Description, Definition and Diagnosis of Common Skin Rashes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Use of Biologic Agents in the Treatment of Oral Lesions Due to Pemphigus and Behçet's Disease: a Systematic Review
Davis GE, Sarandev G, Vaughan AT, Al-Eryani K, Enciso R. The Use of Biologic Agents in the Treatment of Oral Lesions due to Pemphigus and Behçet’s Disease: A Systematic Review. J Anesthesiol & Pain Therapy. 2020;1(1):14-23 Systematic Review Open Access The Use of Biologic Agents in the Treatment of Oral Lesions due to Pemphigus and Behçet’s Disease: A Systematic Review Gerald E. Davis II1,2, George Sarandev1, Alexander T. Vaughan1, Kamal Al-Eryani3, Reyes Enciso4* 1Advanced graduate, Master of Science Program in Orofacial Pain and Oral Medicine, Herman Ostrow School of Dentistry of USC, Los Angeles, California, USA 2Assistant Dean of Academic Affairs, Assistant Professor, Restorative Dentistry, Meharry Medical College, School of Dentistry, Nashville, Tennessee, USA 3Assistant Professor of Clinical Dentistry, Division of Periodontology, Dental Hygiene & Diagnostic Sciences, Herman Ostrow School of Dentistry of USC, Los Angeles, California, USA 4Associate Professor (Instructional), Division of Dental Public Health and Pediatric Dentistry, Herman Ostrow School of Dentistry of USC, Los Angeles, California, USA Article Info Abstract Article Notes Background: Current treatments for pemphigus and Behçet’s disease, such Received: : March 11, 2019 as corticosteroids, have long-term serious adverse effects. Accepted: : April 29, 2020 Objective: The objective of this systematic review was to evaluate the *Correspondence: efficacy of biologic agents (biopharmaceuticals manufactured via a biological *Dr. Reyes Enciso, Associate Professor (Instructional), Division source) on the treatment of intraoral lesions associated with pemphigus and of Dental Public Health and Pediatric Dentistry, Herman Ostrow Behçet’s disease compared to glucocorticoids or placebo. School of Dentistry of USC, Los Angeles, California, USA; Email: [email protected]. -

General Pathomorpholog.Pdf
Ukrаiniаn Medicаl Stomаtologicаl Аcаdemy THE DEPАRTАMENT OF PАTHOLOGICАL АNАTOMY WITH SECTIONSL COURSE MАNUАL for the foreign students GENERАL PАTHOMORPHOLOGY Poltаvа-2020 УДК:616-091(075.8) ББК:52.5я73 COMPILERS: PROFESSOR I. STАRCHENKO ASSOCIATIVE PROFESSOR O. PRYLUTSKYI АSSISTАNT A. ZADVORNOVA ASSISTANT D. NIKOLENKO Рекомендовано Вченою радою Української медичної стоматологічної академії як навчальний посібник для іноземних студентів – здобувачів вищої освіти ступеня магістра, які навчаються за спеціальністю 221 «Стоматологія» у закладах вищої освіти МОЗ України (протокол №8 від 11.03.2020р) Reviewers Romanuk A. - MD, Professor, Head of the Department of Pathological Anatomy, Sumy State University. Sitnikova V. - MD, Professor of Department of Normal and Pathological Clinical Anatomy Odessa National Medical University. Yeroshenko G. - MD, Professor, Department of Histology, Cytology and Embryology Ukrainian Medical Dental Academy. A teaching manual in English, developed at the Department of Pathological Anatomy with a section course UMSA by Professor Starchenko II, Associative Professor Prylutsky OK, Assistant Zadvornova AP, Assistant Nikolenko DE. The manual presents the content and basic questions of the topic, practical skills in sufficient volume for each class to be mastered by students, algorithms for describing macro- and micropreparations, situational tasks. The formulation of tests, their number and variable level of difficulty, sufficient volume for each topic allows to recommend them as preparation for students to take the licensed integrated exam "STEP-1". 2 Contents p. 1 Introduction to pathomorphology. Subject matter and tasks of 5 pathomorphology. Main stages of development of pathomorphology. Methods of pathanatomical diagnostics. Methods of pathomorphological research. 2 Morphological changes of cells as response to stressor and toxic damage 8 (parenchimatouse / intracellular dystrophies). -

FIG. 4A © O O Wo 2015/042110 Al III III II II III III 1 1 II III II II III III II III
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date W O 2015/042110 A l 2 6 March 2015 (26.03.2015) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61P 37/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/US20 14/056021 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, ΓΝ , IR, IS, JP, KE, KG, KN, KP, KR, 17 September 2014 (17.09.2014) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (25) Filing Language: English PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/880,522 20 September 2013 (20.09.2013) (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: CHILDREN'S MEDICAL CENTER COR¬ GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, PORATION [US/US]; 55 Shattuck Street, Boston, Mas¬ TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, sachusetts 021 15 (US). -

