Commonly Missed Uncommon Orthopedic Injuries, Part 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Influence of Altered Lower-Extremity Kinematics on Patellofemoral Joint Dysfunction: a Theoretical Perspective
The Influence of Altered Lower-Extremity Kinematics on Patellofemoral Joint Dysfunction: A Theoretical Perspective Christopher M. Powers, PT, PhD 1 Although patellofemoral pain (PFP) is recognized as being one of the most common disorders of It has been recognized by sev- the lower extremity, treatment guidelines and underlying rationales remain vague and controver- eral authors that the patel- sial. The premise behind most treatment approaches is that PFP is the result of abnormal patellar lofemoral joint may be influenced CLINICAL COMMENTARY tracking and/or patellar malalignment. Given as such, interventions typically focus on the joint by the segmental interactions of itself and have traditionally included strengthening the vastus medialis oblique, taping, bracing, the lower extremity.6,7,21,27,34,45 Ab- soft tissue mobilization, and patellar mobilization. More recently, it has been recognized that the normal motion(s) of the tibia and patellofemoral joint and, therefore, PFP may be influenced by the interaction of the segments and femur in the transverse and frontal joints of the lower extremity. In particular, abnormal motion of the tibia and femur in the transverse and frontal planes may have an effect on patellofemoral joint mechanics. With this in planes are believed to have an mind, interventions aimed at controlling hip and pelvic motion (proximal stability) and ankle/foot effect on patellofemoral joint me- motion (distal stability) may be warranted and should be considered when treating persons with chanics and therefore PFP. An un- patellofemoral joint dysfunction. The purpose of this paper is to provide a biomechanical derstanding of how lower- overview of how altered lower-extremity mechanics may influence the patellofemoral joint. -

A Simultaneous Bilateral Quadriceps and Patellar Tendons Rupture In
Tao et al. BMC Musculoskeletal Disorders (2020) 21:179 https://doi.org/10.1186/s12891-020-03204-6 CASE REPORT Open Access A simultaneous bilateral quadriceps and patellar tendons rupture in patients with chronic kidney disease undergoing long- term hemodialysis: a case report Zhengbo Tao†, Wenbo Liu†, Weifeng Ma, Peng Luo, Shengpeng Zhi and Renyi Zhou* Abstract Background: The incidence of rupture of the quadriceps or patellar tendon s is low, especially that of bilateral quadriceps tendon rupture, and it is generally considered a complication secondary to chronic systemic disorders. We report two rare cases of simultaneous bilateral tendon rupture affecting the extensor function of the knee in patients with chronic kidney disease who have been treated with long-term haemodialysis. Case presentation: Two young males with a history of chronic kidney disease who were being treated with long- term haemodialysis presented to our hospital with clinical signs of disruption of the extensor mechanism of the knee. One patient was diagnosed with bilateral quadriceps tendon rupture, and the other patient had bilateral patellar tendon rupture. They underwent surgical repair of the tendons, and their knees were actively mobilized during physiotherapy. Conclusion: Bilateral quadriceps or patellar tendons rupture is a rare occurrence in patients with chronic kidney disease who are being treated with long-term haemodialysis. Timely surgical treatment and scientific physiotherapy can lead to good recovery of knee joint function. Keywords: Quadriceps tendon, Patellar tendon, Rupture, Haemodialysis, Chronic kidney disease Background undergoing long-term haemodialysis. There were only The disruption of the extensor mechanism of the knee is two cases of simultaneous bilateral quadriceps or patel- commonly caused by fractures of the patella; the inci- lar tendons rupture, and both of them had undergone dence of rupture of the quadriceps or patellar tendons is long-term haemodialysis. -

