Hyperglycemia and Renin-Dependent Hypertension Synergize to Model Diabetic Nephropathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Phylogenetic Screening for Possible Novel
11 M060072591U NORTH-WEST UNIVERSITY tilt• YUNIBESITI YA BOKONE•BOPHIRIMA NOOROVVE S-UNIVERSITEIT PHYLOGENETIC SCREENING FOR POSSIBLE NOVEL ANTIBIOTIC PRODUCING ACTINOMYCETES FROM RHIZOSPHERIC SOIL SAMPLES COLLECTED FROM NGAKA MODIRI MOLEMA DISTRICT IN NORTH WEST PROVINCE, SOUTH AFRICA I BY MOBOLAJI FELICIA ADEGBOYE A thesis submitted in fulfilment of the requirements for the degree of DOCTOR OF PHILOSOPHY (BIOLOGY) DEPARTMENT OF BIOLOGICAL SCIENCES FACULTY OF SCIENCE, AGRICULTURE AND TECHNOLOGY NORTH-WEST UNIVERSITY, MAFIKENG CAMPUS SOUTH AFRICA Supervisor: Professor Olubukola 0. Babalola 2014 LIBRARY o MAFIKENG CAMPUS CALL NO.: 2021 -02- 0 4 DECLARATION I, the undersigned, declare that this thesis submitted to the North-West University for the degree of Doctor of Philosophy in Biology in the Faculty of Science, Agriculture and Technology, School of Environmental and Health Sciences, and the work contained herein is my original work with exemption to the citations and that this work has not been submitted at any other University in partial or entirely for the award of any degree. Name: Mobolaji Felicia Adegboye Signature: .....~ •·· ··· ····· ·· .. ··············· ..... Date: .... ~S.. .. ....a~ ·1·· ·'.}Q~i; ... ............ .... DEDICATION This work is dedicated to Almighty God for His faithfulness over my life and for making my helpers to be many. ii ACKNOWLEDGEMENTS I would like to express my deepest thanks, gratitude and appreciation to my supervisor and mentor, Prof. Olubukola 0. Babalola for giving me the opportunity to pursue my doctoral degree under her supervision and for her encouragement, help and kind support. Her invaluable advice, suggestions, discussions and guidance were a real support to me. I acknowledge with honour and gratitude the International Foundation for Science (IFS) for research grant (F/5330-1 ), Connect Africa Scholarship Award, H3ABioNet/SANBio Scholarship and North-West University for offering me bursary/scholarship award to pursue the PhD degree. -

Age-Dependent Myocardial Transcriptomic Changes in the Rat
Revista Română de Medicină de Laborator Vol. 22, Nr. 1, Martie, 2014 9 Research article DOI: 10.2478/rrlm-2014-0001 Age-dependent myocardial transcriptomic changes in the rat. Novel insights into atrial and ventricular arrhythmias pathogenesis Modificări transcriptomice dependente de vârstă în miocardul de șobolan. Noi aspecte referitoare la patogeneza aritmiilor atriale și ventriculare Alina Scridon1,2, Emmanuelle Fouilloux-Meugnier3, Emmanuelle Loizon3, Marcel Perian1, Sophie Rome3, Claude Julien2, Christian Barrès2, Philippe Chevalier2,4 1.Physiology Department, University of Medicine and Pharmacy of Tîrgu Mureș, 540139, Tîrgu Mureș, Romania 2. Unité de Neurocardiologie, EA4612, Université Lyon 1, F-69008, Lyon, France 3. Unité 1060 INSERM CarMen, Université Lyon 1, F-69008, Lyon, France 4. Hospices Civils de Lyon, Hôpital Louis Pradel, Service de Rythmologie, 69500, Bron, France Abstract Background: Aging is associated with significantly increased prevalence of cardiac arrhythmias, but tran- scriptional events that underlie this process remain to be established. To gain deeper insight into molecular mech- anisms of aging-related cardiac arrhythmias, we performed mRNA expression analysis comparing atrial and ven- tricular myocardium from Wistar-Kyoto (WKY) rats of different ages. Methods: Atrial and ventricular sampling was performed in 3 groups (n=4 each) of young (14-week-old), adult (25-week-old), and aging (47-week-old) WKY rats. mRNA expressions of 89 genes involved in cardiac arrhythmogenicity were investigated using TaqMan Low Density Array analysis. Results: Of the 89 studied genes, 40 and 64 genes presented steady atrial and ventricu- lar expressions, respectively. All genes differentially expressed within the atria of WKY rats were up-regulated with advancing age, mainly the genes encoding for various K+, Ca2+, Na+ channels, and type 6 collagen. -

