Frontier Nursing : Nursing Practice in Medical
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

^8 Big Transports \ Local Tin Can Collection
y \ ■ ■ ■ r ■ MONDAY, APRIL S, IMi ^jtattrbratnr £ontitio Hri Average D*R^^hrenI*tioB '>,. ' , ■ ■' 'y ■ :-. ■ ' ■ \ Tht Weatkar For Mm Month m t M a n ^ 1948 Fofbrurt m t D. Wauthar M ; ^ a Inland F, Apaldlng, 'Jr., son of noon No. 3 went tp >the. top of Brookdeld street a i^ No.' 8 Mr. and Mrs. t-land Spalding of M a t ^ h e s t e ^ Noted Teacher Marine Train I Fires Keep Up Birch street for a fire that' was out at 7:10 last night to 18 Qnt >ntX B8 Oetard' stre e t's^ recently en- rning towards the woods and at road. Ths last firs of tba 8 ,1 0 5 Romawhaf eatdeo toulght; ilhnia- IISM In the A rm j^lr Forcef hae O^te Book I :'15 No. 2 had a call for grass at^8;35 whan No. 8 was aallw Menoibnr of tha Audit leWag^<wln«. d M Eeeslar .Field, Biloxi, Study Subje< rt 94sHayn4s atreot. At 3:10 No. tobods a t tho eomor of Bureau m t CdreuluttoUa »*»!. On Week'Ehd was again eaUod, this time to Schhol streoto. Mtsa,N^ aviation c^et basic Today ^anchetter-^A City of ViUage Charm •ftinooa at traJnlngSjfe gfadu*^ *" June April 5, 8, 7—ElxhIblUon of pot T" from Manchester fll0» aihool and tery of Liea Halpem, Dutch artist, Expression Clubyin De« South End Department ntered the University of.^ Oom.^ , * (TEN PAGES) / / V PRICE THREE CEN fs' ■om i^’^tirMt imrittU Im- Mary Cheney Library. iI^X1CN0.159 (ChMalbsd Adverttslag aq rkg* 8k ' MANCHESTER, CONN., TUESDAY, APRIL 6, 1943 pMtaMt ImmIm m mattan b* Icut,-' Tomorrow bate on. -

Direitos Autorais (Músicas Reproduzidas - ECAD)
SIMPATIA FM LTDA EPP EXPEDICIONÁRIO, 483 - CENTRO CAMPOS NOVOS - SC Fone: (49) 3541-0893 CNPJ: 03818131000179 Direitos Autorais (Músicas Reproduzidas - ECAD) Data Hora Título Intérprete Autor Gravadora Gênero Execução 01/02/2020 04:38:44 FINAL DO FIM GUSTTAVO LIMA GUSTTAVO LIMA PLAY SERTANEJO 2 01/02/2020 04:41:37 SEM CONTRAINDICAÇÃO DIEGO & VICTOR HUGO DIEGO & VICTOR HUGO PLAY SERTANEJO 2 POR TRÁS DA MAQUIAGEM 01/02/2020 04:44:54 MICHEL TELÓ MICHEL TELÓ PLAY SERTANEJO 2 (PART. MARÍLIA MENDONÇA) 01/02/2020 04:47:45 SOFRENDO FEITO UM LOUCO LUAN SANTANA LUAN SANTANA MIDI SERTANEJO 2 ERA PRA SER NESSA VIDA 01/02/2020 04:50:58 TÉO & EDU TÉO E EDU MIDI SERTANEJO 2 PART. MARCOS E BELUTTI 01/02/2020 04:54:48 EU QUERO É ROLO BRUNO & BARRETTO BRUNO E BARRETO MIDI SERTANEJO 2 PRA QUEM SE AMA (FT. EDSON 01/02/2020 04:57:46 DIEGO & ARNALDO Diego & Arnaldo MIDI SERTANEJO 2 & HUDSON) FLASH 01/02/2020 05:01:08 TALVEZ VOCÊ SE LEMBRE LEANDRO & LEONARDO Leandro & Leonardo 2 SERTANEJO FLASH 01/02/2020 05:04:52 SEU AMOR AINDA E TUDO BRUNO E MARRONE Bruno & Marrone 2 SERTANEJO BAR NÃO É FARMÁCIA (PART. 01/02/2020 05:08:46 LOUBET LOUBET PLAY SERTANEJO 2 BRUNINHO & DAVI) 01/02/2020 07:16:40 NOSSO LUGAR MARCOS & BELUTTI MARCOS & BELUTTI MIDI SERTANEJO 2 CLASSICOS 01/02/2020 07:55:59 O DOCE TOQUE DO AMOR ATHAÍDE & ALEXANDRE ATAÍDE & ALEXANDRE 2 SERTANEJO 01/02/2020 07:58:54 DECIDA MILIONARIO & JOSE RICO MILIONARIO & JOSE RICO MIDI SERTANEJO 2 01/02/2020 08:08:13 GIRASSOL KELL SMITH KELL SMITH PLAY POP 2 UM GIRASSOL DA COR DE SEU 01/02/2020 08:12:02 NENHUM DE NÓS NENHUM DE NóS GAVETA 2 CABELO 01/02/2020 08:16:06 VIM PRA FICAR IZA IZA MIDI POP 2 01/02/2020 08:19:08 É ISSO AÍ - SERTANEJO EDUARDO COSTA EDUARDO COSTA MIDI SERTANEJO 2 01/02/2020 08:22:30 MAUS BOCADOS CRISTIANO ARAÚJO CRISTIANO ARAÚJO MIDI SERTANEJO 2 01/02/2020 08:30:06 ÁGUA COM AÇÚCAR LUAN SANTANA LUAN SANTANA MIDI SERTANEJO 2 ALDAIR PLAYBOY PART. -

