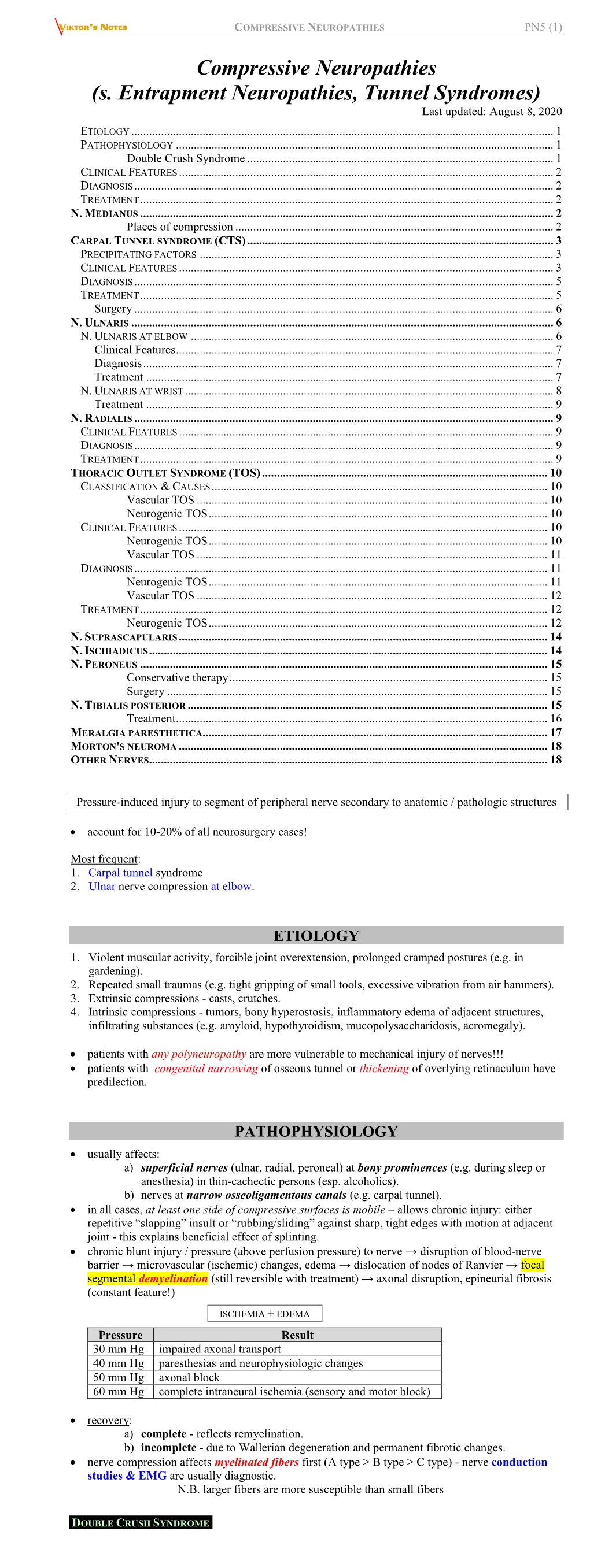
PN5. Compressive Neuropathies.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Occupational Therapy Guide for Entry
University of North Dakota UND Scholarly Commons Occupational Therapy Capstones Department of Occupational Therapy 2008 An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries Ryan Edwards University of North Dakota Follow this and additional works at: https://commons.und.edu/ot-grad Part of the Occupational Therapy Commons Recommended Citation Edwards, Ryan, "An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries" (2008). Occupational Therapy Capstones. 57. https://commons.und.edu/ot-grad/57 This Scholarly Project is brought to you for free and open access by the Department of Occupational Therapy at UND Scholarly Commons. It has been accepted for inclusion in Occupational Therapy Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. AN OCCUPATIONAL THERAPY GUIDE FOR ENTRY-LEVEL THERAPISTS NOT SPECIALIZING IN THE TREATMENT OF UPPER EXTREMITY DYSFUNCTION: THREE COMMON CUMULATIVE TRAUMA INJURIES by Ryan Edwards Advisor: Anne Haskins PhD, OTR/L A Scholarly Project Submitted to the Occupational Therapy Department of the University of North Dakota In partial fulfillment of the requirements for the degree of Master’s of Occupational Therapy Grand Forks, North Dakota August 1, 2008 This Scholarly Project Paper, submitted by Ryan Edwards in partial fulfillment of the requirement for the Degree of Master’s of Occupational Therapy from the University of North Dakota, has been read by the Faculty Advisor under whom the work has been done and is hereby approved. -

Piriformis Syndrome: the Literal “Pain in My Butt” Chelsea Smith, PTA
Piriformis Syndrome: the literal “pain in my butt” Chelsea Smith, PTA Aside from the monotony of day-to-day pains and annoyances, piriformis syndrome is the literal “pain in my butt” that may not go away with sending the kids to grandmas and often takes the form of sciatica. Many individuals with pain in the buttock that radiates down the leg are experiencing a form of sciatica caused by irritation of the spinal nerves in or near the lumbar spine (1). Other times though, the nerve irritation is not in the spine but further down the leg due to a pesky muscle called the piriformis, hence “piriformis syndrome”. The piriformis muscle is a flat, pyramidal-shaped muscle that originates from the front surface of the sacrum and the joint capsule of the sacroiliac joint (SI joint) and is located deep in the gluteal tissue (2). The piriformis travels through the greater sciatic foramen and attaches to the upper surface of the greater trochanter (or top of the hip bone) while the sciatic nerve runs under (and sometimes through) the piriformis muscle as it exits the pelvis. Due to this close proximity between the piriformis muscle and the sciatic nerve, if there is excessive tension (tightness), spasm, or inflammation of the piriformis muscle this can cause irritation to the sciatic nerve leading to symptoms of sciatica (pain down the leg) (1). Activities like sitting on hard surfaces, crouching down, walking or running for long distances, and climbing stairs can all increase symptoms (2) with the most common symptom being tenderness along the piriformis muscle (deep in the gluteal region) upon palpation. -

Piriformis Syndrome Is Overdiagnosed 11 Robert A
American Association of Neuromuscular & Electrodiagnostic Medicine AANEM CROSSFIRE: CONTROVERSIES IN NEUROMUSCULAR AND ELECTRODIAGNOSTIC MEDICINE Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 AANEM COURSE F AANEM 52ND Annual Scientific Meeting Monterey, California CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 COURSE F AANEM 52nd Annual Scientific Meeting Monterey, California AANEM Copyright © September 2005 American Association of Neuromuscular & Electrodiagnostic Medicine 421 First Avenue SW, Suite 300 East Rochester, MN 55902 PRINTED BY JOHNSON PRINTING COMPANY, INC. ii CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Faculty Loren M. Fishman, MD, B.Phil Scott J. Primack, DO Assistant Clinical Professor Co-director Department of Physical Medicine and Rehabilitation Colorado Rehabilitation and Occupational Medicine Columbia College of Physicians and Surgeons Denver, Colorado New York City, New York Dr. Primack completed his residency at the Rehabilitation Institute of Dr. Fishman is a specialist in low back pain and sciatica, electrodiagnosis, Chicago in 1992. He then spent 6 months with Dr. Larry Mack at the functional assessment, and cognitive rehabilitation. Over the last 20 years, University of Washington. Dr. Mack, in conjunction with the Shoulder he has lectured frequently and contributed over 55 publications. His most and Elbow Service at the University of Washington, performed some of the recent work, Relief is in the Stretch: End Back Pain Through Yoga, and the original research utilizing musculoskeletal ultrasound in order to diagnose earlier book, Back Talk, both written with Carol Ardman, were published shoulder pathology. -

Lumbosacral Plexus Entrapment Syndrome. Part One: a Common Yet Little-Known Cause of Chronic Pelvic and Lower Extremity Pain
3-A Running head: ANAESTHESIA, PAIN & INTENSIVE CARE www.apicareonline.com ORIGINAL ARTICLE Lumbosacral plexus entrapment syndrome. Part one: A common yet little-known cause of chronic pelvic and lower extremity pain Kjetil Larsen, CES, George C. Chang Chien, D O2 ABSTRACT Corrective exercise specialist, Training & Rehabilitation, Oslo Lumbosacral plexus entrapment syndrome (LPES) is a little-known but common cause Norway of chronic lumbopelvic and lower extremity pain. The lumbar plexus, including the 2 Director of pain management, lumbosacral tunks emerge through the fibers of the psoas major, and the proximal Ventura County Medical Center, sciatic nerve beneath the piriformis muscles. Severe weakness of these muscles may Ventura, CA 93003, USA. lead to entrapment plexopathy, resulting in diffuse and non-specific pain patterns Correspondence: Kjetil Larsen, CES, Corrective throughout the lumbopelvic complex and lower extremities (LPLE), easily mimicking Exercise Specialist, Training & other diagnoses and is therefore likely to mislead the interpreting clinician. It is a Rehabilitation, Oslo Norway; pathology very similar to that of thoracic outlet syndrome, but for the lower body. This Kjetil@trainingandrehabilitation. two part manuscript series was written in an attempt to demonstrate the existence, com; pathophysiology, diagnostic protocol as well as interventional strategy for LPES, and Tel.: +47 975 45 192 its efficacy. Received: 23 November 2018, Reviewed & Accepted: 28 Key words: Pelvic girdle; Pain, Pelvic girdle; Lumbosacral plexus entrapment syndrome; February 2019 Piriformis syndrome; Nerve entrapment; Double-crush; Pain, Chronic; Fibromyalgia Citation: Larsen K, Chien GCC. Lumbosacral plexus entrapment syndrome. Part one: A common yet little-known cause of chronic pelvic and lower extremity pain. -