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -
Erythema Ab Igne and Use of Laptop Computers
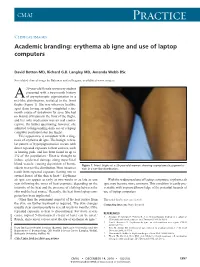
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

Lepromatous Leprosy with Erythema Nodosum Leprosum Presenting As
Lepromatous Leprosy with Erythema Nodosum Leprosum Presenting as Chronic Ulcers with Vasculitis: A Case Report and Discussion Anny Xiao, DO,* Erin Lowe, DO,** Richard Miller, DO, FAOCD*** *Traditional Rotating Intern, PGY-1, Largo Medical Center, Largo, FL **Dermatology Resident, PGY-2, Largo Medical Center, Largo, FL ***Program Director, Dermatology Residency, Largo Medical Center, Largo, FL Disclosures: None Correspondence: Anny Xiao, DO; Largo Medical Center, Graduate Medical Education, 201 14th St. SW, Largo, FL 33770; 510-684-4190; [email protected] Abstract Leprosy is a rare, chronic, granulomatous infectious disease with cutaneous and neurologic sequelae. It can be a challenging differential diagnosis in dermatology practice due to several overlapping features with rheumatologic disorders. Patients with leprosy can develop reactive states as a result of immune complex-mediated inflammatory processes, leading to the appearance of additional cutaneous lesions that may further complicate the clinical picture. We describe a case of a woman presenting with a long history of a recurrent bullous rash with chronic ulcers, with an evolution of vasculitic diagnoses, who was later determined to have lepromatous leprosy with reactive erythema nodosum leprosum (ENL). Introduction accompanied by an intense bullous purpuric rash on management of sepsis secondary to bacteremia, Leprosy is a slowly progressive disease caused by bilateral arms and face. For these complaints she was with lower-extremity cellulitis as the suspected infection with Mycobacterium leprae (M. leprae). seen in a Complex Medical Dermatology Clinic and source. A skin biopsy was taken from the left thigh, Spread continues at a steady rate in several endemic clinically diagnosed with cutaneous polyarteritis and histopathology showed epidermal ulceration countries, with more than 200,000 new cases nodosa. -

Interstitial Granuloma Annulare Triggered by Lyme Disease
Volume 27 Number 5| May 2021 Dermatology Online Journal || Case Presentation 27(5):11 Interstitial granuloma annulare triggered by Lyme disease Jordan Hyde1 MD, Jose A Plaza1,2 MD, Jessica Kaffenberger1 MD Affiliations: 1Division of Dermatology, The Ohio State University Wexner Medical Center, Columbus, Ohio, USA, 2Department of Pathology, The Ohio State University Wexner Medical Center, Columbus, Ohio, USA Corresponding Author: Jessica Kaffenberger MD, Division of Dermatology, The Ohio State University Medical Wexner Medical Center, Suite 240, 540 Officenter Place, Columbus, OH 43230, Tel: 614-293-1707, Email: [email protected] been associated with a variety of systemic diseases Abstract including diabetes mellitus, malignancy, thyroid Granuloma annulare is a non-infectious disease, dyslipidemia, and infection [3,4]. granulomatous skin condition with multiple different associations. We present a case of a man in his 60s There are multiple histological variants of GA, with a three-week history of progressive targetoid including interstitial GA. The histopathology of plaques on his arms, legs, and trunk. Skin biopsy classic GA demonstrates a focal degeneration of demonstrated interstitial granuloma annulare. collagen surrounded by an inflammatory infiltrate Additional testing revealed IgM antibodies to Borrelia composed of lymphocytes and histiocytes. In a less burgdorferi on western blot suggesting interstitial common variant, interstitial GA, scattered histiocytes granuloma annulare was precipitated by the recent are seen -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

