Intestinal Transplantation Page 2 Overview This Information Booklet Is Designed to Give You Information on Intestinal Transplantation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 1 Table 2 Table 3 Table 4 Colonoscopy-Related Costs
Digestive Health Network, Inc. List of Tables Top 10 Physician Specialties Performing Colonoscopies, Medicare Fee-for- Table 1 Service, 2015 Colonoscopy-related Costs, Medicare Fee-for-Service Beneficiaries who Table 2 Received a Screening or Diagnostic Colonoscopy, 2015 Colonoscopy-related Costs, Medicare Fee-for-Service Beneficiaries who Table 3 Received a Colonoscopy in an Ambulatory Surgical Center (ASC), Hospital Outpatient Department, or Physician Office, 2015 Proportion of Medicare Fee-for-Service Medicare Beneficiaries who Received Table 4 a Colonoscopy and were Treated in the Emergency Department within 7 Days of the procedure, 2015 Digestive Health Network, Inc. Responses to Questions Among Medicare beneficiaries, how many colonoscopies are performed in the US, by type of Q1 physician? Nearly 2 million screening and diagnostic colonoscopies were performed in 2015. Of these, over 78% were performed by a gastroenterologist. Nearly 10% were performed by a general surgeon and about 6% were performed by an internal medicine specialist. These results are shown in Table 1. Q2 What proportion of spending on colonoscopies is accounted for by physician services? In 2015, Medicare expenditures associated with colonoscopies totaled over $1.3 billion. (This excludes anesthesiology, pathology, radiology, and other costs identified in Table 2.) Approximately 31% of this amount, or $416 million was associated with professional fees. Q3 What share of Part B Medicare spending is accounted for by colonoscopies? Medicare Part B expenditures in 2015 totaled over $131 billion (data not shown). Colonoscopy costs accounted for approximately 1.03% of this total. Q4 What are the costs associated with colonoscopies for the different settings of care? Costs associated with colonoscopies in ambulatory surgical centers (ASC), hospital outpatient departments (HOPD), and physician offices are shown in Table 3. -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -
High Resolution Anoscopy Overview
High Resolution Anoscopy Overview Naomi Jay, RN, NP, PhD University of California San Francisco Email: [email protected] Disclosures No Disclosures Definition of HRA Examination of the anus, anal canal and perianus using a colposcope with 5% acetic acid and Lugol’s solution. Basic Principles • Office-based procedure • Adapted from gynecologic colposcopy. • Validated for anal canal. • Similar terminology and descriptors. may be unfamiliar to non-gyn providers. • Comparable to vaginal and vulvar colposcopy. • Clinicians familiar with cervical colposcopy may be surprised by the difficult transition. Anal SCJ & AnTZ • Original vs. current SCJ less relevant. • TZ features less common, therefore more difficult to appreciate. • SCJ more subtle, difficult to see in entirety requires more manipulation & acetic acid. • Larger area of metaplastic changes overlying columnar epithelium compared to endocervix. • Most lesions found in the AnTZ. Atypical Metaplasia • Atypical metaplasia may indicate the presence of HSIL. • Radiate over distal rectum from SCJ. • Thin, may wipe off. • Features to look for indicating potential lesions: • Atypical clustered glands (ACG) • Lacy metaplastic borders (LM) • Epithelial Honeycombing (EH) Lugol’s. Staining • More utility in anus compared to cervix. • Adjunctive to help define borders, distinguish between possible LSIL/HSIL. • Most HSIL will be Lugol’s negative • LSIL may be Lugol’s partial or negative • Applied focally with small cotton swabs to better define an acetowhite lesion. •NOT a short cut to determine presence or absence of lesions, acetic acid is used first and is applied frequently. Anal vs. Cervical Characteristics • Punctation & Mosaic rarely “fine” mostly “coarse”. • Mosaic pattern mostly associated with HSIL. • Atypical vessels may be HSIL or cancer • Epithelial honeycombing & lacy metaplasia unique anal descriptors. -

Information for Patients Having a Sigmoid Colectomy
Patient information – Pre-operative Assessment Clinic Information for patients having a sigmoid colectomy This leaflet will explain what will happen when you come to the hospital for your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. Your surgeon will have already discussed your treatment with you and will give advice about what to do when you get home. What is a sigmoid colectomy? This operation involves removing the sigmoid colon, which lies on the left side of your abdominal cavity (tummy). We would then normally join the remaining left colon to the top of the rectum (the ‘storage’ organ of the bowel). The lines on the attached diagram show the piece of bowel being removed. This operation is done with you asleep (general anaesthetic). The operation not only removes the bowel containing the tumour but also removes the draining lymph glands from this part of the bowel. This is sent to the pathologists who will then analyse each bit of the bowel and the lymph glands in detail under the microscope. This operation can often be completed in a ‘keyhole’ manner, which means less trauma to the abdominal muscles, as the biggest wound is the one to remove the bowel from the abdomen. Sometimes, this is not possible, in which case the same operation is done through a bigger incision in the abdominal wall – this is called an ‘open’ operation. It does take longer to recover with an open operation but, if it is necessary, it is the safest thing to do. -