Spanglish Code-Switching in Latin Pop Music: Functions of English and Audience Reception
Spanglish code-switching in Latin pop music: functions of English and audience reception A corpus and questionnaire study Magdalena Jade Monteagudo Master’s thesis in English Language - ENG4191 Department of Literature, Area Studies and European Languages UNIVERSITY OF OSLO Spring 2020 II Spanglish code-switching in Latin pop music: functions of English and audience reception A corpus and questionnaire study Magdalena Jade Monteagudo Master’s thesis in English Language - ENG4191 Department of Literature, Area Studies and European Languages UNIVERSITY OF OSLO Spring 2020 © Magdalena Jade Monteagudo 2020 Spanglish code-switching in Latin pop music: functions of English and audience reception Magdalena Jade Monteagudo http://www.duo.uio.no/ Trykk: Reprosentralen, Universitetet i Oslo IV Abstract The concept of code-switching (the use of two languages in the same unit of discourse) has been studied in the context of music for a variety of language pairings. The majority of these studies have focused on the interaction between a local language and a non-local language. In this project, I propose an analysis of the mixture of two world languages (Spanish and English), which can be categorised as both local and non-local. I do this through the analysis of the enormously successful reggaeton genre, which is characterised by its use of Spanglish. I used two data types to inform my research: a corpus of code-switching instances in top 20 reggaeton songs, and a questionnaire on attitudes towards Spanglish in general and in music. I collected 200 answers to the questionnaire – half from American English-speakers, and the other half from Spanish-speaking Hispanics of various nationalities. -

A Song Only Dead Men Know Cassidy Foust Macalester College, [email protected]
Macalester College DigitalCommons@Macalester College English Honors Projects English Department Spring 5-1-2015 A Song Only Dead Men Know Cassidy Foust Macalester College, [email protected] Follow this and additional works at: http://digitalcommons.macalester.edu/english_honors Recommended Citation Foust, Cassidy, "A Song Only Dead Men Know" (2015). English Honors Projects. Paper 32. http://digitalcommons.macalester.edu/english_honors/32 This Honors Project - Open Access is brought to you for free and open access by the English Department at DigitalCommons@Macalester College. It has been accepted for inclusion in English Honors Projects by an authorized administrator of DigitalCommons@Macalester College. For more information, please contact [email protected]. 1 A Song Only Dead Men Know Cassidy Foust 2 One In old maps, the sea drips off at the edge of the parchment in what is supposed to be the end of the world. Mapmakers would draw monsters here: great sea beasts and serpents with mouths tall as a ship’s mast; winged harpies, their talons raised; beautiful sirens, selkies, and mermaids, their soft lips parted in deadly song. These were always Marin’s favorites, these wicked women, these horrible temptresses. Her grandfather, a grizzled old man who had once served as a mapmaker to the King of England himself, would set her down on his knee and unfurl long parchments of map, teaching her the names of all the waterways as her fingers traced the faded ink. “That’s the Irish Sea,” he would say, “It swirls down towards Europe right past the Salinges.” “Have you ever seen a selkie, Granddad?” Marin would ask, thumbing over the creature’s hair as if she could draw it into life. -

Songs by Title
Songs by Title Title Artist Title Artist - Human Metallica (I Hate) Everything About You Three Days Grace "Adagio" From The New World Symphony Antonín Dvorák (I Just) Died In Your Arms Cutting Crew "Ah Hello...You Make Trouble For Me?" Broadway (I Know) I'm Losing You The Temptations "All Right, Let's Start Those Trucks"/Honey Bun Broadway (I Love You) For Sentimental Reasons Nat King Cole (Reprise) (I Still Long To Hold You ) Now And Then Reba McEntire "C" Is For Cookie Kids - Sesame Street (I Wanna Give You) Devotion Nomad Feat. MC "H.I.S." Slacks (Radio Spot) Jay And The Mikee Freedom Americans Nomad Featuring MC "Heart Wounds" No. 1 From "Elegiac Melodies", Op. 34 Grieg Mikee Freedom "Hello, Is That A New American Song?" Broadway (I Want To Take You) Higher Sly Stone "Heroes" David Bowie (If You Want It) Do It Yourself (12'') Gloria Gaynor "Heroes" (Single Version) David Bowie (If You're Not In It For Love) I'm Outta Here! Shania Twain "It Is My Great Pleasure To Bring You Our Skipper" Broadway (I'll Be Glad When You're Dead) You Rascal, You Louis Armstrong "One Waits So Long For What Is Good" Broadway (I'll Be With You) In Apple Blossom Time Z:\MUSIC\Andrews "Say, Is That A Boar's Tooth Bracelet On Your Wrist?" Broadway Sisters With The Glenn Miller Orchestra "So Tell Us Nellie, What Did Old Ironbelly Want?" Broadway "So When You Joined The Navy" Broadway (I'll Give You) Money Peter Frampton "Spring" From The Four Seasons Vivaldi (I'm Always Touched By Your) Presence Dear Blondie "Summer" - Finale From The Four Seasons Antonio Vivaldi (I'm Getting) Corns For My Country Z:\MUSIC\Andrews Sisters With The Glenn "Surprise" Symphony No. -
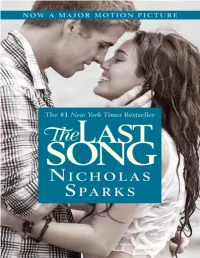
The Last Song
Copyright This book is a work of fiction. Names, characters, places, and incidents are the product of the author’s imagination or are used fictitiously. Any resemblance to actual events, locales, or persons, living or dead, is coincidental. Copyright © 2009 by Nicholas Sparks All rights reserved. Except as permitted under the U.S. Copyright Act of 1976, no part of this publication may be reproduced, distributed, or transmitted in any form or by any means, or stored in a database or retrieval system, without the prior written permission of the publisher. Grand Central Publishing Hachette Book Group 237 Park Avenue New York, NY 10017 Visit our website at www.HachetteBookGroup.com. www.twitter.com/grandcentralpub First eBook Edition: September 2009 Grand Central Publishing is a division of Hachette Book Group, Inc. The Grand Central Publishing name and logo is a trademark of Hachette Book Group, Inc. ISBN 978-0-446-55815-0 Contents Copyright Also by Nicholas Sparks Acknowledgments Prologue Chapter 1 Chapter 2 Chapter 3 Chapter 4 Chapter 5 Chapter 6 Chapter 7 Chapter 8 Chapter 9 Chapter 10 Chapter 11 Chapter 12 Chapter 13 Chapter 14 Chapter 15 Chapter 16 Chapter 17 Chapter 18 Chapter 19 Chapter 20 Chapter 21 Chapter 22 Chapter 23 Chapter 24 Chapter 25 Chapter 26 Chapter 27 Chapter 28 Chapter 29 Chapter 30 Chapter 31 Chapter 32 Chapter 33 Chapter 34 Chapter 35 Chapter 36 Chapter 37 Epilogue ALSO BY NICHOLAS SPARKS The Notebook Message in a Bottle A Walk to Remember The Rescue A Bend in the Road Nights in Rodanthe The Guardian The Wedding Three Weeks with My Brother (with Micah Sparks) True Believer At First Sight Dear John The Choice The Lucky One For Theresa Park and Greg Irikura My friends Acknowledgments As always, I have to start by thanking Cathy, my wife and my dream. -

Listening for a Life
Utah State University DigitalCommons@USU All USU Press Publications USU Press 2004 Listening for a Life Patricia Sawin Follow this and additional works at: https://digitalcommons.usu.edu/usupress_pubs Part of the Folklore Commons Recommended Citation Sawin, P. (2004). Listening for a life: A dialogic ethnography of Bessie Eldreth through her songs and stories. Logan: Utah State University Press. This Book is brought to you for free and open access by the USU Press at DigitalCommons@USU. It has been accepted for inclusion in All USU Press Publications by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. Listening for a Life 5/27/04 2:23 PM Page i Listening for a Life A Dialogic Ethnography of Bessie Eldreth through Her Songs and Stories Listening for a Life 5/27/04 2:23 PM Page ii Listening for a Life 5/27/04 2:23 PM Page iii Listening for a Life A Dialogic Ethnography of Bessie Eldreth through Her Songs and Stories Patricia Sawin Utah State University Press Logan, Utah Listening for a Life 5/27/04 2:23 PM Page iv Copyright © 2004 Utah State University Press All rights reserved Utah State University Press Logan, Utah 84322-7800 Publication of this book was supported by a grant from the University Researcch Council at the University of North Carolina, Chapel Hill. Manufactured in the United States of America Printed on acid-free paper Library of Congress Cataloging-in-Publication Data Sawin, Patricia. Listening for a life : a dialogic ethnography of Bessie Eldreth through her songs and stories / Patricia Sawin. -

BZN Lyrics Book
lyrics book All BZN lyrics together This is an exclusive release of BZN Online. In this release, all lyrics can be found, as they are presented via the BZN Online website. BZN Online does not guarantee the correctness of the contents of this document, nor does it guarantee its completeness. The latest version of this document can be found at www.bzn-online.com. This version of the document is generated on Wednesday, December 03, 2008. This release is made possible with the cooperation of: Etienne van Haren Leo Kolijn Guillaume Sourisce (www.franedvertaling.nl) Alphonsa van de Ven Marcel Versteeg Nothing from this release may be reproduced in any way without the explicit approval of the owners of the published work. This file is only provided for personal use and may not be republished or spreaded in any way. The rights on the contents of this release are with the respective owners. Copyright © 2008, BZN Online Preface During their 42 years of existence the band BZN (the Band Without a Name) from Volendam released many albums and singles and wrote hundreds of songs. Via the website of the band all these lyrics can be found and could be downloaded for personal use. Now that BZN no longer exists, we looked at a new way to make the lyrics available for download. The old format (a zip-file with HTML- files) could not be generated easily and was no longer completely up- to-date. We now chose to release an electronic book containing all lyrics. This method offers some advantages over the old method. -