Closure of Patellar Tendon Defect in ACL Reconstruction
Systematic Review Closure of Patellar Tendon Defect in Anterior Cruciate Ligament Reconstruction With BoneePatellar TendoneBone Autograft: Systematic Review of Randomized Controlled Trials Rachel M. Frank, M.D., Randy Mascarenhas, M.D., Marc Haro, M.D., Nikhil N. Verma, M.D., Brian J. Cole, M.D., M.B.A., Charles A. Bush-Joseph, M.D., and Bernard R. Bach Jr., M.D. Purpose: This study aimed to systematically review the highest level of evidence on anterior cruciate ligament (ACL) reconstruction with boneepatellar tendonebone (BPTB) autografts with patellar tendon defect closure versus no closure after surgery. Methods: We performed a systematic review of multiple medical databases using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Level I and Level II randomized controlled trials comparing patellar tendon defect closure to no closure during ACL reconstruction with BPTB autografts were included. Two inde- pendent reviewers analyzed all studies. Descriptive statistics were calculated. Study methodological quality was analyzed using the Modified Coleman Methodology Score (MCMS) and Jadad scale. Results: Four studies with a combined 221 patients (154 male patients and 67 female patients) with an average age of 26.6 Æ 2.4 years (range, 17 to 54 years) were included. All studies randomized patients before surgery into ACLR with BPTB autografts either with patellar tendon defect closure or without closure. There were no differences in clinical outcomes (Lysholm score, Tegner scale, International Knee Documentation Committee [IKDC] classification, modified Larsen score, and Lauridsen rating) between groups. There were no significant differences in knee pain between groups. All studies reported imaging findings of the patellar tendon defect, with 2 studies showing no difference in appearance between groups, one study showing excessive scar formation with defect repair, and one study showing improved restoration of normal tendon appearance with defect repair. -

Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions
Review Article Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions Abstract Robert D. Bronstein, MD The knee is one of the most commonly injured joints in the body. Its Joseph C. Schaffer, MD superficial anatomy enables diagnosis of the injury through a thorough history and physical examination. Examination techniques for the knee described decades ago are still useful, as are more recently developed tests. Proper use of these techniques requires understanding of the anatomy and biomechanical principles of the knee as well as the pathophysiology of the injuries, including tears to the menisci and extensor mechanism, patellofemoral conditions, and osteochondritis dissecans. Nevertheless, the clinical validity and accuracy of the diagnostic tests vary. Advanced imaging studies may be useful adjuncts. ecause of its location and func- We have previously described the Btion, the knee is one of the most ligamentous examination.1 frequently injured joints in the body. Diagnosis of an injury General Examination requires a thorough knowledge of the anatomy and biomechanics of When a patient reports a knee injury, the joint. Many of the tests cur- the clinician should first obtain a rently used to help diagnose the good history. The location of the pain injured structures of the knee and any mechanical symptoms were developed before the avail- should be elicited, along with the ability of advanced imaging. How- mechanism of injury. From these From the Division of Sports Medicine, ever, several of these examinations descriptions, the structures that may Department of Orthopaedics, are as accurate or, in some cases, University of Rochester School of have been stressed or compressed can Medicine and Dentistry, Rochester, more accurate than state-of-the-art be determined and a differential NY. -

Patellar Tendinopathy: Some Aspects of Basic Science and Clinical Management
346 Br J Sports Med 1998;32:346–355 Br J Sports Med: first published as 10.1136/bjsm.32.4.346 on 1 December 1998. Downloaded from OCCASIONAL PIECE Patellar tendinopathy: some aspects of basic science and clinical management School of Human Kinetics, University of K M Khan, N MaVulli, B D Coleman, J L Cook, J E Taunton British Columbia, Vancouver, Canada K M Khan J E Taunton Tendon injuries account for a substantial tendinopathy, and the remainder to tendon or Victorian Institute of proportion of overuse injuries in sports.1–6 tendon structure in general. Sport Tendon Study Despite the morbidity associated with patellar Group, Melbourne, tendinopathy in athletes, management is far Victoria, Australia 7 Anatomy K M Khan from scientifically based. After highlighting The patellar tendon, the extension of the com- J L Cook some aspects of clinically relevant basic sci- mon tendon of insertion of the quadriceps ence, we aim to (a) review studies of patellar femoris muscle, extends from the inferior pole Department of tendon pathology that explain why the condi- of the patella to the tibial tuberosity. It is about Orthopaedic Surgery, tion can become chronic, (b) summarise the University of Aberdeen 3 cm wide in the coronal plane and 4 to 5 mm Medical School, clinical features and describe recent advances deep in the sagittal plane. Macroscopically it Aberdeen, Scotland, in the investigation of this condition, and (c) appears glistening, stringy, and white. United Kingdom outline conservative and surgical treatment NMaVulli options. BLOOD SUPPLY Department of The blood supply has been postulated to con- 89 Medicine, University tribute to patellar tendinopathy. -