Combined Endo-Laparoscopic Surgery for Difficult Benign Colorectal Polyps
485 Review Article (Current Strategies in Colon Cancer Management) Combined endo-laparoscopic surgery for difficult benign colorectal polyps Zhong-Hui Liu1, Li Jiang1, Fion Siu-Yin Chan1,2, Michael Ka-Wah Li3, Joe King-Man Fan1,2,3 1Department of Surgery, The University of Hong Kong-Shenzhen Hospital, Shenzhen 518053, China; 2Department of Surgery, The University of Hong Kong, Hong Kong, China; 3Asia-Pacific Endo-Lap Surgery Group (APELS), Hong Kong, China Contributions: (I) Conception and design: JKM Fan, MKW Li; (II) Administrative support: MKW Li; (III) Provision of study materials or patients: FSY Chan; (IV) Collection and assembly of data: ZH Liu, L Jiang; (V) Data analysis and interpretation: ZH Liu; FSY Chan; JKM Fan; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Joe King-Man Fan, MBBS (HK), MS (HKU), FRCSEd, FACS. Department of Surgery, The University of Hong Kong-Shenzhen Hospital, Shenzhen 518053, China. Email: [email protected]. Abstract: Prevention of colorectal cancer (CRC) depends largely on the detection and removal of colorectal polyps. Despite the advances in endoscopic techniques, there are still a subgroup of polyps that cannot be treated purely by endoscopic approach, which comprise of about 10–15% of all the polyps. These so-called “difficult colorectal polyps” are polyps with large size, morphology, at difficult location, scarring or due to recurrence, which have historically been managed by surgical segmental resection. In treating benign difficult colorectal polyps, we have to balance the operative risks and morbidities associated with surgical segmental resection. Therefore, combined endoscopic and laparoscopic surgery (CELS) has been developed to remove this subgroup of difficult benign polyps. -

Diagnostic Direct Laryngoscopy, Bronchoscopy & Esophagoscopy
Post-Operative Instruction Sheet Diagnostic Direct Laryngoscopy, Bronchoscopy & Esophagoscopy Direct Laryngoscopy: Examination of the voice box or larynx (pronounced “lair-inks”) under general anesthesia. An instrument called a laryngoscope is carefully placed into the mouth and used to visualize the larynx and surrounding structures. Bronchoscopy: Examination of the windpipe below the voice box in the neck and chest under general anesthesia. A long narrow telescope is passed through the larynx and used to carefully inspect the structures of the trachea and bronchi. Esophagoscopy: Examination of the swallowing pipe in the neck and chest under general anesthesia. An instrument called an esophagoscope is passed into the esophagus (just behind the larynx and trachea) and used to visualize the mucus membranes and surrounding structures of the esophagus. Frequently a small biopsy is taken to evaluate for signs of esophageal inflammation (esophagitis). What to Expect: Diagnostic airway endoscopy procedures generally take about 45 minutes to complete. Usually the procedure is well-tolerated and the child is back-to-normal the next day. Mild throat or tongue discomfort may persist for a few days after the procedure and is usually well-controlled with over-the-counter acetaminophen (Tylenol) or ibuprofen (Motrin). Warning Signs: Contact the office immediately at (603) 650-4399 if any of the following develop: • Worsening harsh, high-pitched noisy-breathing (stridor) • Labored breathing with chest retractions or flaring of the nostrils • Bluish discoloration of the lips or fingernails (cyanosis) • Persistent fever above 102°F that does not respond to Tylenol or Motrin • Excessive coughing or respiratory distress during feeding • Coughing or throwing up bright red blood • Excessive drowsiness or unresponsiveness Diet: Resume baseline diet (no special postoperative diet restrictions). -
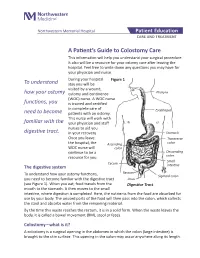
A Patient's Guide to Colostomy Care
Northwestern Memorial Hospital Patient Education CARE AND TREATMENT A Patient’s Guide to Colostomy Care This information will help you understand your surgical procedure. It also will be a resource for your ostomy care after leaving the hospital. Feel free to write down any questions you may have for your physician and nurse. During your hospital Figure 1 To understand stay you will be visited by a wound, how your ostomy ostomy and continence Pharynx (WOC) nurse. A WOC nurse functions, you is trained and certified in complete care of Esophagus need to become patients with an ostomy. This nurse will work with familiar with the your physician and staff nurses to aid you digestive tract. in your recovery. Stomach Once you leave Transverse the hospital, the Ascending colon WOC nurse will colon continue to be a Descending resource for you. colon Small Cecum The digestive system intestine Rectum To understand how your ostomy functions, Sigmoid colon you need to become familiar with the digestive tract Anus (see Figure 1). When you eat, food travels from the Digestive Tract mouth to the stomach. It then moves to the small intestine, where digestion is completed. Here, the nutrients from the food are absorbed for use by your body. The unused parts of the food will then pass into the colon, which collects the stool and absorbs water from the remaining material. By the time this waste reaches the rectum, it is in a solid form. When the waste leaves the body, it is called a bowel movement (BM), stool or feces. -
Laryngeal Endoscopy (Rigid, Flexible, and Stroboscopy)
Laryngeal Endoscopy (Rigid, Flexible, and Stroboscopy) Visualization of the larynx can be performed via several different methods. Special tools are required for laryngeal evaluation. Mirror laryngoscopy (1) o While the patient’s tongue is protruded, a mirror is placed in the posterior oropharynx with gentle pressure on the soft palate while light is reflected caudally into the larynx. o Mirror laryngoscopy can be challenging for both the examiner and the patient, has limited magnification, and may require topical anesthesia. o Mirror laryngoscopy provides the most accurate color representation of laryngeal and pharyngeal tissue because there is no light or digital distortion. Flexible laryngoscopy (2) o A flexible laryngoscope is placed into the nasal cavity, through the naso- and oropharynx and positioned cephalad to the larynx for a full laryngeal assessment. o Nasal anesthesia (lidocaine) and/or nasal decongestants (oxymetazoline/phenylephrine) may be applied to the nose for the purpose of improving patient comfort and tolerance o Supplemental procedures such as dynamic voice assessment (comprehensive laryngeal movement evaluation), functional endoscopic evaluation of swallowing (+/- sensory testing), and other laryngeal procedures (ex. injections, laser surgery, biopsies) can be performed during flexible laryngoscopy. o Flexible laryngoscopy is ideal for evaluating vocal fold weakness, real-time/unencumbered evaluation of task-specific abnormalities (ex. my voice is problematic when I do this), and assessing the intensity of glottal attack. Rigid Laryngoscopy (3) o Rigid laryngoscopy is performed by placing a rigid 70- or 90-degree telescope into the oropharynx during tongue protrusion. o Sometimes, oropharyngeal and/or tongue application of anesthesia (ex. lidocaine, cetacaine) can be helpful for patient tolerance. -

Hybrid Procedure Offers a Less Invasive Alternative to Colectomy
The better way to get better Hybrid procedure offers a less invasive alternative to colectomy Insufflation gas provides important advantage The colonoscopy-laparoscopy procedure is made possible through the combined skills of the gastroenterologist and laparoscopic surgeon, and the use of CO2 rather than ambient air for insufflation — the introduction of gas into the colon to improve visibility. CO2 is more quickly absorbed by the gastrointestinal tract and results in less bowel distension, giving the laparoscopic surgeon a better field of vision within the abdominal cavity. © Copyright Olympus. Used with permission. “Some patients who would have required a bowel resection can instead benefit from this A new, minimally invasive procedure that is a hybrid of colonoscopy and less invasive procedure. We’re laparoscopy is proving to be a safe and effective alternative to open colectomy using this combined technique (removal of part of the colon) for patients with benign colon polyps that are as a way for patients to avoid colectomy,” explains James not removable endoscopically. Yoo, M.D., a colorectal surgeon Patients who undergo this hybrid procedure experience less pain and often go at UCLA. “This procedure home after only one or two days. Scarring and wound complications are minimal involves tiny incisions for the as the laparoscopic surgeon makes only small, keyhole incisions in the abdomen laparoscopic instruments and patients stay in the hospital only rather than the long incision characteristic of a traditional colectomy. a day or two.” WWW.UCLAHEALTH.ORG 1-800-UCLA-MD1 (1-800-825-2631) Who can benefit from the procedure? Participating When a routine colonoscopy reveals polyps, they are usually removed at the Physicians time of the procedure as a precaution against their progression to cancer. -

42 CFR Ch. IV (10–1–12 Edition) § 410.35
§ 410.35 42 CFR Ch. IV (10–1–12 Edition) the last screening mammography was (1) Colorectal cancer screening tests performed. means any of the following procedures furnished to an individual for the pur- [59 FR 49833, Sept. 30, 1994, as amended at 60 FR 14224, Mar. 16, 1995; 60 FR 63176, Dec. 8, pose of early detection of colorectal 1995; 62 FR 59100, Oct. 31, 1997; 63 FR 4596, cancer: Jan. 30, 1998] (i) Screening fecal-occult blood tests. (ii) Screening flexible § 410.35 X-ray therapy and other radi- sigmoidoscopies. ation therapy services: Scope. (iii) In the case of an individual at Medicare Part B pays for X-ray ther- high risk for colorectal cancer, screen- apy and other radiation therapy serv- ing colonoscopies. ices, including radium therapy and ra- (iv) Screening barium enemas. dioactive isotope therapy, and mate- (v) Other tests or procedures estab- rials and the services of technicians ad- lished by a national coverage deter- ministering the treatment. mination, and modifications to tests [51 FR 41339, Nov. 14, 1986. Redesignated at 55 under this paragraph, with such fre- FR 53522, Dec. 31, 1990] quency and payment limits as CMS de- termines appropriate, in consultation § 410.36 Medical supplies, appliances, with appropriate organizations and devices: Scope. (2) Screening fecal-occult blood test (a) Medicare Part B pays for the fol- means— lowing medical supplies, appliances (i) A guaiac-based test for peroxidase and devices: activity, testing two samples from (1) Surgical dressings, and splints, each of three consecutive stools, or, casts, and other devices used for reduc- (ii) Other tests as determined by the tion of fractures and dislocations. -

Double Barrel Wet Colostomy for Urinary and Fecal Diversion
Open Access Clinical Image J Urol Nephrol November 2017 Vol.:4, Issue:2 © All rights are reserved by Kang,et al. Journal of Double Barrel Wet Colostomy for Urology & Urinary and Fecal Diversion Nephrology Yu-Hao Xue and Chih-Hsiung Kang* Keywords: Double barrel wet colostomy; Urinary diversion; Fecal Department of Urology, Chang Gung Memorial Hospital-Kaohsiung diversion Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan, Republic of China Abstract Address for Correspondence A 60-year-old male who had a history of spinal cord injury received Chih-Hsiung Kang, Department of Urology, Chang Gung Memorial loop colostomy for fecal diversion and cystostomy for urinary diversion. Hospital - Kaohsiung Medical Center, Chang Gung University College Because he was diagnosed with muscle invasive bladder cancer, of Medicine, Taiwan, E- mail: [email protected] radical cystectomy and double barrel wet colostomy was conducted. Submission: 30 October, 2017 Computed tomography showed simultaneous urinary and fecal Accepted: 06 November, 2017 diversion and stone formation in the distal segment of colon conduit Published: 10 November, 2017 with urinary diversion. Copyright: © 2017 Kang CH, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, Introduction provided the original work is properly cited. In patients with an advanced primary or recurrent carcinoma, double-barreled wet colostomy can be used for pelvic exenteration Bilateral hydroureters and mild hydronephrosis were noted and and urinary tract reconstruction. It is a technique that separate we suspected the calculi impacted in bilateral ureteto-colostomy urinary and fecal diversion with a single abdominal stoma. -
Flexible Sigmoidoscopy – Outpatients
Flexible sigmoidoscopy – Outpatients You have been referred by your doctor to have a flexible sigmoidoscopy. his information booklet has been written to explain the procedure. This will help you to make an informed decision before consenting to the procedure. If you are unable to attend your appointment please inform us as soon as possible. Please ensure you read this booklet and the enclosed consent form thoroughly. Please also complete the enclosed health questionnaire. You may be contacted by an endoscopy trained nurse before your procedure to go through the admission process and answer any queries you may have. If you are not contacted please come to your appointment at the time stated in your letter. Please note your appointment time is your arrival time on the unit and not the time of your procedure. If you have any mobility issues or if there is a possibility you could be pregnant, please contact the appointment staff on 01284 713551 Please remember there will be other patients in the unit who may arrive after you but are taken in for their procedure before you, this is for medical reasons or they are seeing a different doctor. Due to limited space available and to maintain other patients’ privacy and dignity, we only allow patients (and carers) through to the ward area. Relatives/ escorts will be contacted once you are ready for collection. The Endoscopy Unit endeavours to offer single sex facilities, and we aim to make you stay as comfortable and stress free as possible. Source: Endoscopy Reference No: 5035-14 Issue date: 8/1/21 Review date: 8/1/24 Page 1 of 11 Medication If you are taking WARFARIN, CLOPIDOGREL, RIVAROXABAN or any other anticoagulant (blood thinning medication), please contact the appointment staff on 01284 713551, your GP or anticoagulation nurse, as special arrangements may be necessary.