ICD9 & ICD10 Neuromuscular Codes
ICD-9-CM and ICD-10-CM NEUROMUSCULAR DIAGNOSIS CODES ICD-9-CM ICD-10-CM Focal Neuropathy Mononeuropathy G56.00 Carpal tunnel syndrome, unspecified Carpal tunnel syndrome 354.00 G56.00 upper limb Other lesions of median nerve, Other median nerve lesion 354.10 G56.10 unspecified upper limb Lesion of ulnar nerve, unspecified Lesion of ulnar nerve 354.20 G56.20 upper limb Lesion of radial nerve, unspecified Lesion of radial nerve 354.30 G56.30 upper limb Lesion of sciatic nerve, unspecified Sciatic nerve lesion (Piriformis syndrome) 355.00 G57.00 lower limb Meralgia paresthetica, unspecified Meralgia paresthetica 355.10 G57.10 lower limb Lesion of lateral popiteal nerve, Peroneal nerve (lesion of lateral popiteal nerve) 355.30 G57.30 unspecified lower limb Tarsal tunnel syndrome, unspecified Tarsal tunnel syndrome 355.50 G57.50 lower limb Plexus Brachial plexus lesion 353.00 Brachial plexus disorders G54.0 Brachial neuralgia (or radiculitis NOS) 723.40 Radiculopathy, cervical region M54.12 Radiculopathy, cervicothoracic region M54.13 Thoracic outlet syndrome (Thoracic root Thoracic root disorders, not elsewhere 353.00 G54.3 lesions, not elsewhere classified) classified Lumbosacral plexus lesion 353.10 Lumbosacral plexus disorders G54.1 Neuralgic amyotrophy 353.50 Neuralgic amyotrophy G54.5 Root Cervical radiculopathy (Intervertebral disc Cervical disc disorder with myelopathy, 722.71 M50.00 disorder with myelopathy, cervical region) unspecified cervical region Lumbosacral root lesions (Degeneration of Other intervertebral disc degeneration, -
Reference List for RMA425-2 As at 7 April 2020 Number
ULNAR NEUROPATHY AT THE ELBOW RMA ID Reference List for RMA425-2 as at 7 April 2020 Number Addas BM (2012). Ulnar neuropathy caused by traumatic arterio-venous 63167 fistula following gunshot wound. Neurosciences, 17(2): 165-6. Al-Najjim M, Mustafa A, Fenton C, et al (2013). Giant solitary synovial osteochondromatosis of the elbow causing ulnar nerve neuropathy: a 81900 case report and review of the literature. J Brachial Plex Peripher Nerve Inj, 8(1): 1. Altun Y, Aygun SM, Cevik MU, et al (2013). Relation between 63195 electrophysiological findings and diffusion weighted magnetic resonance imaging in ulnar neuropathy at the elbow. J Neuroradiol, 40(4): 260-6. Aly AR, Rajasekaran S, Obaid H, et al (2013). Bilateral ulnar neuropathy 63758 at the elbow secondary to neuropathic arthropathy associated with syringomyelia. PM & R, 5(6): 533-8. Andersen JH, Frost P, Fuglsang-Frederiksen A, et al (2012). Computer 81462 use and ulnar neuropathy: results from a case-referent study. Work, 41(Suppl 1): 2434-7. Babal JC, Mehlman CT, Klein G (2010). Nerve injuries associated with 81463 pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop, 30(3): 253-63. Balakrishnan A, Chang YJ, Elliott DA, et al (2012). Intraneural lipoma of 81901 the ulnar nerve at the elbow: A case report and literature review. Can J Plast Surg, 20(3): e42-3. Bales J, Bales K, Baugh L, et al (2012). Evaluation for ulnar neuropathy 81464 at the elbow in Ironman triathletes: physical examination and electrodiagnostic evidence. Clin J Sport Med, 22(2): 126-31. Balik G, Balik MS, Ustuner I, et al (2014). -

The Piriformis Syndrome. a Sciatic Nerve Entrapment Misdiagnosed As Lumbar Radiculopathy
VOLUME 72 | ISSUE 2 | APRIL - JUNE 2021 Actcase reportA The Piriformis Syndrome. A sciatic nerve entrapment misdiagnosed as lumbar radiculopathy. A case report and literature review E.K.Frangakis M.D. abstract The term Piriformis Syndrome describes an extrapelvic pressure of the whole or part of the Sciatic Nerve, at the level of the Piriformis muscle caused by various conditions and characterized Clinically by symptoms of sciatica. As early as 1928 Yeoman described extra pelvic entrapment of the sciatic nerve by the piriformis muscle as a cause of sciatica. After Mixter and Barr in 1934 described nerve root compression by disc pro- lapse as a cause of sciatica, this diagnosis dominated the Clinical thinking for nearly three decades and what had been previously described was nearly forgotten. The development of imaging techniques revealed other intraspinal compressing elements. On the other hand, cases of negative root exploration for Sciatica focused attention to extrapelvic sciatic nerve pathology. This report concerns the case of a patient, who after a nega- tive root exploration for severe sciatica proved to have an extrapelvic cause for this problem at the level of the piriformis muscle due mainly to anatomic variation of the sciatic nerve in relation to the piriformis muscle. KEY WORDS: Sciatica, Sciatic nerve, Piriformis Muscle Case report referred her to a specialist who treated her with A sixty-four-year lady suffered from a severe sci- epidural steroid injection and physiotherapy with- atica in the S1 distribution of the left leg i.e. pain out any improvement. The patient was referred to in the left buttock radiating to the posterior aspect us with the diagnosis of Lumbar radiculopathy. -

Perioperative Upper Extremity Peripheral Nerve Injury and Patient Positioning: What Anesthesiologists Need to Know
Anaesthesia & Critical Care Medicine Journal ISSN: 2577-4301 Perioperative Upper Extremity Peripheral Nerve Injury and Patient Positioning: What Anesthesiologists Need to Know Kamel I* and Huck E Review Article Lewis Katz School of Medicine at Temple University, USA Volume 4 Issue 3 Received Date: June 20, 2019 *Corresponding author: Ihab Kamel, Lewis Katz School of Medicine at Temple Published Date: August 01, 2019 University, MEHP 3401 N. Broad street, 3rd floor outpatient building ( Zone-B), DOI: 10.23880/accmj-16000155 Philadelphia, United States, Tel: 2158066599; Email: [email protected] Abstract Peripheral nerve injury is a rare but significant perioperative complication. Despite a variety of investigations that include observational, experimental, human cadaveric and animal studies, we have an incomplete understanding of the etiology of PPNI and the means to prevent it. In this article we reviewed current knowledge pertinent to perioperative upper extremity peripheral nerve injury and optimal intraoperative patient positioning. Keywords: Nerve Fibers; Proprioception; Perineurium; Epineurium; Endoneurium; Neurapraxia; Ulnar Neuropathy Abbreviations: PPNI: Perioperative Peripheral Nerve 2018.The most common perioperative peripheral nerve Injury; MAP: Mean Arterial Pressure; ASA CCP: American injuries involve the upper extremity with ulnar Society of Anesthesiology Closed Claims Project; SSEP: neuropathy and brachial plexus injury being the most Somato Sensory Evoked Potentials frequent [3,4]. In this article we review upper extremity PPNI with regards to anatomy and physiology, Introduction mechanisms of injury, risk factors, and prevention of upper extremity PPNI. Perioperative peripheral nerve injury (PPNI) is a rare complication with a reported incidence of 0.03-0.1% [1,2]. Anatomy and Physiology of Peripheral PPNI is a significant source of patient disability and is the Nerves second most common cause of anesthesia malpractice claims [3,4]. -

Review Article Entrapment Neuropathies in the Upper and Lower Limbs: Anatomy and MRI Features
Hindawi Publishing Corporation Radiology Research and Practice Volume 2012, Article ID 230679, 12 pages doi:10.1155/2012/230679 Review Article Entrapment Neuropathies in the Upper and Lower Limbs: Anatomy and MRI Features Qian Dong, Jon A. Jacobson, David A. Jamadar, Girish Gandikota, Catherine Brandon, Yoav Morag, David P. Fessell, and Sung-Moon Kim Division of Musculoskeletal Radiology, Department of Radiology, University of Michigan Health System, 1500 East Medical Center Drive, TC 2910R, Ann Arbor, MI 48109-5326, USA Correspondence should be addressed to Qian Dong, [email protected] Received 20 June 2012; Revised 30 August 2012; Accepted 25 September 2012 Academic Editor: Avneesh Chhabra Copyright © 2012 Qian Dong et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Peripheral nerve entrapment occurs at specific anatomic locations. Familiarity with the anatomy and the magnetic resonance imaging (MRI) features of nerve entrapment syndromes is important for accurate diagnosis and early treatment of entrapment neuropathies. The purpose of this paper is to illustrate the normal anatomy of peripheral nerves in the upper and lower limbs and to review the MRI features of common disorders affecting the peripheral nerves, both compressive/entrapment and noncompressive, involving the suprascapular nerve, the axillary nerve, the radial nerve, the ulnar nerve, and the median verve in the upper limb and the sciatic nerve, the common peroneal nerve, the tibial nerve, and the interdigital nerves in the lower limb. 1. Introduction itself and is considered superior in delineating the associated indirect signs related to muscle denervation [2, 4]. -

Cubital Tunnel Syndrome Guidance
CUBITAL TUNNEL SYNDROME GUIDANCE Author Louise Ross ([email protected]) Organisation NHS Greater Glasgow and Clyde Created 15/04/2016 15:32:54 Modified 26/10/2016 16:17:15 Modified By Louise Ross This pathway can be viewed at http://www.ckp.scot.nhs.uk/Published/Viewer.aspx?id=1743 Copyright © NHS Greater Glasgow and Clyde 2012. All rights reserved Cubital Tunnel Syndrome Guidance Author: Louise Ross CUBITAL TUNNEL SYNDROME GUIDANCE AHP Exit/ Parallel Serious Red Flags Routes Pathology Cubital Tunnel Syndrome Post Operatively Mild - Moderate Signs Moderate - Severe Signs and and Symptoms Symptoms 1st Line Management Place on hold/ Review in 6/52 Discharge Escalate 2nd Line Management Review Discharge Escalate Surgical Opinion/ List for surgery Post Operative Key More Infomation Decision Discharge Intervention Red Flag Self-Management Default Page 1/9 Cubital Tunnel Syndrome Guidance Author: Louise Ross GENERAL RELATED INFORMATION FOR PATHWAY Copyright Information Copyright © NHS Greater Glasgow and Clyde, 2013-2016, All rights reserved Page 2/9 Cubital Tunnel Syndrome Guidance Author: Louise Ross SPECIFIC RELATED INFORMATION FOR PATHWAY SECTIONS RED FLAGS Pathways Related pathway: MSK Foot and Ankle Red Flags NHSGGC SERIOUS PATHOLOGY Pathways Related pathway: Serious Pathology AHP EXIT/ PARALLEL ROUTES Pathways Related pathway: exit routes x 6 CUBITAL TUNNEL SYNDROME Information Description Cubital tunnel syndrome occurs due to compression of the ulnar nerve at the elbow. It is the second most common nerve compression and causes para/anaesthesia of the little and ulnar half of the ring finger with weakness of small muscles of the hand and/or the thumb. -

Sacroiliac Joint Dysfunction and Piriformis Syndrome
Classic vs. Functional Movement Approach in Physical Therapy Setting Crista Jacobe-Mann, PT Nevada Physical Therapy UNR Sports Medicine Center Reno, NV 775-784-1999 [email protected] Lumbar Spine Intervertebral joints Facet joints Sacroiliac joint Anterior ligaments Posterior ligaments Pelvis Pubic symphysis Obturator foramen Greater sciatic foramen Sacrospinous ligament Lesser sciatic foramen Sacrotuberous ligament Hip Capsule Labrum Lumbar spine: flexion and extension ~30 total degrees of rotation L1-L5 Facet joints aligned in vertical/saggital plane SI joints 2-5 mm in all directions, passive movement, not caused by muscle activation Shock absorption/accepting load with initial contact during walking Hip Joints Extension 0-15 degrees 15% SI joint pain noted in chronic LBP patients Innervation: L2-S3 Classic signs and symptoms Lower back pain generally not above L5 transverse process Pain can radiate down posterior thigh to posterior knee joint, glutes, sacrum, iliac crest sciatic distribution Pain with static standing, bending forward, donning shoes/socks, crossing leg, rising from chair, rolling in bed Relief with continuous change in position Trochanteric Bursitis Piriformis Syndrome Myofascial Pain Lumbosacral Disc Herniation and Bulge Lumbosacral Facet Syndrome J. Travell suspects Si joint pain may causes piriformis guarding and lead to Piriformis syndrome… Tenderness to palpation of PSIS, lower erector spinae, quadratus lumborum and gluteal muscles Sometimes positive SLR Limited hip mobility -
Peripheral Nerve Disorders
CLINICAL GUIDELINES PND Imaging Policy Version 1.0 Effective February 14, 2020 eviCore healthcare Clinical Decision Support Tool Diagnostic Strategies: This tool addresses common symptoms and symptom complexes. Imaging requests for individuals with atypical symptoms or clinical presentations that are not specifically addressed will require physician review. Consultation with the referring physician, specialist and/or individual’s Primary Care Physician (PCP) may provide additional insight. CPT® (Current Procedural Terminology) is a registered trademark of the American Medical Association (AMA). CPT® five digit codes, nomenclature and other data are copyright 2017 American Medical Association. All Rights Reserved. No fee schedules, basic units, relative values or related listings are included in the CPT® book. AMA does not directly or indirectly practice medicine or dispense medical services. AMA assumes no liability for the data contained herein or not contained herein. © 2019 eviCore healthcare. All rights reserved. PND Imaging Guidelines V1.0 Peripheral Nerve Disorders (PND) Imaging Guidelines Abbreviations for Peripheral Nerve Disorders Imaging Guidelines 3 PN-1: General Guidelines 4 PN-2: Focal Neuropathy 5 PN-3: Polyneuropathy 7 PN-4: Brachial Plexus 8 PN-5: Lumbar and Lumbosacral Plexus 9 PN-6: Muscle Disorders 10 PN-7: Magnetic Resonance Neurography (MRN) 13 PN-8: Amyotrophic Lateral Sclerosis (ALS) 14 PN-9: Peripheral Nerve Sheath Tumors (PNST) 15 PN-10: Nuclear Imaging 16 ______________________________________________________________________________________________________