JIM FORD LYRICS Compiled by Robin Dunn & Chrissie Van Varik
JIM FORD LYRICS Compiled by Robin Dunn & Chrissie van Varik Jim Ford was born 23 rd August 1941 in Paintsville, Johnson County, Kentucky, USA. His music is a blend of country, folk, funk and soul; Jim called himself ‘country funky’ – which is about right! He was found dead early in the evening of Sunday 18 th November 2007 in his trailer home by the Mendocino County Sheriff’s department . Only two albums were released during his lifetime: Harlan County (1969) and The Sounds Of Our Time (2007). In between he recorded numerous home demos as well as doing official recording sessions for Capitol and Paramount but none of the tracks laid down were ever issued at the time. In 2006, Swedish journalist L-P Anderson tracked Jim down and discovered a wealth of reel-to-reel tapes piled high on the floor of Jim’s trailer home. The Sounds Of Our Time (2007) contains Jim’s 1969 debut album, complemented with tracks from those reels. Plans were made to release more and even to record again but sadly Jim died before any of this could take place. However, several albums have been issued since, including the two albums Jim recorded in the early 1970s for Capitol and Paramount but were kept in the can. Below is a list of Jim Ford releases. • Harlan County (1969) • The Sounds Of Our Time (2007) • Point Of No Return (2008) • Big Mouth USA – The Unissued Paramount Album (2009) • The Unissued Capitol Album (2009) • Demolition Expert – Rare Acoustic Demos (2011) Included in our Lyric List are songs composed by Jim but recorded by other artists. -

Planilha De Programação Musical - Rádio
PLANILHA DE PROGRAMAÇÃO MUSICAL - RÁDIO RAZÃO SOCIAL: SISTEMA 103 DE RADIOS LTDA - EPP CNPJ: 82721226000146 NOME FANTASIA: DIAL: 103.7 CIDADE: UF: EXECUÇÃO DATA HORA MÚSICA INTÉRPRETE AUTOR GRAVADORA AO VIVO MECÂNICA 01/08/2019 00:00 THUNDER IMAGINE DRAGONS X 01/08/2019 05:11 BOMBACHA RISCADA ALBINO MANIQUE X 01/08/2019 05:15 CLAREANDO O DIA GRUPO RODEIO X 01/08/2019 05:18 RIO GRANDE TCHE OS SERRANOS X 01/08/2019 05:23 NAO PODEMO SE ENTREGA PROS HOMEJOCA MARTINS X 01/08/2019 05:30 CASEIRO XIRU MISSIONEIRO X 01/08/2019 05:34 IMAGEM DO RIO GRANDE NILTON FERREIRA X 01/08/2019 05:41 BAGUAL PEDRO ORTACA X 01/08/2019 05:46 RELHO TRANCADO TEIXEIRINHA X 01/08/2019 05:49 RESPOSTA DO RELHO TRANCADO GILDO DE FREITAS X 01/08/2019 05:53 BAGUAL SEM FREIO BAITACA X 01/08/2019 05:56 BOMBACHA RISCADA ALBINO MANIQUE X 01/08/2019 06:12 MOURO NEGRO MAURO MORAES X 01/08/2019 06:17 MOURO NEGRO JOAO LUIZ CORREA X 01/08/2019 06:27 QUANDO EU VIM DA MINHA TERRA PORCA VEIA X 01/08/2019 06:35 PRA MATEAR COM DEUS ROMARIO GAUCHO X 01/08/2019 06:43 MADRUGADOR ITA CUNHA X 01/08/2019 06:52 ULTIMA LEMBRANCA CESAR OLIVEIRA E ROGERIO MELO X 01/08/2019 06:58 O BRANCO DOS TEUS CABELOS GAROTOS DE OURO X 01/08/2019 07:23 PROSA DOS LENCOS OS MONARCAS X 01/08/2019 07:42 GAUCHAO DE APARTAMENTO JOAO LUIZ CORREA X 01/08/2019 07:52 ABA LARGA ALBINO MANIQUE X 01/08/2019 13:31 BRUTO MEMO BRUNO E BARRETO X 01/08/2019 13:34 I DON'T CARE ED SHEERAN & JUSTIN BIEBER X 01/08/2019 13:38 YEARS & YEARS KING X 01/08/2019 13:49 SONG ON FIRE NICKELBACK X 01/08/2019 13:52 MELODY JAMES BLUNT X 01/08/2019 -