'Spongiosis' Dermatitis With
Spongiosis Spongiosis and Spongiotic • What is ‘spongiosis’? – Intra-epidermal and Dermatitis intercellular edema • Widening of intercellular spaces between keratinocytes • Elongation of G.Peter Sarantopoulos, MD intercellular bridges UCLA Medical Center Spongiosis vs. Spongiotic Spongiosis Dermatitis • ‘Spongiosis’ as a histologic concept (not a • Not everything ‘spongiotic’ is a diagnosis!) spongiotic dermatitis – Intra-epidermal edema accompanies many (if not all) inflammatory skin diseases to some degree • So-called ‘patterns of spongiosis’ • Important to distinguish spongiosis as… – Neutrophilic – The predominant histologic finding – Eosinophilic – A non-specific feature of other inflammatory – Follicular dermatoses (e.g. lichenoid/interface, vasculopathic, – Miliarial psoriasiform, etc) – Sometimes, there is overlap Dermatitis with ‘Spongiosis’ Dermatitis with ‘Spongiosis’ * Neutrophilic: Eosinophilic: Miliarial: Neutrophilic: Eosinophilic: Miliarial: Pustular psoriasis Pemphigus (precursor) M. Crystallina Pustular psoriasis Pemphigus (precursor) M. Crystallina Reiter’s syndrome Pemphigus vegetans M. Rubra Reiter’s syndrome Pemphigus vegetans M. Rubra IgA Pemphigus Bullous pemphigoid M. profunda IgA Pemphigus Bullous pemphigoid M. profunda Pemphigus herpetiformis Cicatricial pemphigoid Pemphigus herpetiformis Cicatricial pemphigoid Infantile acropustulosis Pemphigoid (herpes) Infantile acropustulosis Pemphigoid (herpes) AGEP gestationis Follicular: AGEP gestationis Follicular: Palmoplantar pustulosis Idiopathic eosinophilic Infundibulofolliculitis -

Genital Dermatology
GENITAL DERMATOLOGY BARRY D. GOLDMAN, M.D. 150 Broadway, Suite 1110 NEW YORK, NY 10038 E-MAIL [email protected] INTRODUCTION Genital dermatology encompasses a wide variety of lesions and skin rashes that affect the genital area. Some are found only on the genitals while other usually occur elsewhere and may take on an atypical appearance on the genitals. The genitals are covered by thin skin that is usually moist, hence the dry scaliness associated with skin rashes on other parts of the body may not be present. In addition, genital skin may be more sensitive to cleansers and medications than elsewhere, emphasizing the necessity of taking a good history. The physical examination often requires a thorough skin evaluation to determine the presence or lack of similar lesions on the body which may aid diagnosis. Discussion of genital dermatology can be divided according to morphology or location. This article divides disease entities according to etiology. The clinician must determine whether a genital eruption is related to a sexually transmitted disease, a dermatoses limited to the genitals, or part of a widespread eruption. SEXUALLY TRANSMITTED INFECTIONS AFFECTING THE GENITAL SKIN Genital warts (condyloma) have become widespread. The human papillomavirus (HPV) which causes genital warts can be found on the genitals in at least 10-15% of the population. One study of college students found a prevalence of 44% using polymerase chain reactions on cervical lavages at some point during their enrollment. Most of these infection spontaneously resolved. Only a minority of patients with HPV develop genital warts. Most genital warts are associated with low risk HPV types 6 and 11 which rarely cause cervical cancer. -

Diagnosis, Classification, and Management of Erythema
Arch Dis Child 2000;83:347–352 347 Diagnosis, classification, and management of Arch Dis Child: first published as 10.1136/adc.83.4.347 on 1 October 2000. Downloaded from erythema multiforme and Stevens–Johnson syndrome C Léauté-Labrèze, T Lamireau, D Chawki, J Maleville, A Taïeb Abstract become widely accepted that EM and SJS, as Background—In adults, erythema multi- well as toxic epidermal necrolysis, are all part of forme (EM) is thought to be mainly a single “EM spectrum”. In both EM and SJS, related to herpes infection and Stevens– pathological changes in the earliest skin lesion Johnson syndrome (SJS) to drug reac- consist of the accumulation of mononuclear tions. cells around the superficial dermal blood Aims—To investigate this hypothesis in vessels; epidermal damage is more characteris- children, and to review our experience in tic of EM with keratinocyte necrosis leading to the management of these patients. multilocular intraepidermal blisters.5 In fact, Methods—A retrospective analysis of 77 there is little clinical resemblance between paediatric cases of EM or SJS admitted to typical EM and SJS, and recently some authors the Children’s Hospital in Bordeaux be- have proposed a reconsideration of the “spec- tween 1974 and 1998. trum” concept and a return to the original Results—Thirty five cases, inadequately description.15–17 According to these authors, the documented or misdiagnosed mostly as term EM should be restricted to acrally urticarias or non-EM drug reactions were distributed typical targets or raised oedema- excluded. Among the remaining 42 pa- tous papules. Depending on the presence or tients (14 girls and 28 boys), 22 had EM (11 absence of mucous membrane erosions the EM minor and 11 EM major), 17 had SJS, cases may be classified as EM major or EM 16 and three had isolated mucous membrane minor. -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous,