Statement on Unassisted Birth Attended by a Doula
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of a Midwife in Assisted Reproductive Units
Clinical Obstetrics, Gynecology and Reproductive Medicine Research Article ISSN: 2059-4828 The role of a midwife in assisted reproductive units O Tsonis1, F Gkrozou2*, V Siafaka3 and M Paschopoulos1 1Department of Obstetrics and Gynaecology, University Hospital of Ioannina, Greece 2Department of Obstetrics and Gynaecology, university Hospitals of Birmingham, UK 3Department of Speech and Language Therapy, School of Health Sciences, University of Ioannina, Greece Abstract Problem: The role of midwifery in Assisted Reproductive Units remains unclear. Background: Midwives are valuable health workers in every field or phase of women’s health. Their true value has been consistently demonstrated and regards mainly their function in labour. Infertility is a quite new territory in which a great deal of innovating approaches has been made through the years. Aim: The aim of this study is to present the role of midwifery in Assisted Reproductive Units based on scientific data Methods: For this review 3 (three) major search engines were included MEDLINE, PubMed and EMBASE focusing on the role of midwives in the assisted reproductive units. Findings: It seems that midwives have three distinct roles, when it comes to emotional management of the infertile couple, being the representative of the infertile couple and also, performing assisted reproductive techniques in some cases. Their psychomedical support is profound and, in this review, we try to research their potential role in the assisted reproductive units. Discussion: In the literature, only few scientific articles have been conducted in search of the role of Midwifery in Infertility. Their importance is once again undeniable and further research needs to be conducted in order to increase their adequate participation into this medical field. -

The Birth Sisters Program: a Model of Hospital-Based Doula Support to Promote Health Equity
The Birth Sisters Program: A Model of Hospital-Based Doula Support to Promote Health Equity Julie Mottl-Santiago, Kirsten Herr, Dona Rodrigues, Catherine Walker, Catherine Walker, Emily Feinberg Journal of Health Care for the Poor and Underserved, Volume 31, Number 1, February 2020, pp. 43-55 (Article) Published by Johns Hopkins University Press DOI: https://doi.org/10.1353/hpu.2020.0007 For additional information about this article https://muse.jhu.edu/article/747773 Access provided at 19 Feb 2020 19:43 GMT from University of California, Davis REPORT FROM THE FIELD Th e Birth Sisters Program: A Model of Hospital- Based Doula Support to Promote Health Equity Julie Mottl- Santiago, MPH, CNM Kirsten Herr, BA Dona Rodrigues, MPH, CNM Catherine Walker, MPH, CNM Emily Feinberg, ScD, CPNP Summary: Maternity care in the United States is characterized by racial and income disparities in maternal and infant outcomes. Th is article describes an innovative, hospital- based doula model serving a racially and ethnically diverse, low-income population. Th e program’s his- tory, program model, administration requirements, training, and evaluations are described. Key words: Doula, community health worker, maternal- child health services, low-income populations, obstetrics. acial and income disparities in maternity care outcomes in the United States are Rlarge and persistent. Non- Hispanic Black people and Hispanic people have higher rates of preterm birth,1,2 lower rates of engagement with prenatal care,3 lower rates of breastfeeding,4,5 and higher rates -

Experiences of Transition to Motherhood Among Pregnant Women Following Assisted Reproductive Technology: a Systematic Review Protocol of Qualitative Evidence
SYSTEMATIC REVIEW PROTOCOL Experiences of transition to motherhood among pregnant women following assisted reproductive technology: a systematic review protocol of qualitative evidence 1,2 1,2 1,2 1,2 1,2 Kunie Maehara Hiroko Iwata Mai Kosaka Kayoko Kimura Emi Mori 1Graduate School of Nursing, Chiba University, Chiba, Japan, 2The Chiba University Centre for Evidence Based Practice: a Joanna Briggs Institute Affiliated Group ABSTRACT Objective: This systematic review aims to identify and synthesize available qualitative evidence related to the experiences of transition to motherhood during pregnancy in women who conceived through assisted reproductive technology (ART). Introduction: Women who conceived through ART experience pregnancy-specific anxiety and paradoxical feelings, and face unique challenges in their identity transition to motherhood. It is important for healthcare professionals working with these women to understand the context and complexity of this special path to parenthood, including the emotional adaptation to pregnancy following ART. A qualitative systematic review can provide the best available evidence to inform development of nursing interventions to meet the needs of pregnant women after ART. Inclusion criteria: This review will consider any qualitative research data from empirical studies published from 1992–2019 in English or Japanese that described experiences of transition to motherhood during pregnancy in women who conceived with ART. Methods: This review will follow the JBI approach for qualitative systematic reviews. Databases that will be searched for published and unpublished studies include MEDLINE, CINAHL, PsycINFO, ProQuest Health & Medical Collection, Google Scholar and Open Access Theses and Dissertations (in English), and Ichushi-Web, CiNii and the Institutional Repositories Database (in Japanese). -

Impact of Whole Systems Traditional Chinese Medicine on in Vitro Fertilization Outcomes
HHS Public Access Author manuscript Author Manuscript Author ManuscriptReprod Author ManuscriptBiomed Online. Author Manuscript Author manuscript; available in PMC 2016 June 01. Published in final edited form as: Reprod Biomed Online. 2015 June ; 30(6): 602–612. doi:10.1016/j.rbmo.2015.02.005. Impact of Whole Systems Traditional Chinese Medicine on In Vitro Fertilization Outcomes Lee E. Hullender Rubina, Michael S. Opsahlb, Klaus Wiemerb, Scott D. Mistc, and Aaron B. Caugheyc aOregon College of Oriental Medicine, Oregon Health and Science University, 75 NW Couch St, Portland Oregon, 97210, USA bNorthwest Center for Reproductive Sciences, Kirkland, Washington; Poma Fertility, Kirkland, Washingon, USA cOregon Health and Science University, Portland, Oregon, USA Abstract Patients undergoing IVF patients may receive either acupuncture or whole-systems traditional Chinese medicine (WS-TCM) as an adjuvant IVF treatment. WS-TCM is a complex intervention that can include acupuncture, Chinese herbal medicine, dietary, lifestyle recommendations, or both. In this retrospective cohort study, 1231 IVF patient records were reviewed to assess the effect of adjuvant WS-TCM on IVF outcomes compared among three groups: IVF with no additional treatment; IVF and elective acupuncture on day of embryo transfer; or IVF and elective WS-TCM. The primary outcome was live birth. Of 1069 non-donor cycles, WS-TCM was associated with greater odds of live birth compared with IVF alone (adjusted odds ratio [AOR] 2.09; 95% confidence interval [CI] 1.36 to 3.21), or embryo transfer with acupuncture only (AOR 1.62; 95% CI 1.04 to 2.52). Of 162 donor cycles, WS-TCM was associated with increased live births compared with all groups (odds Ratio [OR] 3.72; 95% CI 1.05 to 13.24, unadjusted] or embryo transfer with acupuncture only (OR 4.09; 95% CI: 1.02 to 16.38, unadjusted). -

The Factors Affecting Amniocentesis Decision by Pregnant Women in the Risk Group and the Influence of Consultant
A L J O A T U N R I N R A E L P Original Article P L E R A Perinatal Journal 2019;27(1):6–13 I N N R A U T A L J O ©2019 Perinatal Medicine Foundation The factors affecting amniocentesis decision by pregnant women in the risk group and the influence of consultant Kanay Yararbafl1 İD , Ayflegül Kuflkucu2 İD 1Department of Medical Genetics, Faculty of Medicine, Ac›badem Mehmet Ali Ayd›nlar University, Istanbul, Turkey 2Department of Medical Genetics, Faculty of Medicine, Yeditepe University, Istanbul, Turkey Abstract Özet: Risk grubundaki gebelerin amniyosentez karar› almas›ndaki faktörler ve genetik dan›flman›n etkisi Objective: The most frequent goal for prenatal diagnosis is to Amaç: Do¤um öncesi tan›da günümüzde en s›k amaçlanan hedef detect pregnancies with Down syndrome. Since karyotyping, which Down sendromlu gebelikleri tespit etmektir. Tan›da alt›n standart is the golden standard for the diagnosis, has not been replaced with yöntem olan karyotiplemenin yerini henüz non-invaziv bir yön- a non-invasive method, pregnant women in the risk group should tem dolduramad›¤›ndan, CVS, amniyosentez gibi bir yöntem için choose the method such as CVS and amniocentesis. Therefore, risk alt›ndaki gebelerin seçimi gereklidir. Bu amaçla giriflimsel ol- screening tests are performed by non-invasive method, and preg- mayan yöntemlerle tarama testleri yap›lmakta, riskli gebelere ge- nant women under risk are provided genetic consultation and the netik dan›flma verilerek invaziv giriflim karar› aileye b›rak›lmakta- family is expected to make a decision for invasive procedure. -

Report Title: Celebrating Birth – Aboriginal Midwifery in Canada
Report title: Celebrating Birth – Aboriginal Midwifery in Canada © Copyright 2008 National Aboriginal Health Organization ISBN: 978-1-926543-11-6 Date Published: December 2008 OAAPH [now known as the National Aboriginal Health Organization (NAHO)] receives funding from Health Canada to assist it to undertake knowledge-based activities including education, research and dissemination of information to promote health issues affecting Aboriginal persons. However, the contents and conclusions of this report are solely that of the authors and not attributable in whole or in part to Health Canada. The National Aboriginal Health Organization, an Aboriginal-designed and -controlled body, will influence and advance the health and well-being of Aboriginal Peoples by carrying out knowledge-based strategies. This report should be cited as: National Aboriginal Health Organization. 2008. Celebrating Birth – Aboriginal Midwifery in Canada. Ottawa: National Aboriginal Health Organization. For queries or copyright requests, please contact: National Aboriginal Health Organization 220 Laurier Avenue West, Suite 1200 Ottawa, ON K1P 5Z9 Tel: (613) 237-9462 Toll-free: 1-877-602-4445 Fax: (613) 237-1810 E-mail: [email protected] Website: www.naho.ca Under the Canadian Constitution Act, 1982, the term Aboriginal Peoples refers to First Nations, Inuit and Métis people living in Canada. However, common use of the term is not always inclusive of all three distinct people and much of the available research only focuses on particular segments of the Aboriginal population. NAHO makes every effort to ensure the term is used appropriately. Acknowledgements The original Midwifery and Aboriginal Midwifery in Canada paper was published by the National Aboriginal Health Organization (NAHO) in May 2004. -

Virginia Commonwealth University Volunteer Doula Program Training Manual Kathleen M
Virginia Commonwealth University VCU Scholars Compass School of Nursing Publications School of Nursing 2015 Virginia Commonwealth University Volunteer Doula Program Training Manual Kathleen M. Bell Virginia Commonwealth University, [email protected] Susan L. Linder Virginia Commonwealth University, [email protected] Follow this and additional works at: http://scholarscompass.vcu.edu/nursing_pubs Part of the Maternal, Child Health and Neonatal Nursing Commons Copyright © 2015 The Authors Downloaded from http://scholarscompass.vcu.edu/nursing_pubs/16 This Curriculum Material is brought to you for free and open access by the School of Nursing at VCU Scholars Compass. It has been accepted for inclusion in School of Nursing Publications by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. Virginia Commonwealth University Volunteer Doula Program Training Manual “Empowerment, advocacy and support for one of life’s greatest journeys.” 1 Reflection and Discussion Why are you here? Why did you decide to do this doula training? What experiences do you have with birth, and how have they shaped your desire to participate in this program? What does it mean to be a doula with the VCU School of Nursing? What other reflections do you have? 2 Table of Contents 1. An overview of birth: Statistics and trends………………page 4-6 2. Birth workers and their roles………………...……………pages 7-10 3. You are a doula! Your birth-bag and preparation………..pages 11-14 4. Anatomy and Physiology of birth………………………...pages 15-18 5. Hormonal regulation of labor and birth…………………..pages 19-21 6. Pharmacologic management of labor…………………….pages 22-26 7. -

Nurses and Doulas: Complementary Roles to Provide Optimal Maternity Care Lois Eve Ballen and Ann J
CLINICAL ISSUES Nurses and Doulas: Complementary Roles to Provide Optimal Maternity Care Lois Eve Ballen and Ann J . Fulcher Staff in maternity-care facilities are seeing an doulas and hospital staff. The purpose of this article increase in doulas, nonmedical childbirth assistants, is to clarify the positive effects of doula support in who are trained to provide continuous physical, emo- labor, clarify some misconceptions about the doula ’ s tional, and informational labor support. The long- role, and discuss ways that nurses and doulas can term medical and psychosocial benefi ts are well work effectively together. documented. In this article, misconceptions about the doula ’ s role are corrected, and suggestions are of- Benefi ts of Continuous Labor Support fered on ways to improve communication between health care providers and doulas. Together, nurses A growing and unambiguous body of literature and doulas can provide birthing women with a safe demonstrates medical benefi ts and an increase in pa- and satisfying birth. JOGNN, 35, 304-311; 2006. tient satisfaction with continuous labor support to DOI: 10.1111/J.1552-6909.2006.00041.x both mother and infant and the cost savings to be Keywords: Birth outcomes — Childbirth — gained by the use of doulas ( Abramson, Altfeld, & Complementary roles — confl ict — Doula — Evidenced- Teibloom-Mishkin, 2000; Hodnett, Gates, Hofmeyr, based practice — Labor support & Sakala, 2003; Sauls, 2002 ). The Cochrane Library published an updated systematic review on continuous Accepted: October 2005 labor support in 2003, concluding “ Women who had continuous intrapartum support were less likely to To the relief of some busy nurses, and the conster- have intrapartum analgesia, operative birth or to re- nation of others, trained childbirth assistants called port dissatisfaction with their childbirth experiences. -

Midwifery: a Career for Men in Nursing
Midwifery: A career for men in nursing It may not be a common path men take, but how many male midwives are there? By Deanna Pilkenton, RN, CNM, MSN, and Mavis N. Schorn, RN, CNM, PHD(C) Every year, faculty at Vanderbilt University School of there are so few men in this profession. In fact, these Nursing reviews applications to the school’s nurse- conversations often lead to the unanimous sentiment midwifery program. The applicants’ diversity is always that men shouldn’t be in this specialty at all. Scanning of interest. A wide spectrum of age is common. A pleas- the web and reviewing blog discussions on this topic ant surprise has been the gradual improvement in the confirms that it’s a controversial idea, even among Eethnic and racial diversity of applicants. Nevertheless, midwives themselves. male applicants are still rare. It’s common knowledge that the profession of nurs- Many people wonder if there’s such thing as a male ing is female dominated, and the challenges and com- midwife. There are male midwives; there just aren’t plexities of this have been explored at length. many of them. When the subject of men in midwifery is Midwifery, however, may be one of the most exclusive- discussed, it usually conjures up perplexed looks. The ly and disproportionately female specialties in the field very idea of men in midwifery can create quite a stir, of nursing and it’s time to acknowledge the presence of and most laypeople don’t perceive it as strange that male midwives, the challenges they face, and the posi- www.meninnursingjournal.com February 2008 l Men in Nursing 29 tive attributes they bring to the pro- 1697, is credited with innovations fession. -
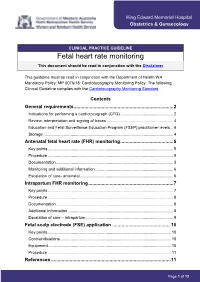
Fetal Heart Rate Monitoring This Document Should Be Read in Conjunction with the Disclaimer
King Edward Memorial Hospital Obstetrics & Gynaecology CLINICAL PRACTICE GUIDELINE Fetal heart rate monitoring This document should be read in conjunction with the Disclaimer This guideline must be read in conjunction with the Department of Health WA Mandatory Policy: MP 0076/18: Cardiotocography Monitoring Policy. The following Clinical Guideline complies with the Cardiotocography Monitoring Standard. Contents General requirements ........................................................................... 2 Indications for performing a cardiotocograph (CTG) ............................................... 2 Review, interpretation and signing of traces ........................................................... 4 Education and Fetal Surveillance Education Program (FSEP) practitioner levels ... 4 Storage ................................................................................................................... 4 Antenatal fetal heart rate (FHR) monitoring ........................................ 5 Key points ............................................................................................................... 5 Procedure ............................................................................................................... 5 Documentation ........................................................................................................ 5 Monitoring and additional information ..................................................................... 6 Escalation of care- antenatal .................................................................................. -