The Mineralocorticoid Receptor Leads to Increased Expression of EGFR
www.nature.com/scientificreports OPEN The mineralocorticoid receptor leads to increased expression of EGFR and T‑type calcium channels that support HL‑1 cell hypertrophy Katharina Stroedecke1,2, Sandra Meinel1,2, Fritz Markwardt1, Udo Kloeckner1, Nicole Straetz1, Katja Quarch1, Barbara Schreier1, Michael Kopf1, Michael Gekle1 & Claudia Grossmann1* The EGF receptor (EGFR) has been extensively studied in tumor biology and recently a role in cardiovascular pathophysiology was suggested. The mineralocorticoid receptor (MR) is an important efector of the renin–angiotensin–aldosterone‑system and elicits pathophysiological efects in the cardiovascular system; however, the underlying molecular mechanisms are unclear. Our aim was to investigate the importance of EGFR for MR‑mediated cardiovascular pathophysiology because MR is known to induce EGFR expression. We identifed a SNP within the EGFR promoter that modulates MR‑induced EGFR expression. In RNA‑sequencing and qPCR experiments in heart tissue of EGFR KO and WT mice, changes in EGFR abundance led to diferential expression of cardiac ion channels, especially of the T‑type calcium channel CACNA1H. Accordingly, CACNA1H expression was increased in WT mice after in vivo MR activation by aldosterone but not in respective EGFR KO mice. Aldosterone‑ and EGF‑responsiveness of CACNA1H expression was confrmed in HL‑1 cells by Western blot and by measuring peak current density of T‑type calcium channels. Aldosterone‑induced CACNA1H protein expression could be abrogated by the EGFR inhibitor AG1478. Furthermore, inhibition of T‑type calcium channels with mibefradil or ML218 reduced diameter, volume and BNP levels in HL‑1 cells. In conclusion the MR regulates EGFR and CACNA1H expression, which has an efect on HL‑1 cell diameter, and the extent of this regulation seems to depend on the SNP‑216 (G/T) genotype. -

Exosomes Confer Chemoresistance to Pancreatic Cancer Cells By
FULL PAPER British Journal of Cancer (2017) 116, 609–619 | doi: 10.1038/bjc.2017.18 Keywords: chemoresistance; exosomes; pancreatic cancer; ROS; microRNA Exosomes confer chemoresistance to pancreatic cancer cells by promoting ROS detoxification and miR-155-mediated suppression of key gemcitabine-metabolising enzyme, DCK Girijesh Kumar Patel1, Mohammad Aslam Khan1, Arun Bhardwaj1, Sanjeev K Srivastava1, Haseeb Zubair1, Mary C Patton1, Seema Singh1,2, Moh’d Khushman3 and Ajay P Singh*,1,2 1Department of Oncologic Sciences, Mitchell Cancer Institute, University of South Alabama, Mobile, AL, USA; 2Department of Biochemistry and Molecular Biology, College of Medicine, University of South Alabama, Mobile, AL, USA and 3Department of Interdisciplinary Clinical Oncology, Mitchell Cancer Institute, University of South Alabama, Mobile, AL, USA Background: Chemoresistance is a significant clinical problem in pancreatic cancer (PC) and underlying molecular mechanisms still remain to be completely understood. Here we report a novel exosome-mediated mechanism of drug-induced acquired chemoresistance in PC cells. Methods: Differential ultracentrifugation was performed to isolate extracellular vesicles (EVs) based on their size from vehicle- or gemcitabine-treated PC cells. Extracellular vesicles size and subtypes were determined by dynamic light scattering and marker profiling, respectively. Gene expression was examined by qRT-PCR and/or immunoblot analyses, and direct targeting of DCK by miR-155 was confirmed by dual-luciferase 30-UTR reporter assay. Flow cytometry was performed to examine the apoptosis indices and reactive oxygen species (ROS) levels in PC cells using specific dyes. Cell viability was determined using the WST-1 assay. Results: Conditioned media (CM) from gemcitabine-treated PC cells (Gem-CM) provided significant chemoprotection to subsequent gemcitabine toxicity and most of the chemoresistance conferred by Gem-CM resulted from its EVs fraction. -

