Nassau-Queens-PPS-Lo
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Beny Primm Was Interviewed by Nancy D
on-site media transcription services Dr. Beny Primm was interviewed by Nancy D. Campbell June 18, 2006 and February 3, 2010 for the Oral History of Substance Abuse Research project, which was supported by the National Science Foundation; the University of Michigan Substance Abuse Research Center; the College on Problems of Drug Dependence; and Rensselaer Polytechnic Institute. Ideas expressed do not reflect official positions of any of these organizations. Transcripts of the oral histories are held at the Bentley Historical Library, University of Michigan, Ann Arbor. The interview below is reposted with permission of Dr. Primm and the Oral History of Substance Abuse Research project. Information on other interviews conducted as part of the Oral History of Substance Abuse Research can be found at http://sitemaker.umich.edu/umsarc/oral_history_interviews. NANCY CAMPBELL NANCY CAMPBELL: Can you tell me how you got to the University of Geneva for medical school? BP: In 1950 I finished college at West Virginia State College, which is now West Virginia State University. I was a member of the Reserve Officers Training Corps, ROTC, during the Korean War. I was a premed, biological science, and German major, and I knew I was going to get drafted. I even stayed an extra year to finish ROTC because I had transferred to West Virginia State College from another school. You had to be there four years to do ROTC. Although I was premed, my degree was a bachelor of NANCY CAMPBELL/ADDICTION RESEARCH/BENY PRIMM Page 2 of 56 science in education. I could either go into teaching and be a coach, because I was a basketball player, or I could end up going into the service. -

Careconnect Facilities
CareConnect Facilities Yale-New Haven Bridgeport Northern Westchester Phelps Memorial Greenwich White Plains Peconic Bay Medical Center Montefiore Medical Huntington Centers Glen Cove Syosset Zucker North Shore Lenox Hill Hillside University Plainview Manhattan Eye Ear & Throat Hospital N LIJ Medical Center Lenox Hill Healthplex Forest Cohen Nassau University Southside Hills Children’s Medical Center Wyckoff Heights South Oaks Franklin Staten Island Maimonides University (North) Staten Island University (South) Hospitals • Bridgeport Hospital, 267 Grant St, Bridgeport, CT 06610, P: 203-688-8412 • Forest Hills Hospital, 102-01 66th Road, Forest Hills, NY 11375, P: 718-830-4000 • Franklin Hospital, 900 Franklin Avenue, Valley Stream, NY 11580, P: 516-256-6000 • Glen Cove Hospital, 101 St. Andrews Lane, Glen Cove, NY 11542, P: 516-674-7540 • Greenwich Hospital, 5 Perryridge Road, Greenwich, CT 06830, P: 203-688-8412 • Huntington Hospital, 270 Park Avenue, Huntington, NY 11743, P: 631-351-2000 • Lenox Hill HealthPlex, 36 Seventh Avenue, New York, NY 10011, P: 212-434-2000 • Lenox Hill Hospital, 100 East 77th Street, New York, NY 10021, P: 212-434-2000 • Long Island Jewish Medical Center, 270-05 76th Avenue, New Hyde Park, NY 11040, P: 718-470-7000 • Maimonides Medical Center, 4802 Tenth Avenue, Brooklyn, NY 11219, P: 718-283-6000 • Manhattan Eye, Ear & Throat Hospital, 210 East 64th Street, New York, NY 10021, P: 212-838-9200 • Montefiore Medical Center - Montefiore Westchester Square, 2475 Saint Raymonds Avenue, Bronx, NY 10461, P: 718-430-7300 • Montefiore Medical Center - Montefiore Hospital, 111 East 210th Street, Bronx, NY 10467, P: 718-920-4321 • Montefiore Medical Center - Wakefield Hospital, 600 East 233rd Street, Bronx, NY 10466, P: 718-920-9000 • Montefiore Medical Center - Weiler Hospital, 1825 Eastchester Road, Bronx, NY 10461, P: 718-904-2000 • Montefiore Mt. -

Careconnect Facilities
CareConnect Facilities Manhattan Hospitals Yale-New Haven Northern Harlem Westchester Bridgeport Metropolitan Lenox Hill Manhattan Eye, Ear & Throat Phelps Memorial Lenox Health Greenwich Greenwich Montefiore White Plains Village Medical Bellevue Centers Peconic Bay Medical Center North Central Bronx Jacobi Huntington Glen Cove Lincoln Syosset North Shore University Zucker Hillside Plainview Elmhurst LIJ Medical Center Cohen Children’s LIJ Forest Nassau University Hills Queens Medical Center Southside Woodhull Wyckoff Heights South Oaks Kings County LIJ Valley Stream Staten Island Maimonides University (North) Coney Island Staten Island University (South) For a searchable list of CareConnect’s providers, visit CareConnect.com/providersearch Hospitals • Bellevue Hospital Center, 462 First Avenue, New York, NY 10016, P: 212-562-4141 • Bridgeport Hospital, 267 Grant St, Bridgeport, CT 06610, P: 203-688-8412 • Coney Island Hospital, 2601 Ocean Parkway, Brooklyn, NY 11235, P: 718 616-3000 • Elmhurst Hospital Center, 79-01 Broadway, Elmhurst, NY, 11373, P: 718-334-4000 • Glen Cove Hospital, 101 St. Andrews Lane, Glen Cove, NY 11542, P: 516-674-7540 • Greenwich Hospital, 5 Perryridge Road, Greenwich, CT 06 830, P: 203-688-8412 • Harlem Hospital Center, 506 Lenox Avenue, New York, NY 10037, P: 212-939-1000 • Huntington Hospital, 270 Park Avenue, Huntington, NY 11743, P: 631-351-2000 • Jacobi Medical Center, 1400 Pelham Parkway South, Bronx, NY 10461, P: 718-918-5000 • Kings County Hospital Center, 451 Clarkson Avenue, Brooklyn, NY 11203, P: 718-245-3131 -

NURSING HOME SHARPS COLLECTION SITES in NEW YORK STATE (Revised on March 15, 2016 )
NURSING HOME SHARPS COLLECTION SITES in NEW YORK STATE (Revised on March 15, 2016 ) County Nursing Home Address Phone # Hours of Operation Location of Drop‐off 780 Albany Shaker Rd., Thursdays Albany County Nursing Home 518-869-2231 Receiving Department Albany Albany, 12111 8 AM- Noon 180 Washington Ave. Ext., Daughters Of Sarah Nursing Center 518-456-7831 8 AM-4 PM Reception desk in lobby Albany Albany, 12203 Reception Main Campus - 40 Autumn Drive, Sharps received in an Eddy Village Green at Beverwyck 518-482-8774 8 AM-8 PM Slingerlands, 12159 appropriate sealed puncture Albany proof container Guilderland Center Rehabilitation 428 Route 146, Guilderland, 518-861-5141 10 AM-1 PM Lobby Albany and Extended Care Facility 12085 Our Lady Of Hope Residence-little 1 Jeanne Jugan Lane, Wednesday 518-785-4551 Lobby Albany Sisters Of The Poor Latham, 12110 9-11AM 2 Mercycare Lane, Monday thru Friday Main Lobby at Reception Our Lady Of Mercy Life Center 518-464-8100 Albany Guilderland, 12084 9:00AM -3:00PM Desk 27 Hackett Blvd., Monday-Friday St Margarets Center 518-591-3300 Reception Desk Albany Albany, 12208 8:00 AM-4 PM St Peter's Nursing and Rehabilitation 301 Hackett Blvd., Monday-Friday 518-525-7600 Reception Desk Albany Center Albany, 12208 10:00 AM-3 PM Teresian House Nursing Home Co 200 Washington Ave Ext., Front Entrance, Infrom 518-456-2000 8 AM-3 PM Albany Inc Albany 12203 Switchboard Operator Monday-Friday 140 West Main St., Cuba Memorial Hospital Inc Snf 585-968-2000 8 AM-4 PM Hospital Lobby Cuba 14727 Allegany Highland Park Rehabilitation -
Resource Guide for Mental Health 2021-2022
2021 -2022 Resource Guide for Mental Health It’s okay not to be okay. www.squarecarehealth.com Table of Contents Contents Table of Contents ................................................................................................................................... Introduction ......................................................................................................................................... 1 Postpartum Care: ................................................................................................................................. 2 Links to resources for Fathers & Families experiencing Postpartum Depression: .................................. 7 Fertility Specialists: .............................................................................................................................. 8 Infertility Counseling: ......................................................................................................................... 16 Online Therapy for Moms: ................................................................................................................. 21 Outpatient Psychiatry Services: .......................................................................................................... 25 Outpatient Psychiatry Services that provides Therapy: ...................................................................... 31 Psychotherapy Services ONLY: ........................................................................................................... 48 Resources for LBGT+ -

Hospitals Locations at a Glance
Hospitals Locations at a glance Nassau County Syosset Hospital Zucker Hillside Hospital Glen Cove Hospital 221 Jericho Turnpike 75-59 263rd Street 101 St. Andrews Lane Syosset, NY 11791 Glen Oaks, NY 11004 Glen Cove, NY 11542 (516) 496-6400 (718) 470-8100 (516) 674-7300 Suffolk County Manhattan Long Island Jewish (LIJ) Huntington Hospital Lenox Hill Hospital Valley Stream 270 Park Avenue 100 East 77th Street 900 Franklin Avenue Huntington, NY 11743 New York, NY 10075 Valley Stream, NY 11580 (631) 351-2000 (212) 434-2000 (516) 256-6000 Mather Hospital Manhattan Eye, Ear North Shore University Hospital 75 North Country Road & Throat Hospital 300 Community Drive Port Jefferson, NY 11777 210 East 64th Street Manhasset, NY 11030 (631) 473-1320 New York, NY 10065 (516) 562-0100 (212) 838-9200 Peconic Bay Medical Center Long Island Jewish 1300 Roanoke Avenue Bronx Medical Center Riverhead, NY 11901 St. Barnabas Hospital 270-05 76th Avenue (631) 548-6000 4487 Third Avenue New Hyde Park , NY 11040 Bronx, NY 10457 (718) 470-7000 South Oaks Hospital (718) 960-9000 400 Sunrise Highway Plainview Hospital Amityville, NY 11701 Kings 888 Old Country Road (631) 264-4000 Maimonides Medical Center Plainview, NY 11803 4802 Tenth Avenue (516) 719-3000 Southside Hospital Brooklyn, NY 11219 301 East Main Street (718) 285-3300 Steven & Alexandra Cohen Bay Shore, NY11706 Children’s Medical Center of (631) 968-3000 Wyckoff Heights Medical Center New York 374 Stockholm Street 269-01 76th Avenue Queens Brooklyn, NY 11237 New Hyde Park , NY 11040 Long Island Jewish -
The Bipolar Prodrome Symptom Interview and Scale-Prospective
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Hofstra Northwell Academic Works (Hofstra Northwell School of Medicine) Donald and Barbara Zucker School of Medicine Journal Articles Academic Works 2014 The iB polar Prodrome Symptom Interview and Scale-Prospective (BPSS-P): description and validation in a psychiatric sample and healthy controls C. U. Correll Hofstra Northwell School of Medicine D. M. Olvet Northwell Health A. M. Auther Hofstra Northwell School of Medicine M. Hauser Hofstra Northwell School of Medicine T. Kishimoto Hofstra Northwell School of Medicine See next page for additional authors Follow this and additional works at: https://academicworks.medicine.hofstra.edu/articles Part of the Psychiatry Commons Recommended Citation Correll CU, Olvet D, Auther AM, Hauser M, Kishimoto T, Carrion R, Snyder S, Cornblatt BA. The ipoB lar Prodrome Symptom Interview and Scale-Prospective (BPSS-P): description and validation in a psychiatric sample and healthy controls. 2014 Jan 01; 16(5):Article 996 [ p.]. Available from: https://academicworks.medicine.hofstra.edu/articles/996. Free full text article. This Article is brought to you for free and open access by Donald and Barbara Zucker School of Medicine Academic Works. It has been accepted for inclusion in Journal Articles by an authorized administrator of Donald and Barbara Zucker School of Medicine Academic Works. Authors C. U. Correll, D. M. Olvet, A. M. Auther, M. Hauser, T. Kishimoto, R. Carrion, S. Snyder, and B. A. Cornblatt This article is available at Donald and Barbara Zucker School of Medicine Academic Works: https://academicworks.medicine.hofstra.edu/articles/996 NIH Public Access Author Manuscript Bipolar Disord. -

Queens County Assessment
Northwell Health 2019 Community Health Needs Assessment: Queens County Assessment Encompassing the following Northwell Health Hospital: Long Island Jewish Forest Hills 1 Queens County Health Indicator Status Since 2016 CHNA The 2016-2019 Implementation Plan activities have had an impact in improving and meeting New York State Prevention Agenda Objectives that were related to health disparities, chronic disease, safe environments, maternal child health, STD/HIV, vaccine preventable diseases, healthcare-associated infections and behavioral health as shown below. Since 2018, Northwell Health has delivered over 13,000 community health programs and over 22,000 health screenings. Examples of interventions that helped achieved these goals include robust chronic disease and cancer screening programs; implementation of culturally relevant evidence-based chronic disease self-management education; prevention of childhood obesity through school- based projects as well as promotion of policies and practices in support of breastfeeding; creation of community environments that promote and support healthy food and beverage choices and physical activity; elimination of exposure to secondhand smoke and prevention of the initiation of tobacco use by youth, especially among low socioeconomic status (SES) populations and the promotion of tobacco cessation, especially among low SES populations and those with poor mental health; and strengthened infrastructure to promote mental, emotional and behavioral wellbeing. However, the burden of health disparities, chronic disease, obesity and behavioral health issues is still present as demonstrated below by the indicators that have not met the New York State Department of Health (NYSDOH) Prevention Agenda Objectives and/or have worsened indicating the need to continue to primarily address the 2019-2024 priority agenda items of Prevent Chronic Disease and Promote Well Being and Prevent Mental and Substance Use Disorders as well as including strategies that can improve other priority areas as well. -

Carrier Hospital Guide
2021 Carrier Hospital Guide EmblemHealth EmblemHealth EmblemHealth Oscar Oxford Oxford Hospital Name Healthfirst County Prime Select Care Millenium Circle Metro Liberty Albert Einstein College of Medicine √ √ √ √ √ Bronx BronxCare Health System √ √ √ √ Bronx Calvary Hospital √ √ √ √ Bronx Jacobi Medical Center √ √ √ √ √ Bronx Lincoln Medical & Mental Health Center √ √ √ √ √ Bronx Montefiore Medical Center √ √ √ √ Bronx Montefiore Westchester Square √ √ Bronx North Central Bronx Hospital √ √ √ √ √ Bronx St. Barnabas Hospital √ √ √ √ √ √ Bronx Total Hospitals in Bronx County 9 4 4 7 2 7 7 Midhudson Regional Hospital √ √ √ Dutchess Northern Dutchess Hospital √ √ √ √ Dutchess Vassar Brothers Medical Center √ √ √ √ Dutchess Total Hospitals in Dutchess County 3 2 0 0 0 3 3 Brookdale University Hospital Medical Center √ √ √ √ √ Kings Brooklyn Hospital Center √ √ √ √ √ √ √ Kings Coney Island Hospital Center √ √ √ √ √ Kings Interfaith Medical Center √ √ √ √ √ Kings Kings County Hospital Center √ √ √ √ √ Kings Kingsbrook Jewish Medical Center √ √ √ √ √ Kings Maimonides Medical Center √ √ √ Kings Mount Sinai Brooklyn √ √ √ √ √ √ √ Kings NYC Health + Hospitals √ √ √ √ √ Kings New York Community Hospital of Brooklyn √ √ √ √ Kings New York Presbyterian Methodist √ √ √ √ √ Kings NYU Lutheran Medical Center √ √ √ √ Kings SUNY Downstate Medical Center √ √ √ √ Kings Woodhull Medical and Mental Health Center √ √ √ √ √ Kings Wyckoff Heights Medical Center √ √ √ √ Kings Total Hospitals in Kings County 15 6 11 10 3 13 15 Cohen Children's Medical Center √ √ -

Lincoln Medical and Mental Health Center 234 Eugenio Maria De Hostos Blvd.(149Th Street) the Bronx, New York 10451 718-579-5000
LINCOLN LINCOLN MEDICAL AND MENTAL HEALTH CENTER 234 EUGENIO MARIA DE HOSTOS BLVD.(149TH STREET) THE BRONX, NEW YORK 10451 718-579-5000 LINCOLN MEDICAL AND MENTAL HEALTH CENTER Predoctoral Psychology Internship Program Dear Applicant: Thank you for your interest in the Internship Program at Lincoln Medical and Mental Health Center. Please take the time to review our 2017-2018 Psychology Internship Program brochure (for the 2018-2019 training year). Please note that we will be operating in accordance with the APPI Online Application process for the 2018-2019 internship year. We are accepting online applications this year. Please click on the following link for more information: http://www.appic.org/match/5_3_match_application.html Also, to maximize your chances for a successful match, please take the time to read below, as well as our brochure. ♦ Each applicant is responsible for compiling all the documentation that is requested, including APPI Online Application, CV, transcripts, and only three letters of recommendation. ♦ Your application must be received by November 30th. ♦ Please be aware that we participate in the APPIC Internship Matching Program. You must obtain the Application Agreement Package from the National Matching Services Inc, P.O.Box 1208, Lewiston, NY 14092-8208. Tel# (716)282- 4013, Fax# (716)282-0611, Internet web address www.natmatch.com/psychint. (Please note: once matched, all interns-to- be are required to pass preliminary background checks and drug screenings in August with our Human Resources Department. It is upon successful clearance that internship may begin in September.) ♦ Our program code number is 144711 ♦ Our training program involves a wide range of training opportunities, from newborns to geriatric populations. -

Health Systems and Hospitals
FS000006046 121st Street Family Health Center CS000434510 121st. Street Hc CS000434511 35th Street Hc FS000001385 35th Street Health Center CS000000267 3rd Avenue Pediatrics CS000000284 43rd Street Family Practice CS000434512 53rd Street Hc CS000140193 54 Main Street Medical Practice Pc RX000020261 58th Street Pharmacy, Inc., Town Drug And Surgical CS000000410 609 Fulton Pediatrics Pc CS000000405 61st St Family Health Center CS000436719 786 Medical Pc FS000010161 850 Grand St Campus High School CS000000425 8th Avenue Medical Office CS000000498 93 17 Medical Office Pc CS000187023 @phillips Ambulatory Care Center CS000430681 A & E Ob Gyn Pc FS000000534 A Holly Patterson Extended Care Facility FS000006802 A Merryland Health Center CS000437620 A Plus Medical Care CS000438635 A To Z Pediatrics, Pc CS000438636 A&d; Medical, Pc CS000000633 Aaron B Grotas Md CS000000634 Aaron Daluiski Md CS000000995 Aaron David Ob/gyn CS000000658 Aaron E Walfish Md CS000000665 Aaron N Manson Md CS000434513 Aaron Woodall, Md CB000000002 Abbott House As of: September 7, 2021 Page 1 MH000018730 Abbott House, Inc. CS000000788 Abbydek CS000000795 Abbydek Family Medical Practice CS000434158 Abbydek Family Medical Practice CS000000800 Abbydek Family Medical Practice CS000000867 Abdul A Khuwaja Md CS000436229 Abdul-haki Issah, Md, Pc CS000000986 Abk Neurological Associates FS000004471 Able Health Care Service Inc CS000001174 Abu M Haque M.d CS000438945 Academic Health Care Center FS000000941 Acadia Center For Nursing And Rehabilitation CS000001348 Access Community Health -
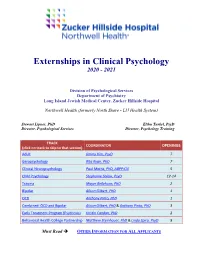
Externships in Clinical Psychology 2020 - 2021
Externships in Clinical Psychology 2020 - 2021 Division of Psychological Services Department of Psychiatry Long Island Jewish Medical Center, Zucker Hillside Hospital Northwell Health (formerly North Shore - LIJ Health System) Stewart Lipner, PhD Elihu Turkel, PsyD Director, Psychological Services Director, Psychology Training TRACK COORDINATOR OPENINGS (click on track to skip to that section) Adult Jimmy Kim, PsyD 7 Geropsychology Rita Ryan, PhD 7 Clinical Neuropsychology Paul Mattis, PhD, ABPP-CN 5 Child Psychology Stephanie Solow, PsyD 12-14 Trauma Mayer Bellehsen, PhD 2 Bipolar Alison Gilbert, PhD 1 OCD Anthony Pinto, PhD 1 Combined: OCD and Bipolar Alison Gilbert, PhD & Anthony Pinto, PhD 3 Early Treatment Program (Psychosis) Kristin Candan, PhD 2 Behavioral Health College Partnership Matthew Steinhauer, PhD & Linda Spiro, PsyD 8 Must Read OTHER INFORMATION FOR ALL APPLICANTS Externships in Clinical Psychology: 2020 – 2021 Brochure Page | 2 The Professional Setting Long Island Jewish Medical Center (LIJMC), a member of Northwell Health (formerly North Shore – LIJ Health System), is a voluntary tertiary care, non-profit facility. The three divisions, Long Island Jewish Hospital, The Zucker Hillside Hospital and the Steven and Alexandra Cohen Children's Medical Center, are all situated on a 48-acre landscaped campus in New Hyde Park on the border of Queens and Nassau counties, 15 miles east of Manhattan. The Medical Center and its affiliates serve patients from some of the most diverse ethnic, cultural and economic backgrounds. As a partner in the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Northwell's graduate medical education program is one of the largest in New York State.