Patellar Ligament Rupture During Total Knee Arthroplasty in an Ochronotic Patient
CASE REPORT Acta Orthop Traumatol Turc 2014;48(3):367-370 doi: 10.3944/AOTT.2014.3245 Patellar ligament rupture during total knee arthroplasty in an ochronotic patient Madan Mohan SAHOO, Sudhir Kumar MAHAPATRA, Gopal Chandra SETHI, Sunil Kumar DASH SCB Medical College, Cuttack, India Ochronotic arthropathy mainly involves the spine and large joints. Along with blackening of the joint, degeneration rapidly progresses mostly in the knee, resulting in symptoms by the 4th or 5th decade. As the role of medical treatment and joint conservation surgeries are limited in the early stages, joint replacement is the only effective option in one third of patients. We present a case of the unique com- plication of patellar ligament rupture during total knee replacement (TKR) of an ochronotic joint. A 51-year-old male presented with bilateral severe tricompartmental osteoarthritis with varus deformi- ties and restriction of motion. Bilateral TKR was performed. At the 28-month follow-up, the patient was walking pain free with acceptable position of implants in radiographs. To our knowledge this is the first report of rupture of the patellar ligament during TKR of an ochronotic joint. We propose ap- propriate preoperative preparation and greater care in the handling of the tendon during TKR of an ochronotic joint in order to avoid complication. Key words: Ligament rupture; ochronosis; total knee replacement. Blackening of the joint may be due to endogenous ochro- Considering that the knee is the most commonly re- nosis (deficiency of homogentisic acid oxidase) or, rarely, placed symptomatic joint, any complication occurring exogenous ochronosis (due to accumulation of hydro- during total knee replacement (TKR) is of great impor- quinone, resorcinol, phenol, mercury or picric acid). -

Focal Knee Swelling Clinical Presentation
Focal Knee Swelling Clinical Presentation Click for referral info for MSK Triage Click for History and Examination more info Click for Medial or Lateral Focal Click for Baker's Cyst more Swelling Bursitis more info info Consider meniscal Cysts Refer for Weight Bearing Refer for diagnostic Assessment and Management X-ray AP and Lateral ultrasound scan • depends on its aetiology • have a low threshold for performing, or referring for, aspiration to rule out septic arthritis Ganglion or Meniscal Cyst · likely to be a degenerative tear Osteoarthritis Normal · majority can be treated conservatively confirmed Non-septic Bursitis Click for Click for more Septic Bursitis more info info Conservative Management Refer for diagnostic Manage as per (where appropriate) ultrasound scan Osteoarthritis pathway Self-management for 6 Immediate referral to weeks secondary care Click for Refer to MSK triage more Manage as per See pathway If no improvement with info pathology Knee Pain Management conservative management Physio for 6 weeks If no improvement with self-management Physio to refer to MSK triage Click for more If no improvement with physio info Back to History and examination pathway History Ask about: · History of trauma · Pain: nature, onset · Stiffness · Fever, systemic illness · Locking or clicking · Past medical history · Occupational and recreational activities that may have precipitated pathology Examination · Look: assess location of swelling (generalised/media/lateral/ popliteal fossa), overlying erythema, lesions to overlying skin · Feel: -