ADAM9: a Novel Player in Vestibular Schwannoma Pathogenesis
1856 ONCOLOGY LETTERS 19: 1856-1864, 2020 ADAM9: A novel player in vestibular schwannoma pathogenesis MARIA BREUN1, ALEXANDRA SCHWERDTFEGER1, DONATO DANIEL MARTELLOTTA1, ALMUTH F. KESSLER1, CAMELIA M. MONORANU2, CORDULA MATTHIES1, MARIO LÖHR1* and CARSTEN HAGEMANN1* 1Department of Neurosurgery, University Hospital Würzburg; 2Department of Neuropathology, Institute of Pathology, University of Würzburg, D-97080 Würzburg, Germany Received April 27, 2019; Accepted October 2, 2019 DOI: 10.3892/ol.2020.11299 Abstract. A disintegrin and metalloproteinase 9 (ADAM9) is VS samples (n=60). A total of 30 of them were from patients a member of the transmembrane ADAM family. It is expressed with neurofibromatosis. Healthy peripheral nerves from in different types of solid cancer and promotes tumor invasive- autopsies (n=10) served as controls. ADAM9 mRNA levels ness. To the best of our knowledge, the present study was the were measured by PCR, and protein levels were determined first to examine ADAM9 expression in vestibular schwan- by immunohistochemistry (IHC) and western blotting (WB). nomas (VS) from patients with and without neurofibromatosis The Hannover Classification was used to categorize tumor type 2 (NF2) and to associate the data with clinical parameters extension and hearing loss. ADAM9 mRNA levels were of the patients. The aim of the present study was to evaluate 8.8-fold higher in VS compared with in controls. The levels if ADAM9 could be used as prognostic marker or therapeutic were 5.6-fold higher in patients with NF2 and 12-fold higher in target. ADAM9 mRNA and protein levels were measured in patients with sporadic VS. WB revealed two mature isoforms of the protein, and according to IHC ADAM9 was mainly expressed by S100-positive Schwann cells. -

Importance of Β-APP, ADAM9, 10, 17 in Alzheimer Disease
Available online at www.ijmrhs.com al R edic ese M a of rc l h a & n r H u e o a J l l t h International Journal of Medical Research & a n S ISSN No: 2319-5886 o c i t i Health Sciences, 2019, 8(7): 68-7 e a n n c r e e t s n I • • I J M R H S Importance of β-APP, ADAM9, 10, 17 in Alzheimer Disease: Preliminary Autopsy Study with Immunohistochemical Expression in Human Brain Filiz Eren1, Nursel Turkmen Inanır1,2, Recep Fedakar2, Bulent Eren3*, Murat Serdar Gurses1, Mustafa Numan Ural4, Sumeyya Akyol5, Busra Aynekin5 and Kadir Demircan5 1 Bursa Morgue Department, Council of Forensic Medicine of Turkey, Bursa, Turkey 2 Department of Forensic Medicine, School of Medicine, Uludag University, Bursa, Turkey 5 3 Department of Forensic Medicine, School of Medicine, Tokat Gaziosmanpaşa University Tokat, Turkey 4 5 Bilgemed Work Safety and Security, Bursa, Turkey 5 Independent Researcher, Ankara, Turkey *Corresponding e-mail: [email protected] ABSTRACT Alzheimer’s disease (AD) is encountered as an important health problem. It was exposed that in the pathophysiology of AD, formation, and aggregation of amyloid β from amyloid precursor protein ( APP), was restrained by α-secretase group, ADAM (a disintegrin and metalloproteinase) enzymes. From this perspective, ADAM group of enzymes can be presumably used in the future both as a diagnostic marker, and potential treatment modality. In our study, 9 cases with or without AD in different age groups with various causes of death who were autopsied in the Bursa Morgue Department of the Council of Forensic Medicine of Turkey were included in the study. -
New PDF Document
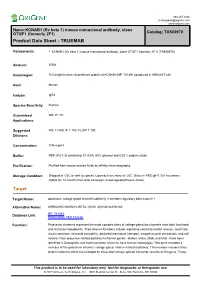
888.267.4436 [email protected] www.origene.com Name:KCNAB1 (Kv beta 1) mouse monoclonal antibody, clone OTI2F1 (formerly 2F1) Catalog: TA503970 Product Data Sheet - TRUEMAB Components: • KCNAB1 (Kv beta 1) mouse monoclonal antibody, clone OTI2F1 (formerly 2F1) (TA503970) Amount: 100ul Immunogen: Full length human recombinant protein of KCNAB1(NP_751891) produced in HEK293T cell. Host: Mouse Isotype: IgG1 Species Reactivity: Human Guaranteed WB, IF, FC Applications: Suggested WB 1:1000, IF 1:100, FLOW 1:100, Dilutions: Concentration: 0.96 mg/ml Buffer: PBS (PH 7.3) containing 1% BSA, 50% glycerol and 0.02% sodium azide. Purification: Purified from mouse ascites fluids by affinity chromatography Storage Condition: Shipped at -20C or with ice packs. Upon delivery store at -20C. Dilute in PBS (pH7.3) if necessary. Stable for 12 months from date of receipt. Avoid repeated freeze-thaws. Target Target Name: potassium voltage-gated channel subfamily A member regulatory beta subunit 1 Alternative Name: AKR6A3|KCNA1B|KV-BETA-1|Kvb1.3|hKvBeta3|hKvb3 Database Link: NP_751891 Entrez Gene 7881 Human Function: Potassium channels represent the most complex class of voltage-gated ion channels from both functional and structural standpoints. Their diverse functions include regulating neurotransmitter release, heart rate, insulin secretion, neuronal excitability, epithelial electrolyte transport, smooth muscle contraction, and cell volume. Four sequence-related potassium channel genes - shaker, shaw, shab, and shal - have been identified in Drosophila, and each has been shown to have human homolog(s). This gene encodes a member of the potassium channel, voltage-gated, shaker-related subfamily. This member includes three distinct isoforms which are encoded by three alternatively spliced transcript variants of this gene. -

