Drospirenone)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Optum Essential Health Benefits Enhanced Formulary PDL January
PENICILLINS ketorolac tromethamineQL GENERIC mefenamic acid amoxicillin/clavulanate potassium nabumetone amoxicillin/clavulanate potassium ER naproxen January 2016 ampicillin naproxen sodium ampicillin sodium naproxen sodium CR ESSENTIAL HEALTH BENEFITS ampicillin-sulbactam naproxen sodium ER ENHANCED PREFERRED DRUG LIST nafcillin sodium naproxen DR The Optum Preferred Drug List is a guide identifying oxacillin sodium oxaprozin preferred brand-name medicines within select penicillin G potassium piroxicam therapeutic categories. The Preferred Drug List may piperacillin sodium/ tazobactam sulindac not include all drugs covered by your prescription sodium tolmetin sodium drug benefit. Generic medicines are available within many of the therapeutic categories listed, in addition piperacillin sodium/tazobactam Fenoprofen Calcium sodium to categories not listed, and should be considered Meclofenamate Sodium piperacillin/tazobactam as the first line of prescribing. Tolmetin Sodium Amoxicillin/Clavulanate Potassium LOW COST GENERIC PREFERRED For benefit coverage or restrictions please check indomethacin your benefit plan document(s). This listing is revised Augmentin meloxicam periodically as new drugs and new prescribing LOW COST GENERIC naproxen kit information becomes available. It is recommended amoxicillin that you bring this list of medications when you or a dicloxacillin sodium CARDIOVASCULAR covered family member sees a physician or other penicillin v potassium ACE-INHIBITORS healthcare provider. GENERIC QUINOLONES captopril ANTI-INFECTIVES -

MIRENA Data Sheet Vx3.0, CCDS 25 1
NEW ZEALAND DATA SHEET 1. PRODUCT NAME MIRENA 52 mg intrauterine contraceptive device (release rate: 20 microgram/24 hours) 2. QUALITATIVE AND QUANTITATIVE COMPOSITION MIRENA is an intrauterine system (IUS) containing 52 mg levonorgestrel. For details of release rates, see Section 5.2. For the full list of excipients, see Section 6.1. 3. PHARMACEUTICAL FORM MIRENA consists of a white or almost white drug core covered with an opaque membrane, which is mounted on the vertical stem of a T-body. The vertical stem of the levonorgestrel intrauterine system is loaded in the insertion tube at the tip of the inserter. Inserter components are an insertion tube, plunger, flange, body and slider. The white T-body has a loop at one end of the vertical stem and two horizontal arms at the other end. Brown coloured removal threads are attached to the loop. The T-body of MIRENA contains barium sulfate, which makes it visible in X-ray examination. The IUS and inserter are essentially free from visible impurities. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Contraception Treatment of idiopathic menorrhagia provided there is no underlying pathology. Prevention of endometrial hyperplasia during estrogen replacement therapy MIRENA Data Sheet Vx3.0, CCDS 25 1 4.2 Dose and method of administration MIRENA is inserted into the uterine cavity. One administration is effective for five years. The in vivo dissolution rate is approximately 20 microgram/24 hours initially and is reduced to approximately 18 microgram/24 hours after 1 year and to 10 microgram/24 hours after five years. The mean dissolution rate of levonorgestrel is about 15 microgram /24 hours over the time up to five years. -

Pharmacokinetic Drug–Drug Interactions Among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients
International Journal of Molecular Sciences Review Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients Marta Kara´zniewicz-Łada 1 , Anna K. Główka 2 , Aniceta A. Mikulska 1 and Franciszek K. Główka 1,* 1 Department of Physical Pharmacy and Pharmacokinetics, Poznan University of Medical Sciences, 60-781 Pozna´n,Poland; [email protected] (M.K.-Ł.); [email protected] (A.A.M.) 2 Department of Bromatology, Poznan University of Medical Sciences, 60-354 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-(0)61-854-64-37 Abstract: Anti-epileptic drugs (AEDs) are an important group of drugs of several generations, rang- ing from the oldest phenobarbital (1912) to the most recent cenobamate (2019). Cannabidiol (CBD) is increasingly used to treat epilepsy. The outbreak of the SARS-CoV-2 pandemic in 2019 created new challenges in the effective treatment of epilepsy in COVID-19 patients. The purpose of this review is to present data from the last few years on drug–drug interactions among of AEDs, as well as AEDs with other drugs, nutrients and food. Literature data was collected mainly in PubMed, as well as google base. The most important pharmacokinetic parameters of the chosen 29 AEDs, mechanism of action and clinical application, as well as their biotransformation, are presented. We pay a special attention to the new potential interactions of the applied first-generation AEDs (carba- Citation: Kara´zniewicz-Łada,M.; mazepine, oxcarbazepine, phenytoin, phenobarbital and primidone), on decreased concentration Główka, A.K.; Mikulska, A.A.; of some medications (atazanavir and remdesivir), or their compositions (darunavir/cobicistat and Główka, F.K. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -

Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva
REVIEW ARTICLE Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva Philip N. Patsalos, FRCPath, PhD*† and Dave J. Berry, FRCPath, PhD† INTRODUCTION Abstract: Blood (serum/plasma) antiepileptic drug (AED) therapeu- Measuring antiepileptic drugs (AEDs) in serum or tic drug monitoring (TDM) has proven to be an invaluable surrogate plasma as an aid to personalizing drug therapy is now a well- marker for individualizing and optimizing the drug management of established practice in the treatment of epilepsy, and guidelines patients with epilepsy. Since 1989, there has been an exponential are published that indicate the particular features of epilepsy and increase in AEDs with 23 currently licensed for clinical use, and the properties of AEDs that make the practice so beneficial.1 recently, there has been renewed and extensive interest in the use of The goal of AED therapeutic drug monitoring (TDM) is to saliva as an alternative matrix for AED TDM. The advantages of saliva ’ fl optimize a patient s clinical outcome by supporting the man- include the fact that for many AEDs it re ects the free (pharmacolog- agement of their medication regimen with the assistance of ically active) concentration in serum; it is readily sampled, can be measured drug concentrations/levels. The reason why TDM sampled repetitively, and sampling is noninvasive; does not require the has emerged as an important adjunct to treatment with the expertise of a phlebotomist; and is preferred by many patients, AEDs arises from the fact that for an individual patient -

Results of a Nationwide Veterans Administration Cooperative Study Comparing the Efficacy and Toxicity of Carbamazepine, Phenobarbital, Phenytoin, and Primidone