Patellar Tendon Debridement Surgery
175 Cambridge Street, 4th floor Boston, MA 02114 Tel: 617-726-7500 PATELLAR TENDON DEBRIDEMENT SURGERY PREOPERATIVE INSTRUCTIONS Here are guidelines that will help you prepare for surgery: WITHIN ONE MONTH BEFORE SURGERY: The doctor will see you in the office. The doctor or his associate will do a preoperative history and physical examination and complete the necessary paperwork. He will write preoperative hospital orders and order laboratory tests. These tests usually include a complete blood count (and also electrocardiogram for patients over 40 years old.) SEVERAL DAYS BEFORE SURGERY: Wash the knee several times a day to get it as clean as you can. This decreases the risk of infection. Be careful not to get any scratches, cuts, sunburn, poison ivy, etc. The skin has to be in very good shape to prevent problems. You do not need to shave the knee. THE DAY BEFORE SURGERY: Please contact the doctor’s office to get the exact time you should report to the hospital for surgery. You can have nothing to eat or drink after midnight on the evening before surgery. It is very important to have a completely empty stomach prior to surgery for anesthesia safety reasons. If you have to take medication, you can take the medication with a sip of water early in the morning prior to surgery (but later tell the anesthesiologist you have done so). THE DAY OF SURGERY: Surgery is performed in the Wang building at MGH and at the Orthopedic Ambulatory Surgery Center at Mass General West in Waltham. • nothing to eat or drink • For surgery at MGH main campus in Boston: Report directly to the 12th floor of the Lunder Building, Center for Preoperative Care at Massachusetts General Hospital, two hours prior to surgery. -

Recurrent Unremitting Patellar Tendonitis/ Tendonosis Rehabilitation Program
Page 1 of 3 Recurrent Unremitting Patellar Tendonitis/ Tendonosis Rehabilitation Program I. Phase I Goals: Diminish pain and inflammation Promote tendon healing Improve quadriceps strength Enhance flexibility Control functional stresses Treatment Regimen: • Hot packs applied to knee • Ultrasound to patellar tendon • Transverse friction massage • Warm-up bicycle (10-12 min.) • Stretch (hamstrings quadriceps, gastroc) • Application of pain stimulation to each side of patella tendon or infra-patellar fat pad x 10 minutes • Electrical stimulation parameters • Waveform: Russian • Frequency: 2500 H2 pulse; width: 200 MS; Rate: 50/sec • 60 pulses per second (pps) • duty cycle 10 on/10 off; ramp of 1 second • pad placement- 1”x1” electrodes placed on each side of inflamed/painful tendon (After 3 minutes, palpate tendon, should be less painful and becoming numb, if not, move electrodes) • Quadriceps strengthening program (Level I) • E-stim to quadriceps* • Quad sets* • SLR flexion* • Hip adduction/abduction* • Vertical squats (tilt board) • Hip flexion/extension • Toe-calf raises • Bicycle (15-20 min.) *Monitor subjective pain level response (goal level 5-7) • Pool program • Stretch (aggressive stretching) • Laser • Cryotherapy II. Phase II Emphasize eccentric training for quadriceps Goals: Gradual increase stress to patellar tendon Enhance quadriceps strength Improve flexibility Gradual increase functional activities Copyright © by the Advanced Continuing Education Institute, LLC. AdvancedCEU.com. All Rights Reserved. Any redistribution, alteration, -
Knee Extensor Mechanism Reconstruction with Complete Extensor Allograft After Failure of Patellar Tendon Repair
A Case Report & Literature Review Knee Extensor Mechanism Reconstruction With Complete Extensor Allograft After Failure of Patellar Tendon Repair Savyasachi C. Thakkar, MD, Nigel Hsu, MD, and Erik A. Hasenboehler, MD Case Report Abstract A 30-year-old healthy man landed on an empty glass fish Disruptions of the extensor mechanism of the knee tank, resulting in a traumatic right-knee arthrotomy. On ini- may be bony or tendinous in nature. The consequences tial evaluation, the patient had a negative straight-leg-raise test of such disruptions are not favorable because they and impaired knee extension. The patient was taken urgently prevent normal function of the knee, which is critical to the operating room for irrigation and débridement and for independent ambulation. We report on a 30-year- concurrent repair of the patellar tendon laceration. Antibiotic old man who underwent a successful knee extensor prophylaxis with 2 g of intravenous (IV) cefazolin was given mechanism reconstruction with allograft after his initial in the emergency room. tendon repair failed. Intraoperatively, after visualizing the patellar tendon lac- eration and excluding any associated chondral lesions, we proceeded with extensive débridement and irrigation using 9 L of normal saline pulse lavage. After we achieved a clean he extensor mechanism of the knee comprises the site, we proceeded to repair the patellar tendon using No. 2 quadriceps tendon, the patella, and the patellar tendon. FiberWire sutures (Arthrex, Naples, Florida) with a classic AJO8 TThe extensor mechanism may be damaged by injury Krackow repair consisting of 2 sutures run in a 4-row fashion to these structures, with consequences such as the inability to through the patella and the patellar tendon. -