COMPLAINT Receipt No: 0973-21033857
Wixen Music Publishing, Inc. v. Spotify USA Inc. Doc. 1 Att. 1 EXHIBIT A MUSICAL COMPOSITION LIST Composition Title U.S. Copyright Registration Number or Application Number 1% PA 1-339-382 3:36 PA0001799397 11:11 PA0001589410 60% PA 1-314-745 143 PA0001927806 367 PAu002701327 717 PAu002722038 1998 PA 900-730 2002 PA0001647911 November 1942 PA0001635686 #1 ZERO PA0001281054 (GIRL WE GOT A) GOOD THING 1-5748105248 (I GOT) TWO HANDS EU0000285380 (IF YOU COULD ONLY) SEE ME NOW PA0000267669 (IF YOU'RE WONDERING IF I WANT YOU PA0001666840 TO) I WANT YOU (LOVE ECHOES IN THE) PINE HILLS PA0001187980 (MONA LISA) WHO I AM PA0000907642 (SHE'S GONNA) RESPECT ME PA0000062032 (VARIATIONS ON) BAMBOO PA0001279092 (WHAT'S YOUR) ANGLE? PA0000968734 (YOU'LL NEVER FIND ANYONE) TO BE A EU0000169346 SLAVE ............. PA0001267039 1, 2 STEP PA0001305520 10 A.M. AUTOMATIC PA0001397356 10 LOVERS PA0001902461 10 THOUSAND WAYS 1-5682847781 10 YOU US PA0002019265 100 TIMES FUCKEDER PA 1-314-745 100 YEARS PA0001876028 100 YEARS 1-6002566401 101 DALMATIONS PAu003422528 10102 EAST 7TH AVENUE PA 1-942-917 1040 BLUES PA0000668988 110TH PAu200872004 12 DAYS OF THE BLUES PA0001098136 Exhibit A – Musical Composition List Dockets.Justia.com 13 STITCHES PA 1-144-468 143 (KELLY'S SONG) 2011 PA0001927806 16 YEARS PA0001721692 16 YEARS OF LOVE PAu001370611 17TH MOON PA0001053823 19 SEVENTY SUMTHIN' 1-5842578060 1990'S THEME PAu000425537 2 MINUTES IN SEPTEMBER PA0001314523 20 YEAR OLD LOVER PA000133155 200 LIVES EU0000319301 2000 VOLTS PA0001013448 21@12 PA0001738830 22 YEARS -

ASCAP/BMI Comment
Stuart Rosen Senior Vice President General Counsel November 20, 2015 Chief, Litigation III Section Antitrust Division U.S. Department of Justice 450 5th Street NW, Suite 4000 Washington, DC 20001 Re: Justice Department Review of the BMI and ASCAP Consent Decrees To the Chief of the Litigation III Section: BMI recently alerted its community of affiliated songwriters, composers and publishers to the profound impact 100% licensing would have on their careers, both creatively and financially, if it were to be mandated by the U.S. Department of Justice. In a call to action, BMI provided a letter, one for songwriters and one for publishers, to which their signatures could be added. The response was overwhelming. BMI received nearly 13,000 signatures from writers, composers and publishers of all genres of music, at all levels in their careers. Some of the industry's most well- known songwriters added their names, including Stephen Stills, Cynthia Weil, Steve Cropper, Ester Dean, Dean Pitchford, Congressman John Hall, Trini Lopez, John Cafferty, Gunnar Nelson, Lori McKenna, Shannon Rubicam and Don Brewer, among many others. Enclosed you will find the letters, with signatures attached. On behalf of BMI, I strongly urge you to consider the voices of thousands of songwriters and copyright owners reflected here before making a decision that will adversely affect both the creators, and the ongoing creation of, one ofAmerica's most important cultural and economic resources. Vert truly yours, Stuart Rosen 7 World Trade Center, 250 Greenwich Street, New York, NY 10007-0030 (212) 220-3153 Fax: (212) 220-4482 E-Mail: [email protected] ® A Registered Trademark of Broadcast Music, Inc.