The Law of Placenta
The Law of Placenta Mathilde Cohent ABSTRACT: Of the forms of reproductive labor in which legal scholars have been interested, placenta, the organ developed during pregnancy, has been overlooked. As placenta becomes an object of value for a growing number of individuals, researchers, clinicians, biobanks, and biotech companies, among others, its cultural meaning is changing. At the same time, these various constituencies may be at odds. Some postpartum parents and their families want to repossess their placenta for personal use, while third parties use placentas for a variety of research, medical, and commercial purposes. This Article contributes to the scholarship on reproductive justice and agency by asking who should have access to placentas and under what conditions. The Article emphasizes the insufficient protection the law affords pregnant people wishing to decide what happens to their placenta. Generally considered clinical waste under federal and state law, placental tissue is sometimes made inaccessible to its producers on the ground that it is infectious at the same time as it is made available to third parties on the ground that placenta is discarded and de-identified tissue. Less privileged people who lack the ability to shop for obstetric and other pregnancy-related services that allow them to keep their placentas are at a disadvantage in this chain of supply and demand. While calling for further research on the modus operandi of placenta markets and how pregnant people think about them, this Article concludes that lawmakers should take steps to protect decision-making autonomy over placental labor and offers a range of proposals to operationalize this idea. -

Birthing Outside the System: Trauma and Autonomy in Maternity Care
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/201204 Please be advised that this information was generated on 2021-10-07 and may be subject to change. Birthing outside the system: system: the Birthing outside Uitnodiging voor het bijwonen van de openbare verdediging van mijn proefschrift Birthing outside the system: trauma and autonomy in maternity care op dinsdag 19 maart 2019 om 14:30 uur in de Aula van de Radboud Universiteit trauma and autonomy in maternity care in maternity autonomy and trauma Comeniuslaan 2, Nijmegen. U bent van harte welkom bij deze plechtigheid en de aansluitende receptie. Martine Hollander [email protected] | Martine Helene Hollander Martine Helene Birthing outside the system: trauma and autonomy in maternity care Paranimfen Lianne Holten [email protected] Martine Helene Hollander Claire Stramrood [email protected] Birthing outside the system: trauma and autonomy in maternity care Martine Helene Hollander 528107-L-sub01-bw-Hollander Processed on: 23-1-2019 PDF page: 1 ISBN 978-94-028-1373-9 Design/lay-out Promotie In Zicht, Arnhem Print Ipskamp Printing, Enschede © M.H. Hollander, 2019 All rights are reserved. No part of this book may be reproduced, distributed, stored in a retrieval system, or transmitted in any form or by any means, without prior written permission of the author. 528107-L-sub01-bw-Hollander Processed on: 23-1-2019 PDF page: 2 Birthing outside the system: trauma and autonomy in maternity care Proefschrift ter verkrijging van de graad van doctor aan de Radboud Universiteit Nijmegen op gezag van de rector magnificus prof.