How to Measure and Improve Population Health Webinar Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

State Gun Laws, Gun Ownership, and Mass Shootings in the US: Cross Sectional Time Series BMJ: First Published As 10.1136/Bmj.L542 on 6 March 2019
RESEARCH State gun laws, gun ownership, and mass shootings in the US: BMJ: first published as 10.1136/bmj.l542 on 6 March 2019. Downloaded from cross sectional time series Paul M Reeping,1 Magdalena Cerdá,2 Bindu Kalesan,3 Douglas J Wiebe,4 Sandro Galea,5 Charles C Branas1 1Department of Epidemiology, ABSTRACT a growing divide appears to be emerging between Columbia University, Mailman OBJECTIVE restrictive and permissive states. School of Public Health, 722 To determine whether restrictiveness-permissiveness West 168th Street, New York, of state gun laws or gun ownership are associated NY 10032, USA Introduction 2 with mass shootings in the US. Department of Population Despite an increasing frequency of mass shootings in Health, New York University, DESIGN Langone School of Medicine, the US and the seemingly disproportionate occurrence New York, NY, USA Cross sectional time series. of mass shootings in some states and not others, little 3Department of Community SETTING AND POPULATION research has been carried out to understand state level Health Sciences, Boston US gun owners from 1998-2015. factors that could influence mass shootings.1 A 2018 University School of Public Health, Boston, MA, USA EXPOSURE report pointed to only three studies that had examined 4Department of Biostatistics, An annual rating between 0 (completely restrictive) associations between gun laws and mass shooting Epidemiology & Informatics, and 100 (completely permissive) for the gun laws events.2-5 However, testing the effects of state gun University of Pennsylvania, of all 50 states taken from a reference guide for laws on the occurrence of mass shootings was not the Perelman School of Medicine, Philadelphia, PA, USA gun owners traveling between states from 1998 to primary objective of at least one of these studies and 5Boston University School of 2015. -

Sandro Galea: the Epidemiology of Consequence Sandro Galea Talks to Gary Humphreys About the Power of Epidemiology and the Need to Change the Way We Talk About Health
News Sandro Galea: the epidemiology of consequence Sandro Galea talks to Gary Humphreys about the power of epidemiology and the need to change the way we talk about health. Q: You started your career as a primary health care physician in northern Can- Sandro Galea has devoted the last 20 years to ada. How did you end up focusing on raising awareness and improving our understanding behavioural epidemiology? of the drivers of health and poor health through A: It might seem counter-intuitive, epidemiological studies, writing and teaching. He but I wanted to have more of an impact. is the dean and Robert A Knox Professor at Boston University School of Public Health. From 2010 to 2015, Q: Can you explain that? he was Gelman Professor and Chair of the Department A: Well, I always wanted to make a of Epidemiology at Columbia University. Before that he difference. Even when I was in medical Galea Courtesy of Sandro school, I was very interested in work- Sandro Galea was at the University of Michigan (2005-2010) and the ing in countries where the need for New York Academy of Medicine (2000-2005). His latest health-care professionals was acute. So, book targets a general audience: Well: what we need to talk about when we talk for example, during my training I spent about health. He is also one of the editors of Urban health, a recently published four months in Papua New Guinea and collection of essays. Galea holds a medical degree from the University of Toronto, a couple of months in Guatemala City at graduate degrees from Harvard University and Columbia University. -

Sandro Galea, MD, MPH, Drph CONTACT
Sandro Galea, MD, MPH, DrPH CONTACT INFORMATION Office of the Dean School of Public Health Boston University 715 Albany Street Boston, MA 02118 t: 617.638.4644 f: 617.638.5299 [email protected] DATE OF PREPARATION January 1, 2017 PERSONAL DATA Birthdate: April 24, 1971 Birthplace: Malta Citizenship: United States EDUCATION University of Toronto September 1988-May 1990 Cell and Molecular Biology Toronto, Canada University of Toronto Medical School September 1990-May 1994 Medical Doctor Toronto, Canada Harvard University School of Public Health September 1999-May 2000 Master of Public Health Boston, MA Quantitative Methods Concentration Columbia University School of Public Health June 2000-July 2003 Doctor of Public Health New York, NY Epidemiology Curriculum Vitae: Sandro Galea; page 1 of 103 POSTDOCTORAL TRAINING Rural/Remote Family Medicine Resident and Chief Resident July 1994-July 1996 McMaster University Family Medicine North Thunder Bay, Canada Emergency Medicine Resident July 1996-June 1997 University of Toronto Toronto, Canada LICENSES § Certificant of the Canadian College of Family Physicians § Certificate of Special Competence in Emergency Medicine § MCCQE I and II: Licentiate of the Medical Council of Canada § College of Physicians and Surgeons of Ontario Physician Independent Practice License (#68093) § New York State Office of the Professions Physician Practice License (#234731) § Michigan State Department of Community Health Physician Practice License (#4301086718) PROFESSIONAL ORGANIZATIONS AND SOCIETIES § Canadian College of Family Physicians (1994-present). § American Public Health Association (2000-present). § International Society for Traumatic Stress Studies (2002-present). § Fellow of the Royal Institute of Public Health (2002-present). § American College of Epidemiology (2002-present) § American Academy for the Advancement of Science (2002-present). -

URBAN HEALTH: Evidence, Challenges, and Directions
17 Feb 2005 11:16 AR AR238-PU26-15.tex AR238-PU26-15.sgm LaTeX2e(2002/01/18) P1: IBD 10.1146/annurev.publhealth.26.021304.144708 Annu. Rev. Public Health 2005. 26:341–65 doi: 10.1146/annurev.publhealth.26.021304.144708 Copyright c 2005 by Annual Reviews. All rights reserved First published online as a Review in Advance on August 18, 2004 URBAN HEALTH: Evidence, Challenges, and Directions Sandro Galea and David Vlahov Center for Urban Epidemiologic Studies, New York Academy of Medicine, and Department of Epidemiology, Joseph T. Mailman School of Public Health, Columbia University, New York, NY 10029; email: [email protected]; [email protected] KeyWords multilevel, methods, social epidemiology, cities, mechanisms ■ Abstract Urbanization is one of the most important demographic shifts world- wide during the past century and represents a substantial change from how most of the world’s population has lived for the past several thousand years. The study of urban health considers how characteristics of the urban environment may affect population health. This paper reviews the empirical research assessing urban living’s impact on population health and our rationale for considering the study of urban health as a dis- tinct field of inquiry. The key factors affecting health in cities can be considered within three broad themes: the physical environment, the social environment, and access to health and social services. The methodologic and conceptual challenges facing the study of urban health, arising both from the limitations of the research to date and from the complexities inherent in assessing the relations among complex urban systems, disease causation, and health are discussed. -

Sandro Galea, M.D., M.P.H., Drph Dr Galea Is a Physician and An
Sandro Galea, M.D., M.P.H., DrPH Dr Galea is a physician and an epidemiologist. He is the Robert A. Knox Professor and Dean at the Boston University School of Public Health. Prior to his appointment at Boston University, Dr Galea served as the Gelman Professor and Chair of the Department of Epidemiology at the Columbia University Mailman School of Public Health. He previously held academic and leadership positions at the University of Michigan and at the New York Academy of Medicine. His tenure as Dean of the Boston University School of Public Health has been marked by expansion and innovation. The school launched a new Master of Public Health curriculum, a digital Master of Public Health, synchronous hybrid-flexible Learn from Anywhere teaching, lifelong learning, a public health communication initiative, and a student-alumni mentoring program among others. He has invested substantially in the school’s diversity, equity, and inclusion, agenda, elevating social justice to the heart of the school’s mission, centered around an 11-point plan of action. During this time the school doubled its research funding portfolio and development revenue, rose substantially in the US News rankings, and received full 7-year re-accreditation. Dr Galea’s scholarship has been about the social causes of health, mental health, and the consequences of trauma. His work has been principally funded by the National Institutes of Health, Centers for Disease Control and Prevention, and several foundations. He has published over 850 scientific journal articles, 50 chapters, and 18 books and his research has been featured extensively in current periodicals and newspapers. -

Sandro Galea, MD, MPH, Drph CONTACT INFORMATION Office Of
Sandro Galea, MD, MPH, DrPH CONTACT INFORMATION Office of the Dean School of Public Health Boston University 715 Albany Street Boston, MA 02118 t: 617.638.4644 f: 617.638.5299 [email protected] DATE OF PREPARATION September 1, 2018 PERSONAL DATA Birthdate: April 24, 1971 Birthplace: Malta Citizenship: United States EDUCATION University of Toronto September 1988-May 1990 Cell and Molecular Biology Toronto, Canada University of Toronto Medical School September 1990-May 1994 Medical Doctor Toronto, Canada Harvard University School of Public Health September 1999-May 2000 Master of Public Health Boston, MA Quantitative Methods Concentration Columbia University School of Public Health June 2000-July 2003 Doctor of Public Health New York, NY Epidemiology Curriculum Vitae: Sandro Galea; page 1 of 119 POSTDOCTORAL TRAINING Rural/Remote Family Medicine Resident and Chief Resident July 1994-July 1996 McMaster University Family Medicine North Thunder Bay, Canada Emergency Medicine Resident July 1996-June 1997 University of Toronto Toronto, Canada LICENSES § Certificant of the Canadian College of Family Physicians § Certificate of Special Competence in Emergency Medicine § MCCQE I and II: Licentiate of the Medical Council of Canada § College of Physicians and Surgeons of Ontario Physician Independent Practice License (#68093) § New York State Office of the Professions Physician Practice License (#234731, inactive) § Michigan State Department of Community Health Physician Practice License (#4301086718, inactive) PROFESSIONAL ORGANIZATIONS AND SOCIETIES § Canadian College of Family Physicians (1994-present). § American Public Health Association (2000-present). § International Society for Traumatic Stress Studies (2002-present). § Fellow of the Royal Institute of Public Health (2002-present). § American College of Epidemiology (2002-present) § American Academy for the Advancement of Science (2002-present). -

Dr. Sandro Galea, Boston University School of Public Health
Gun Violence Prevention Challenge Summit & Hack-a-thon April 13 – 15, 2018 | Boston, Massachusetts Sandro Galea, a physician and an epidemiologist, is dean and Robert A. Knox Professor at Boston University School of Public Health. He previously held academic and leadership positions at Columbia University, the University of Michigan, and the New York Academy of Medicine. Dr. Galea’s scholarship has been at the intersection of social and psychiatric epidemiology with a focus on the behavioral health consequences of trauma, including firearms. He has published more than 700 scientific journal articles, 50 chapters, and 13 books, and his research has been featured extensively in current periodicals and newspapers. His latest book, Healthier: Fifty Thoughts on the Foundations of Population Health was published by Oxford University Press in 2017. Galea holds a medical degree from the University of Toronto and graduate degrees from Harvard University and Columbia University. He also holds an honorary doctorate from the University of Glasgow. Galea was named one of Time magazine’s epidemiology innovators, and has been listed as one of the “World’s Most Influential Scientific Minds”. He is past president of the Society for Epidemiologic Research and of the Interdisciplinary Association for Population Health Science. He is an elected member of the National Academy of Medicine and the American Epidemiological Society. Galea has received several lifetime achievement awards for his research, including the Rema Lapouse Award from the American Public Health Association and the Robert S. Laufer Memorial Award from the International Society for Traumatic Stress Studies. He is a regular contributor to Fortune magazine and has published widely in the lay press, including the Wall Street Journal, Harvard Business Review, the Boston Globe, and The New York Times. -

Urban Health Populations, Methods, and Practice
Chapter 1 Urban Health Populations, Methods, and Practice Sandro Galea and David Vlahov 1.0. WHAT IS A CITY AND WHAT IS “URBAN HEALTH”? We all know what cities are; or at least we think we do. However, it is more likely that each of our personal experiences has shaped what we think of when we discuss “cities” and that each of us has a different image of “city” in our own head. We may be in good company. Saul Bellow, the novelist and Nobel Prize laureate, in dis- cussing how Americans think of New York City, suggested: “ That is perhaps like ask- ing how Scotsmen feel about the Loch Ness monster. It is our legendary phenomenon, our great thing, our world-famous impossibility . New York is stir- ring, insupportable, agitated, ungovernable, demonic. No single individual can judge it adequately” (New York Times, 1970). Indeed, cities can defeat definition and challenge the imagination. Cities are elegant, sophisticated places. Think of Piccadilly Circus in London, the Arc de Triomphe in Paris, or the Copacabana in Rio De Janeiro. But cities are also dense, teeming, and dangerous places. Think of the squatter colonies of Lagos and parts of Los Angeles or New York City. Cities can be distinctive (there is only one Paris) or can look monotonously alike (think of any number of North American mid-size cities). Cities can be small, compact areas that are immediately walkable, and can be vast, extensive, automobile-dependent metro- politan areas that are disconnected, homogenous, and pedestrian-hostile. In short, cities, and by extension the urban experience, can represent diverse conditions within which people live, and represent a range of human experiences. -
Appointment of Dean Sandro Galea As the Robert A
Boston University Office of the Provost Professor Jean Morrison, University Provost and Chief Academic Officer One Silber Way Boston, Massachusetts 02215 T 617-353-2230 F 617-353-6580 www.bu.edu/provost TO: Boston University Faculty FROM: Jean Morrison, University Provost and Chief Academic Officer DATE: January 19, 2016 SUBJECT: Appointment of Dean Sandro Galea as the Robert A. Knox Professor I am delighted to announce that Sandro Galea, Dean of the Boston University School of Public Health and Professor of Epidemiology, has been named as the Robert A. Knox Professor. The Robert A. Knox Professorship was established in 2012 as a result of the generosity and vision of businessman, philanthropist, and BU Board of Trustees Chair, Robert Knox (CAS ’74, Questrom ’75). The Professorship is designated to support a faculty member anywhere in the University who demonstrates excellence in scholarship, research and teaching, as well as impact on society. An internationally recognized physician, epidemiologist, scholar, and leader in defining the future of public health research, education and practice, Professor Galea is the ideal faculty member to hold this distinguished professorship. Professor Galea’s current research interests are focused on the social production of health of urban populations. His research examines the causes of brain disorders, particularly common mood-anxiety disorders and substance abuse. In addition to his focus on urban health, Professor Galea’s scholarship includes a significant global dimension. He is a leading expert on the health consequences of mass trauma and conflict worldwide, including the September 11 attacks, Hurricane Katrina, conflicts in sub-Saharan Africa, and combat in Iraq and Afghanistan. -

Appointment of Dr. Sandro Galea As Dean of the School of Public Health
Boston University Office of the Provost Professor Jean Morrison, University Provost and Chief Academic Officer One Silber Way Boston, Massachusetts 02215 T 617-353-2230 F 617-353-6580 www.bu.edu/provost TO: Boston University Faculty and Staff FROM: Jean Morrison, University Provost and Chief Academic Officer Karen Antman, Provost of the Medical Campus and Dean of the School of Medicine DATE: September 12, 2014 SUBJECT: Appointment of Dr. Sandro Galea as Dean of the School of Public Health This past winter, we began a national-level search for a new Dean of the School of Public Health. We sought candidates who would bring the proven leadership, strategic vision, and track record of research and academic accomplishment essential to chart the future of the School of Public Health. After a rigorous and competitive search process that considered many exceptional candidates and thorough consultation with our Search Advisory Committee, we are delighted to join President Brown in announcing the appointment of Dr. Sandro Galea as Dean of the School of Public Health. Dr. Galea is the Gelman Professor and Chair in the Department of Epidemiology at the Columbia University Mailman School of Public Health – a position that includes oversight of more than 150 faculty members with a total grant portfolio of more than $100 million, and which trains 400 students, including Master’s level, doctoral students and post-doctoral fellows. An elected member of the Institute of Medicine of the National Academy of Sciences, Dr. Galea has spent his career as both an accomplished physician and teacher of epidemiology, focusing his research on the social production of health of urban populations. -

SANDRO GALEA, MD, MPH, Drph
SANDRO GALEA, MD, MPH, DrPH HEALTH NOT HEALTHCARE: WHAT WE SHOULD TALK ABOUT WHEN WE TALK ABOUT HEALTH JANUARY 24, 2019 4:00 P.M. 208 LIGHT HALL SPONSORED BY: DEPARTMENT OF BIOMEDICAL INFORMATICS VANDERBILT PRIZE IN BIOMEDICAL SCIENCE LECTURE ANGELIKA AMON PH.D. Kathleen and Curtis Marble Professor in Cancer Research Professor of Biology, Koch Institute for Integrative Cancer Research at MIT January 31, 2019 208 Light Hall / 4:00 P.M. 01-24-19 DLS Galea - BK-CH .indd 1 1/11/19 12:35 PM SANDRO GALEA, MD, MPH, DrPH HEALTH NOT HEALTHCARE: WHAT WE SHOULD DEAN AND ROBERT A. KNOX PROFESSOR, TALK ABOUT WHEN WE TALK ABOUT HEALTH SCHOOL OF PUBLIC HEALTH, BOSTON UNIVERSITY The United States spends far more on health per capita than Sandro Galea, a physician, epidemiologist, and author, is dean and any other country. But our health outcomes are worse than any Robert A. Knox Professor at Boston University School of Public Health. other high income country and getting worse. We have now had He previously held academic and leadership positions at Columbia a decline in national life expectancy every year for the past 3 University, the University of Michigan, and the New York Academy of years—the worst downturn since the 1918 flu pandemic. Why Medicine. He has published more than 750 scientific journal articles, 50 is this? Ultimately, this is because we are not investing in health; chapters, and 13 books, and his research has been featured extensively in we are investing in healthcare. This presentation will discuss what current periodicals and newspapers. -
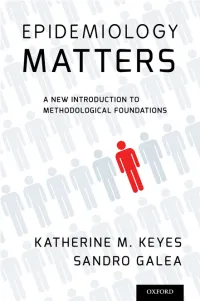
Epidemiology Matters : a New Introduction to Methodological Foundations / Katherine M
Epidemiology Matters Epidemiology Matters A New Introduction to Methodological Foundations KATHERINE M. KEYES Department of Epidemiology, Columbia University SANDRO GALEA Department of Epidemiology, Columbia University 1 1 Oxford University Press is a department of the University of Oxford. It furthers the University’s objective of excellence in research, scholarship, and education by publishing worldwide. Oxford New York Auckland Cape Town Dar es Salaam Hong Kong Karachi Kuala Lumpur Madrid Melbourne Mexico City Nairobi New Delhi Shanghai Taipei Toronto With offices in Argentina Austria Brazil Chile Czech Republic France Greece Guatemala Hungary Italy Japan Poland Portugal Singapore South Korea Switzerland Thailand Turkey Ukraine Vietnam Oxford is a registered trademark of Oxford University Press in the UK and certain other countries. Published in the United States of America by Oxford University Press 198 Madison Avenue, New York, NY 10016 © Oxford University Press 2014 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without the prior permission in writing of Oxford University Press, or as expressly permitted by law, by license, or under terms agreed with the appropriate reproduction rights organization. Inquiries concerning reproduction outside the scope of the above should be sent to the Rights Department, Oxford University Press, at the address above. You must not circulate this work in any other form and you must impose this same condition on any acquirer. Library of Congress Cataloging-in-Publication Data Keyes, Katherine M., author. Epidemiology matters : a new introduction to methodological foundations / Katherine M. Keyes, Sandro Galea.