Simultaneous Bilateral Rupture of Patellar Tendons in Diabetic Hemodialysis Patient: a Case Report
Caspian J Intern Med 2018; 9(3):306-311 DOI: 10.22088/cjim.9.3.306 Case Report Simultaneous bilateral rupture of patellar tendons in diabetic hemodialysis patient: A case report 1 Ali Torkaman (MD) Abstract Alireza Yousof Gomrokchi (MD) 1* Background: Bilateral rupture of the patellar tendon is a very rare injury, which takes Omid Elahifar (MD) 1 place in relation to chronic systemic diseases. These injuries are known causes. Some of these Pooyan Barmayoon (MD) 2 Seyedeh Fahimeh Shojaei (MSc) 2 causes are particular in patellar tendon rupture and another are in quadriceps tendon rupture. Case presentation: 70-year-old diabetic man with simultaneous bilateral patellar tendon disruption of proximal insertion without trauma, receiving long-term hemodialysis. Conclusions: In the present study, we report a case of patellar tendon rupture that has two 1. Bone and Joint Reconstruction differences with literature: first, renal failure is a known risk factor for quadriceps tendon Research Center, Shafa Orthopedic rupture, and secondly, the prevalent age of patellar tendon rupture is less than 40 years. Hospital, Iran University of Clinical picture, diagnosis, pathogenesis and treatment are discussed. Finally, the literature Medical Sciences, Tehran, Iran 2. Firoozgar Clinical Research and is reviewed based on previous studies. Development Center, (FCRDC) , Keywords: Bilateral, Hemodialysis, Patellar tendon, Rupture Iran University of Medical Sciences, (IUMS) , Tehran, Iran Citation: Torkaman A, Yousof Gomrokchi A, Elahifar O, et al. Simultaneous bilateral rupture of patellar tendons in diabetic hemodialysis patient: A case report. Caspian J Intern Med 2018; 9(3):306- 311. The disruption of the extensor mechanism of the knee is commonly caused by the fracture of the patella in most cases. -
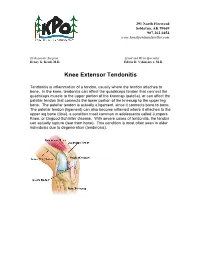
Knee Extensor Tendonitis
291 North Fireweed Soldotna, AK 99669 907-262-6454 www.kenaipeninsulaortho.com ______________________________________________________________________________________ Orthopaedic Surgeon: Hand and Wrist Specialist: Henry G. Krull, M.D. Edwin D. Vyhmeister, M.D. Knee Extensor Tendonitis Tendonitis is inflammation of a tendon, usually where the tendon attaches to bone. In the knee, tendonitis can affect the quadriceps tendon that connect the quadriceps muscle to the upper portion of the kneecap (patella), or can affect the patellar tendon that connects the lower portion of the kneecap to the upper leg bone. The patellar tendon is actually a ligament, since it connects bone to bone. The patellar tendon (ligament) can also become inflamed where it attaches to the upper leg bone (tibia), a condition most common in adolescents called Jumpers Knee, or Osgood-Schlatter disease. With severe cases of tendonitis, the tendon can actually rupture (tear from bone). This condition is most often seen in older individuals due to degeneration (tendinosis). 291 North Fireweed Soldotna, AK 99669 907-262-6454 www.kenaipeninsulaortho.com Symptoms: Pain is the hallmark of extensor tendonitis, and is located either just above the patella (quadriceps tendonitis), or just below the patella (patellar tendonitis). Sometimes there is an injury, but tendonitis is more common with overuse and under-conditioning. There is occasionally swelling and warmth over the inflamed tendon. The joint may become stiff, but range of motion is often reduced due to pain. Tenderness is present over the affected tendon. Cause: Extensor tendonitis is often caused by injury, particularly sports injuries, or overuse. Tendonitis can often be caused by inadequate stretching prior to exercise, or increasing an exercise program too rapidly.