Medical Aspects of Radiation Incidents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Utilization of MOSFET Dosimeters for Clinical Measurements in Radiology
The Utilization of MOSFET Dosimeters for Clinical Measurements in Radiology David Hintenlang, Ph.D., DABR, FACMP Medical Physics Program Director J. Crayton Pruitt Family Department of Biomedical Engineering J. Crayton Pruitt Family Department of Biomedical Engineering Medical Physics Program Conflict of interest statement: The presenter holds no financial interest in, and has no affiliation or research support from any manufacturer or distributor of MOSFET Dosimetry systems. J. Crayton Pruitt Family Department of Biomedical Engineering Medical Physics Program The MOSFET Dosimeter • Metal oxide silicon field effect transistor • Uniquely packaged to serve as a radiation detector – developed as early as 1974 • Applications – Radiation Therapy Dose Verification – Cosmic dose monitoring on satellites – Radiology • ~ 1998 - present J. Crayton Pruitt Family Department of Biomedical Engineering Medical Physics Program Attractive features • Purely electronic dosimeter • Provides immediate dose feedback • Integrates over short periods of time • Small size and portability • Simultaneous measurements (up to 20) J. Crayton Pruitt Family Department of Biomedical Engineering Medical Physics Program Demonstrated radiology applications – Patient dose monitoring/evaluation • Radiography • Fluoroscopic and interventional procedures • CT • Mammography J. Crayton Pruitt Family Department of Biomedical Engineering Medical Physics Program Principles of operation • Ionizing radiation results in the creation of electron-hole pairs • Holes migrate and build up -
RADIATION EFFECTS and SOURCES What Is Radiation? What Does Radiation Do to Us? Where Does Radiation Come From?
RADIATION EFFECTS and SOURCES What is radiation? What does radiation do to us? Where does radiation come from? United Nations Environment Programme RADIATION EFFECTS and SOURCES What is radiation? What does radiation do to us? Where does radiation come from? United Nations Environment Programme DISCLAIMER This publication is largely based on the findings of the United Nations Scientific Committee on the Effects of Atomic Radiation, a subsidiary body of the United Nations General Assembly and for which the United Nations Environment Pro- gramme provides the secretariat. This publication does not necessarily r epresent the views of the Scientific Committee or of the United Nations Environment Programme. The designations employed and the presentation of the material in this publica- tion do not imply the expression of any opinion whatsoever on the part of the United Nations Environment Programme concerning the legal status of any country, territory, city or area or of its authorities, or concerning delimitation of its frontiers or boundaries. This publication may be reproduced in whole or in part and in any form for educational or non-profit purposes without special permission from the copyright holder, provided acknowledgement of the source is made. The United Nations Environment Programme would appreciate receiving a copy of any publication that uses this publication as a source. No use of this publication may be made for resale or for any other commercial purpose whatsoever without prior permission in writing from the United Nations Environment Programme. The United Nations Environment Programme promotes environmentally sound practices globally and in its own activities. This publication was printed on recycled paper, 100 per cent chlorine free. -

Assessment of Occupational Radiation Exposure from Industrial Radiography Practice