Epilepsin, 28(Suppl. 3):SSO-S58, 1987 Raven Press, Ltd., New York 0 International League Against Epilepsy Results of a Nationwide Veterans Administration Cooperative Study Comparing the Efficacy and Toxicity of Carbamazepine, Phenobarbital, Phenytoin, and Primidone Dennis B. Smith, "Richard H. Mattson, ?Joyce A. Cramer, $Joseph F. Collins, §Robert A. Novelly, [[BruceCraft, and the Weterans Administration Epilepsy Cooperative Study Group Good Samaritan Hospital & Medical Center, Portland Oregon; *Yale University School of Medicine, New Haven, Connecticut; $Veterans Administration Cooperative Studies Program, Perry Point, Maryland; *f§Veterans Administration Hospital, West Haven, Connecticut; and llNeurology Service, Veterans Administration Medical Center, Augusta, Georgia, U.S.A. Summary: In 1985 a 5-year multicenter Veterans Admin- sociated with significantly lower incidences of intolerable istration Cooperative Study was completed that com- side effects than were primidone or phenobarbital. A be- pared the efficacy and toxicity of phenobarbital, car- havioral toxicity battery was performed whenever pos- bamazepine, phenytoin, and primidone in a double-blind sible prior to administration of any antiepileptic drug and prospective study design. A total of 622 patients, either at 1, 3, 6, and 12 months after initiation of monotherapy. previously untreated or undertreated, were entered into Significant differences in performance on all subtests of the study. Strict exclusion criteria limited confounding the battery were found between patients with epilepsy factors such as drug or alcohol abuse. Results showed and a control group matched by age, sex, and education. that each of the four drugs used as monotherapy were When the differential effects of all four drugs on behav- similarly effective in the treatment of generalized tonic- ioral toxicity were compared, few statistically significant clonic seizures, but carbamazepine was significantly differences emerged. -

2015 ACVIM Small Animal Consensus Statement on Seizure Management in Dogs
2015 ACVIM Small Animal Consensus Statement on seizure management in dogs Podell, M.; Volk, H. A.; Berendt, Mette; Löscher, W.; Muñana, K.; Patterson, E. E.; Platt, S. R. Published in: Journal of Veterinary Internal Medicine DOI: 10.1111/jvim.13841 Publication date: 2016 Document version Publisher's PDF, also known as Version of record Document license: CC BY-NC Citation for published version (APA): Podell, M., Volk, H. A., Berendt, M., Löscher, W., Muñana, K., Patterson, E. E., & Platt, S. R. (2016). 2015 ACVIM Small Animal Consensus Statement on seizure management in dogs. Journal of Veterinary Internal Medicine, 30(2), 477-490. https://doi.org/10.1111/jvim.13841 Download date: 28. Sep. 2021 ACVIM Consensus Statement J Vet Intern Med 2016;30:477–490 Consensus Statements of the American College of Veterinary Internal Medicine (ACVIM) provide the veterinary community with up-to-date information on the pathophysiology, diagnosis, and treatment of clinically important animal diseases. The ACVIM Board of Regents oversees selection of relevant topics, identification of panel members with the expertise to draft the statements, and other aspects of assuring the integrity of the process. The statements are derived from evidence-based medicine whenever possible and the panel offers interpretive comments when such evidence is inadequate or contradictory. A draft is prepared by the panel, followed by solicitation of input by the ACVIM membership which may be incor- porated into the statement. It is then submitted to the Journal of Veterinary Internal Medicine, where it is edited before publication. The authors are solely responsible for the content of the statements. -

5 Clinical Pearls for Contraception and Preconception Counseling
EDITORIAL Women with epilepsy: 5 clinical pearls for contraception and preconception counseling For women with epilepsy, intrauterine devices are the optimal reversible contraceptive, and, preconception, the use of antiepileptic drugs with the lowest teratogenic potential should be considered Robert L. Barbieri, MD Editor in Chief, OBG MANAGEMENT Chair, Obstetrics and Gynecology Brigham and Women’s Hospital, Boston, Massachusetts Kate Macy Ladd Professor of Obstetrics, Gynecology and Reproductive Biology Harvard Medical School, Boston n 2015, 1.2% of the US population bazepine (Aptiom), felbamate (Fel- becoming pregnant while taking the was estimated to have active epi- batol), oxcarbazepine (Trileptal), oral contraceptive.6 Carbamazepine, Ilepsy.1 For neurologists, key goals perampanel (Fycompa), phenobarbi- a strong inducer of hepatic enzymes, in the treatment of epilepsy include: tal, phenytoin (Dilantin), primidone was the most frequently used AED in controlling seizures, minimizing (Mysoline), rufinamide (Banzel), this sample. adverse effects of antiepileptic drugs and topiramate (Topamax) (at dos- Many studies report that carba- (AEDs) and optimizing quality of ages >200 mg daily). According to mazepine accelerates the metabo- life. For obstetrician-gynecologists, Lexicomp, the following AEDs do not lisms of estrogen and progestins and women with epilepsy (WWE) have cause clinically significant changes reduces contraceptive efficacy. For unique contraceptive, preconcep- in hepatic enzymes that metabolize example, in one study 20 healthy tion, and obstetric needs that require steroid hormones: acetazolamide women were administered an ethi- highly specialized approaches to (Diamox), clonazepam (Klonopin), nyl estradiol (20 µg)-levonorgestrel care. Here, I highlight 5 care points ethosuximide (Zarontin), gabapentin (100 µg) contraceptive, and randomly that are important to keep in mind (Neurontin), lacosamide (Vimpat), assigned to either receive carbamaze- when counseling WWE. -

2015 ACVIM Small Animal Consensus Statement on Seizure Management in Dogs
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Copenhagen University Research Information System 2015 ACVIM Small Animal Consensus Statement on seizure management in dogs Podell, M.; Volk, H. A.; Berendt, Mette; Löscher, W.; Muñana, K.; Patterson, E. E.; Platt, S. R. Published in: Journal of Veterinary Internal Medicine DOI: 10.1111/jvim.13841 Publication date: 2016 Document version Publisher's PDF, also known as Version of record Document license: CC BY-NC Citation for published version (APA): Podell, M., Volk, H. A., Berendt, M., Löscher, W., Muñana, K., Patterson, E. E., & Platt, S. R. (2016). 2015 ACVIM Small Animal Consensus Statement on seizure management in dogs. Journal of Veterinary Internal Medicine, 30(2), 477-490. https://doi.org/10.1111/jvim.13841 Download date: 08. Apr. 2020 ACVIM Consensus Statement J Vet Intern Med 2016;30:477–490 Consensus Statements of the American College of Veterinary Internal Medicine (ACVIM) provide the veterinary community with up-to-date information on the pathophysiology, diagnosis, and treatment of clinically important animal diseases. The ACVIM Board of Regents oversees selection of relevant topics, identification of panel members with the expertise to draft the statements, and other aspects of assuring the integrity of the process. The statements are derived from evidence-based medicine whenever possible and the panel offers interpretive comments when such evidence is inadequate or contradictory. A draft is prepared by the panel, followed by solicitation of input by the ACVIM membership which may be incor- porated into the statement. It is then submitted to the Journal of Veterinary Internal Medicine, where it is edited before publication. -
![APTIOM (Eslicarbazepine Acetate) Is (S)-10-Acetoxy-10,11-Dihydro-5H Dibenz[B,F]Azepine-5-Carboxamide](https://docslib.b-cdn.net/cover/5440/aptiom-eslicarbazepine-acetate-is-s-10-acetoxy-10-11-dihydro-5h%C2%AD-dibenz-b-f-azepine-5-carboxamide-1265440.webp)
APTIOM (Eslicarbazepine Acetate) Is (S)-10-Acetoxy-10,11-Dihydro-5H Dibenz[B,F]Azepine-5-Carboxamide
HIGHLIGHTS OF PRESCRIBING INFORMATION Monitor and discontinue if another cause cannot be established. (5.2, 5.3, These highlights do not include all the information needed to use 5.4) APTIOM safely and effectively. See full prescribing information for • Hyponatremia: Monitor sodium levels in patients at risk or patients APTIOM. experiencing hyponatremia symptoms. (5.5) • Neurological Adverse Reactions: Monitor for dizziness, disturbance in gait APTIOM® (eslicarbazepine acetate) tablets, for oral use and coordination, somnolence, fatigue, cognitive dysfunction, and visual Initial U.S. Approval: 2013 changes. Use caution when driving or operating machinery. (5.6) • Withdrawal of APTIOM: Withdraw APTIOM gradually to minimize the ---------------------------RECENT MAJOR CHANGES------------------------- risk of increased seizure frequency and status epilepticus. (2.6, 5.7, 8.1) Indications and Usage (1) 9/2017 • Dosage and Administration (2) 9/2017 Drug Induced Liver Injury: Discontinue APTIOM in patients with jaundice Warnings and Precautions (5) 9/2017 or evidence of significant liver injury. (5.8) • Hematologic Adverse Reactions: Consider discontinuing. (5.10) ----------------------------INDICATIONS AND USAGE-------------------------- APTIOM is indicated for the treatment of partial-onset seizures in patients 4 ------------------------------ADVERSE REACTIONS------------------------------ years of age and older. (1) • Most common adverse reactions in adult patients receiving APTIOM (≥4% and ≥2% greater than placebo): dizziness, somnolence, nausea, headache, ----------------------DOSAGE AND ADMINISTRATION---------------------- diplopia, vomiting, fatigue, vertigo, ataxia, blurred vision, and tremor. (6.1) • Adult Patients: The recommended initial dosage of APTIOM is 400 mg • Adverse reactions in pediatric patients are similar to those seen in adult once daily. For some patients, treatment may be initiated at 800 mg once patients. daily if the need for seizure reduction outweighs an increased risk of adverse reactions. -
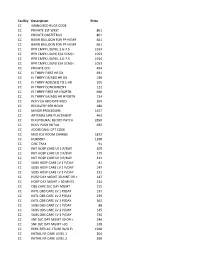
NMMC West Point CDM.Xlsx
Facility Description Price CC SWING BED RUGS CODE CC PRIVATE 1ST WEST 861 CC PRIVATE OBSTETRICS 861 CC BAKRI BALLOON FOR PP HEMR 661 CC BAKRI BALLOON FOR PP HEMR 661 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC PRIVATE ECU 494 CC IV THRPY FIRST HR DX 691 CC IV THRPY EA/ADD HR DX 190 CC IV THRPY ADD/SEQ TO 1 HR 205 CC IV THRPY CONCURRENT 122 CC IV THRPY FIRST HR HYDRTN 690 CC IV THRPY EA/ADD HR HYDRTN 134 CC INJ IV EA ADD DIFF MED 269 CC RECOVERY PER HOUR 280 CC MINOR PROCEDURE 1627 CC ARTERIAL LINE PLACEMENT 463 CC INJ EPIDURAL BLOOD PATCH 2850 CC INJ IV PUSH INITIAL 692 CC ADDITIONAL CPT CODE CC MED ICU ROOM CHARGE 1872 CC NURSERY 1200 CC CIRC TRAY 91 CC INIT HOSP CARE LV 1 P/DAY 205 CC INIT HOSP CARE LV 2 P/DAY 279 CC INIT HOSP CARE LV 3 P/DAY 412 CC SUBS HOSP CARE LV 1 P/DAY 81 CC SUBS HOSP CARE LV 2 P/DAY 147 CC SUBS HOSP CARE LV 3 P/DAY 212 CC HOSP DAY MGMT 30 MNT OR < 147 CC HOSP DAY MGMT > 30 MNTS 214 CC OBS CARE D/C DAY MGMT 155 CC INITL OBS CARE LV 1 P/DAY 197 CC INITL OBS CARE LV 2 P/DAY 239 CC INITL OBS CARE LV 3 P/DAY 362 CC SUBS OBS CARE LV 1 P/DAY 88 CC SUBS OBS CARE LV 2 P/DAY 145 CC SUBS OBS CARE LV 3 P/DAY 236 CC SNF D/C DAY MGMT 30 OR < 240 CC SNF D/C DAY MGMT >30 318 CC PERC REPLAC J TUBE W/O FL 1948 CC INITIAL NF CARE LEVEL 1 204 CC INITIAL NF CARE LEVEL 2 290 CC INITIAL NF CARE LEVEL 3 368 CC SUBSQENT NF CARE LEVEL 197 CC SUBSQENT NF CARE LEVEL 2 151 CC SUBSQENT NF CARE LEVEL 3 198 CC SUBSQENT NF CARE LEVEL 4 295 CC OBS OR I/P -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine