less then 37 weeks [1, 2]. -

Central-Sleep-Apnea-Facilitator-Guide
Vidya Krishnan and Sutapa Mukherjee for the Sleep Education for Pulmonary Fellows and Practitioners, SRN ATS Committee, 2015 Facilitators Guide I.A. In a patient of this age and presentation the broad category of sleep disorders include: 1) 1) Sleep disordered breathing conditions: OSA, CSA, hypoventilation 2) 2) Insomnia (patients with HF rarely sleep 7-8 hours but usually <4/night and have developed horrible sleep hygiene 3) 3) Parasomnias like REM behavioral disorder (if treated with beta blockers) 4) 4) RLS like symptoms from renal insufficiency/failure, iron deficiency I.B. What are known risk factors for Central Sleep Apnea? 1) age - >65 years old 2) sex – men>women – higher apneic threshold in men 3) heart failure 4) stroke – especially in first 3 months after stroke 5) opioid use 6) renal failure II. A. What is a central sleep apnea? Cessation of airflow for at least 10 seconds, without respiratory effort during the event. II. B. How does your assessment for central sleep apnea risk alter with the given information? - oxycodone can increase risk of central sleep apnea - new onset atrial fibrillation and increased left atrial size can increase the risk of CSA in SHF patient - oropharyngeal exam does not support increased risk of OSA II. C. What are the syndromic presentations of central sleep apnea? What type of central sleep apnea might you expect to see on a sleep study in this patient at this time? 1. Primary central sleep apnea 2. Secondary central sleep apnea a. Cheyne Stokes Respiration b. Secondary to a medical condition – CNS diseases, neuromuscular disease, severe abnormalities in pulmonary mechanics (such as kyphoscoliosis) c. -
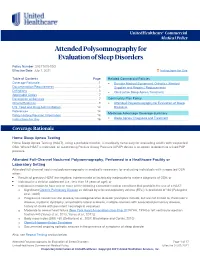
Attended Polysomnography for Evaluation of Sleep Disorders
UnitedHealthcare® Commercial Medical Policy Attended Polysomnography for Evaluation of Sleep Disorders Policy Number: 2021T0334GG Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ....................................................................... 1 • Durable Medical Equipment, Orthotics, Medical Documentation Requirements ...................................................... 3 Supplies and Repairs/ Replacements Definitions ...................................................................................... 3 • Obstructive Sleep Apnea Treatment Applicable Codes .......................................................................... 7 Description of Services ................................................................. 7 Community Plan Policy Clinical Evidence ........................................................................... 9 • Attended Polysomnography for Evaluation of Sleep U.S. Food and Drug Administration ........................................... 14 Disorders References ................................................................................... 14 Medicare Advantage Coverage Summary Policy History/Revision Information ........................................... 16 • Sleep Apnea: Diagnosis and Treatment Instructions for Use ..................................................................... 16 Coverage Rationale Home Sleep Apnea Testing Home Sleep Apnea Testing (HSAT), using a portable monitor, is medically necessary for evaluating