Transactions of the Korean Nuclear Society Virtual spring Meeting May 13 -14, 2021 Assessment of Occupational Radiation Exposure from Industrial Radiography Practice Soja Reuben Joseph and Juyoul Kim* Department of NPP Engineering, KEPCO International Nuclear Graduate School, 658-91 Haemaji-ro, Seosaeng-myeon, Ulju-gun, Ulsan 45014 *Corresponding author: [email protected] 1. Introduction used for industrial gamma radiography applications to inspect materials and structures in the density range of Reports of high radiation-related accidents have been approximately 2.71 g/cm3 through 8.53 g/cm3. The linked with industrial radiography than any other exposure device body is shielded with depleted uranium radiography sub-specialty, mainly due to deviation from (DU) or Tungsten (W) shield is encased within a welded standard operating procedures (SOP) and radiation tubular stainless-steel shell end plates, aluminum, brass, protection practices resulting to workers exposure [1]. tungsten and polyurethane with labels, comprises details Industrial gamma radiography is one of the most of radioactive material and transportation package type commonly used non-destructive testing (NDT) methods among others as shown in Fig. 1 [6]. The authorized that employs a technique of inspecting materials for contents of Sentinel model 880 series source projectors hidden flaws by using high activity sealed radioactive parameters are shown in Table I. source housed in a shielded exposure device (commonly known as source projectors) for used in imaging of weld joints and castings and must be managed safely and securely [2]. The devices are operated manually by spinning the controller unit to project the gamma source outside the shielding, in a projection casing. -

Radiation Shielding Design Assessment and Verification Requirements 17
4. High-risk premises 4.1 General description 4.1.1 Premises are classified as high-risk where the potential for radiation exposure is high and substantial shielding is required to operate within dose limits. 4.1.2 A shielding plan must be prepared for all high-risk premises as detailed in Section 6 of this guideline. Complex shielding plans for high risk premises may require significantly more detail than the minimum requirements listed in Section 6. 4.1.3 There is no requirement that the shielding plan be prepared by a CRE, however, the plan must be assessed by an appropriately accredited CRE to ensure compliance with this guideline. In addition, for all premises classified as high risk, a second CRE who is appropriately accredited must carry out an independent assessment of the shielding plan to verify that the plan is satisfactory for the proposed use and that it is compliant with the requirements of this guideline. The shielding plan must be certified by the second CRE. 4.2 High-risk applications 4.2.1 Premises not classified as low or medium are considered to be high risk. These include: a. radiotherapy using a sealed source or irradiating apparatus greater than 150 kVp, including remote after-loading devices b. positron emission tomography (PET) c. in patient isolation facility for nuclear medicine therapy using unsealed gamma emitting radionuclides d. industrial radiography in fully-or partially-enclosed sites and other industrial, research and non-medical activities using radiation apparatus or using and storing sealed sources (where the activity thresholds for sealed radioactive sources, or aggregation of, are categorised as category 1, 2 or 3 as listed in Appendix A,). -

Non-Medical Industrial Radiography V2
Minnesota Rules, Chapter 4732 X-Ray Revision DRAFT INDUSTRIAL RADIOGRAPHY X-RAY SYSTEMS, 2.0 (03/09/2018) Summary of Changes MDH made a number of changes to the Industrial Radiography rule draft v1.0 based on the industrial focus group’s review and feedback at the March 1, 2018 meeting. Substantive changes to version 1.0 are described below. Subp. 2. Safety device. • Deleted item C Subp. 3. Warning lights and devices. • Revised wording in item B Subp. 5. Shutters. • Deleted “either” and “or a coupling” in item A. • Deleted item B Subp. 7. Safety device evaluation. • Item C (2). inserted “if applicable” Subp. 8. Radiation emission limit. • Deleted this subpart. Subp. 8. Radiation protection survey. (formerly Subp. 10) • Renumbered • Revised first sentence inserting underscored language: A registrant is responsible for performing a radiation protection survey for a permanent installation of an industrial radiography x-ray system that includes all beam directions. • Item A. Deleted “of an industrial radiography x-ray system in a permanent location” Subp. 9. Area survey. (formerly Subp. 11) • Renumbered; no changes Subp. 10. Radiation safety officer; qualifications. (formerly Subp. 12) • Renumbered • Updated internal reference in item A. DRAFT INDUSTRIAL RADIOGRAPHY X - RAY SYSTEMS, 2.0 (03/09/2018) • Revised item B by inserting “to include 40 hours of classroom training in the establishment and maintenance of a radiation safety protection program” • Deleted item C Subp. 11. Alternate qualifications. (formerly Subp. 13) • Renumbered; no changes Subp. 12. Radiation safety officer; authority and duties. (formerly Subp. 14) • Renumbered; no changes Subp. 13. Radiographer requirements. (formerly Subp. -

AFRRI Biodosimetry Worksheet
Armed Forces Radiobiology Research Institute Biodosimetry Worksheet (Medical Record of Radiation Dose, Contamination, and Acute Radiation Sickness Response) Reporting Authority (person(s) creating this page of the report) Last name: First name: Country of origin: Unit: Phone: Fax: Email: Location: Date (yymmdd): Time: Casualty Last name: First name: Rank: Country of origin: Parent unit: Parent unit location: Parent unit phone: Unit e-mail: Unit fax: Casualty location: History of presenting injury (conventional and/or radiation): History of previous radiation exposure: Past medical history (general): Medical countermeasures (e.g., antiemetics, transfusion), specify: Administered (where, when, route): Exposure conditions Date of exposure (yymmdd): Exposure location: Time of exposure: Weather conditions (at time of exposure): Exposure results Describe incident: External exposure overview Contamination overview Body exposure: Total Partial Uncertain External contamination: Yes No Shielding confounder: Yes No Internal contamination: Yes No Contaminated wound: Yes No If wound(s) are radiation contaminated, please provide details here: Biodosimetric assays overview Sampling date, time Estimated time Dose Reference radiation quality yymmdd (time) post-exposure (h) (Gy) and dose rate (Gy/min) Time onset of vomiting: Lymphocyte counts or depletion kinetics: Urine bioassay: Cytogenetic biodosimetry: Other: ARS response category overview (maximum grading 0-4; see pages 4 through 6 for guidance) N: C: G: H: = RC: days after radiation exposure: AFRRI -

Experiment "Gamma Dosimetry and Dose Rate Determination" Instruction for Experiment "Gamma Dosimetry and Dose Rate Determination"
TECHNICAL UNIVERSITY DRESDEN Institute of Power Engineering Training Reactor Reactor Training Course Experiment "Gamma Dosimetry and Dose Rate Determination" Instruction for Experiment "Gamma Dosimetry and Dose Rate Determination" Content: 1 .... Motivation 2..... Theoretical Background 2.1... Properties of Ionising Radiation and Interactions of Gamma Radiation 2.2. Detection of Ionising Radiation 2.3. Quantities and Units of Dosimetry 3..... Procedure of the Experiment 3.1. Commissioning and Calibration of the Dosimeter Thermo FH40G 3.2. Commissioning and Calibration of the Dosimeter Berthold LB 133-1 3.3. Commissioning and Calibration of the Dosimeter STEP RGD 27091 3.4. Setup of the Experiment 3.4.1. Measurement of Dose Rate in Various Distances from the Radiation Source 3.4.2. Measurement of Dose Rate behind Radiation Shielding 3.5. Measurement of Dose Rate at the open Reactor Channel 4..... Evaluation of Measuring Results Figures: Fig. 1: Composition of the attenuation coefficient µ of γ-radiation in lead Fig. 2: Design of an ionisation chamber Fig. 3: Classification and legal limit values of radiation protection areas Fig. 4: Setup of the experiment (issued: January 2019) - 1 - 1. Motivation The experiment aims on familiarising with the methods of calibrating different detectors for determination of the dose and the dose rate. Furthermore, the dose rate and the activity in the vicinity of an enclosed source of ionising radiation (Cs-137) will be determined taking into account the background radiation and the measurement accuracy. Additionally, the experiment focuses on the determination of the dose rate of a shielded source as well as on the calculation of the required thickness of the shielding protection layer for meeting the permissible maximum dose rate. -
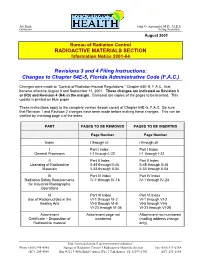
RADIOACTIVE MATERIALS SECTION Revisions 3 and 4 Filing Instructions
Jeb Bush John O. Agwunobi, M.D., M.B.A Governor Acting Secretary August 2001 Bureau of Radiation Control RADIOACTIVE MATERIALS SECTION Information Notice 2001-04 Revisions 3 and 4 Filing Instructions: Changes to Chapter 64E-5, Florida Administrative Code (F.A.C.) Changes were made to “Control of Radiation Hazard Regu lations,” Chapter 64E-5, F.A.C., that became effective August 8 and September 11, 2001. These changes are indicated as Revision 3 or (R3) and Revision 4 (R4) in the margin. Enclosed are copies of the pages to be inserted. This update is printed on blue paper. These instructions apply to the complete version (brown cover) of Chapter 64E -5, F.A.C. Be sure that Revision 1 and Revision 2 changes have been made before making these changes. This can be verified by checking page ii of the index. PART PAGES TO BE REMOVED PAGES TO BE INSERTED Page Number Page Number Index i through xii i through xii I Part I Index Part I Index General Provisions I-1 through I-22 I-1 through I-22 II Part II Index Part II Index Licensing of Radioactive II-45 through II-46 II-45 through II-46 Materials II-53 through II-54 II-53 through II-54 IV Part IV Index Part IV Index Radiation Safety Requirements IV-1 through IV-16 IV-1 through IV-24 for Industrial Radiographic Operations VI Part VI Index Part VI Index Use of Radionuclides in the VI-1 through VI-2 VI-1 through VI-2 Healing Arts VI-5 through VI-6 VI-5 through VI-6 VI-23 through VI-26 VI-23 through VI-26 Attachment Attachment page not Attachment not numbered Certificate – Disposition of numbered (mailing -

Digital Radiation Monitor Is a Health and Safety Instrument That Measures Alpha, Digital Radiation Monitor Beta, and Gamma Radiation
1 Introduction The Digital Radiation Monitor is a health and safety instrument that measures alpha, Digital Radiation Monitor beta, and gamma radiation. With the Digital Radiation Monitor, you can: • Monitor possible radiation exposure while working near radionuclides (Order Code DRM-BTD) • Ensure compliance with regulatory standards Contents • Check for leakage from X-ray machines and other sources • Screen for environmental contamination or environmental sources of 1 Introduction ............................................................................................................. 2 radioactivity How the DRM Detects Radiation ................................................................. 2 • Connect the Digital Radiation Monitor to a computer or data logger to record 2 Features ................................................................................................................... 3 and tabulate your data The Display................................................................................................... 3 The Switches ................................................................................................4 This manual gives complete instructions for using the Digital Radiation Monitor and The Detector..................................................................................................5 procedures for common applications. The Ports....................................................................................................... 5 3 Operation................................................................................................................ -

Release of Patients Administered Radioactive Materials
NEW YORK STATE DEPARTMENT OF HEALTH BUREAU OF ENVIRONMENTAL RADIATION PROTECTION DRAFT RADIATION GUIDE 10.17 RELEASE OF PATIENTS ADMINISTERED RADIOACTIVE MATERIALS A. INTRODUCTION Section 16.123(b) of 10 NYCRR Part 16 requires licensees to assess the radiation exposure to individuals from patients administered radioactive materials and take action, as appropriate, to reduce exposures to other individuals. These requirements apply for both diagnostic and therapeutic uses regardless of the amount administered. Section 16.123(b), Medical uses of radioactive material, states: P The licensee shall confine patients undergoing procedures authorized by ...until the total effective dose equivalent for the individuals (other than the patient) likely to receive the greatest dose is 5 mSv (500 mrem) or less. P When the total effective dose equivalent to any individual that could result from the release of a patient is likely to exceed 1 mSv (100 mrem), the licensee shall: • provide the patient, or his/her competent representative, written information on risks of radiation and methods for reducing the exposure of individuals; and • keep records of such patients release for a period of five years. This document is designed to provide guidance on determining the potential dose to an individual likely to receive the highest dose from exposure to the patient, to establish appropriate activities and dose rates for release, to provide guidelines for instructions to patients on how to reduce exposures to other individuals, to describe recordkeeping requirements, and to inform licensees of other potential problems associated with the release of patients containing radioactive materials. B. DISCUSSION The radiation dose to another individual from a patient is highly dependent on a number of factors, including the amount and type of radioactive material administered, the patient's living/working arrangements, ability/willingness to follow instructions, etc. -
Radiation Sources- Radiating Health and Progress…
RADIATION SOURCES- RADIATING HEALTH AND PROGRESS…. ….. BUT NEED REGULATION NEVERTHELESS!!! Anuradha V ATOMIC ENERGY REGULATORY BOARD Contents- The four W’s What are radiation sources? Where are they used? Why do we need them? When is their use dangerous and how to overcome this? 3 Applications of Radiation- All areas of life Medical- Diagnosis and treatment Industrial- Food processing, Radiography, Gauges and measurement Research – Irradiation of samples, Calibration sources, tracers Agriculture- Tracer studies MEDICAL USES RADIOTHERAPY INTERVENTIONAL RADIOLOGY RADIO-PHARMACEUTICALS COMPUTED TOMOGRAPHY BLOOD/TISSUE IRRADIATOR INDUSTRIAL USES FOOD IRRADIATION INDUSTRIAL RADIOGRAPHY NUCLEONIC GAUGES RESEARCH TRACER STUDY IRRADIATION OF SAMPLES Department of Atomic Energy Atomic Department of Image courtesy: courtesy: Image Alexander L.- Polonium poisoning of Russian spy Atomic bomb survivors “RADIATION GOOGLE IS INDEED DISASTROUS” Image courtesy: socialistworld.net Image courtesy: courtesy: Image THE QUESTION TO ASK IS NOT "IS THERE ANY RADIOACTIVITY PRESENT?" BUT RATHER, "HOW MUCH, AND IS IT ENOUGH TO BE HARMFUL?" Atomic Energy Regulatory Board, Anushakti nagar Mumbai 10 Safety Research Institute at Kalpakkam Regional Centers at Chennai, New Delhi and Kolkata Effects Linear- Non Threshold model for Radiation AERB mandates in this area for safety DNA damage reduction CANCER RISK Epilation Erythema GI/ CNS Symptoms area for Prevention Prevention area for Death mandates in this AERB These effects are more profound in the foetus and children “Licence in accordance with Atomic Energy (Radiation Protection)Rules, 2004 from AERB is mandatory requirement for the procurement and use of radiation sources in India”. 12 Safety Research funding Safety in application of nuclear and radiation facilities Environmental Impact Assessment Transport of Radioactive material Radioactive Waste Management Civil and Structural Engineering Spent Fuel Storage Reactor Physics Thermal Hydraulics/Fluid Structure Interactions in Reactors under Accident Conditions . -
Development of Chemical Dosimeters Development Of
SUDANSUDAN ACADEMYAGADEMY OFOF SCIENCES(SAS)SGIENGES(SAS) ATOMICATOMIC ENERGYEhTERGYRESEARCHESRESEARCHES COORDINATIONCOORDII\rATI ON COUNCILCOUNCIL - Development of Chemical Dosimeters A dissertation Submitted in a partial Fulfillment of the Requirement forfbr Diploma Degree in Nuclear Science (Chemistry) By FareedFadl Alla MersaniMergani SupervisorDr K.S.Adam MurchMarch 2006 J - - - CONTENTS Subject Page -I - DedicationDedication........ ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... I Acknowledgement ... '" ... ... ... ... ... ... '" ... ... ... ... '" ... '" ....... .. 11II Abstract ... ... ... '" ... ... ... '" ... ... ... ... -..... ... ... ... ... ... ..... III -I Ch-lch-1 DosimetryDosimefry - 1-1t-l IntroductionLntroduction . 1I - 1-2t-2 Principle of Dosimetry '" '" . 2 1-3l-3 DosimetryDosimefiySystems . 3J 1-3-1l-3-l primary standard dosimeters '" . 4 - 1-3-2l-3-Z Reference standard dosimeters ... .. " . 4 1-3-3L-3-3 Transfer standard dosimeters ... ... '" . 4 1-3-4t-3-4 Routine dosimeters . 5 1-4I-4 Measurement of absorbed dose . 6 1-5l-5 Calibration of DosimetryDosimetrvsystemsvstem '" . 6 1-6l-6 Transit dose effects . 8 Ch-2ch-2 Requirements of chemical dosimeters 2-12-l Introduction ... ... ... .............................................. 111l 2-2 Developing of chemical dosimeters ... ... .. ....... ... .. ..... 12t2 2-3 Classification of Dosimetry methods.methods .......................... 14l4 2-4 RequirementsRequiremsnts of ideal chemical dosimeters ,. ... 15 2-5 Types of chemical system .