Integrative Systems Biology– Renal Diseases: a Road to a Holist View of Chronic Disease Mechanism
Integrative Systems biology– Renal Diseases: A road to a holist view of chronic disease mechanism Matthias Kretzler Div. Nephrology / Internal Medicine Computational Medicine and Bioinformatics University of Michigan Medical School The challenge in chronic disease • Descriptive disease categorization with multiple pathogenetic mechanisms § Problems of ‘mixed bag’ diseases: • Unpredictable disease course and response to therapy • Nephrology as an ‘art of trial and error’ • Shift in our disease paradigms: § Mechanism based patient management • Define the disease process active in the individual patient – Base prognosis on specific disease process – Target therapy to interfere with the mechanism currently destroying endorgan function Molecular Nephrology approach Clinical outcome research Genetics Molecular Pathology Molecular Epigenetics Phenotyping Genomics Functional Clinical research Disease Genomics Biobanks Proteomics Model systems Animal models Molecular interaction In vitro tissue culture model systems Organ culture and development Tower of Babylon: Search for the universal language for the medicine of the 21st century Pieter Bruegl: 1563. Kunsthistorisches Museum Wien Molecular Nephrology approach Clinical outcome research Genetics Molecular Pathology Molecular Epigenetics Phenotyping Genomics Functional Clinical research Disease Genomics Integrative Biobanks Proteomics Biology (Physiology) Model systems Animal models Molecular interaction of renal disease In vitro tissue culture model systems Organ culture and development Systems -

The Chondrocyte Channelome: a Novel Ion Channel Candidate in the Pathogenesis of Pectus Deformities
Old Dominion University ODU Digital Commons Biological Sciences Theses & Dissertations Biological Sciences Summer 2017 The Chondrocyte Channelome: A Novel Ion Channel Candidate in the Pathogenesis of Pectus Deformities Anthony J. Asmar Old Dominion University, [email protected] Follow this and additional works at: https://digitalcommons.odu.edu/biology_etds Part of the Biology Commons, Molecular Biology Commons, and the Physiology Commons Recommended Citation Asmar, Anthony J.. "The Chondrocyte Channelome: A Novel Ion Channel Candidate in the Pathogenesis of Pectus Deformities" (2017). Doctor of Philosophy (PhD), Dissertation, Biological Sciences, Old Dominion University, DOI: 10.25777/pyha-7838 https://digitalcommons.odu.edu/biology_etds/19 This Dissertation is brought to you for free and open access by the Biological Sciences at ODU Digital Commons. It has been accepted for inclusion in Biological Sciences Theses & Dissertations by an authorized administrator of ODU Digital Commons. For more information, please contact [email protected]. THE CHONDROCYTE CHANNELOME: A NOVEL ION CHANNEL CANDIDATE IN THE PATHOGENESIS OF PECTUS DEFORMITIES by Anthony J. Asmar B.S. Biology May 2010, Virginia Polytechnic Institute M.S. Biology May 2013, Old Dominion University A Dissertation Submitted to the Faculty of Old Dominion University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY BIOMEDICAL SCIENCES OLD DOMINION UNIVERSITY August 2017 Approved by: Christopher Osgood (Co-Director) Michael Stacey (Co-Director) Lesley Greene (Member) Andrei Pakhomov (Member) Jing He (Member) ABSTRACT THE CHONDROCYTE CHANNELOME: A NOVEL ION CHANNEL CANDIDATE IN THE PATHOGENESIS OF PECTUS DEFORMITIES Anthony J. Asmar Old Dominion University, 2017 Co-Directors: Dr. Christopher Osgood Dr. Michael Stacey Costal cartilage is a type of rod-like hyaline cartilage connecting the ribs to the sternum. -

The Positive Side of Proteolysis in Alzheimer's Disease
Hindawi Publishing Corporation Biochemistry Research International Volume 2011, Article ID 721463, 13 pages doi:10.1155/2011/721463 Review Article Zinc Metalloproteinases and Amyloid Beta-Peptide Metabolism: The Positive Side of Proteolysis in Alzheimer’s Disease Mallory Gough, Catherine Parr-Sturgess, and Edward Parkin Division of Biomedical and Life Sciences, School of Health and Medicine, Lancaster University, Lancaster LA1 4YQ, UK Correspondence should be addressed to Edward Parkin, [email protected] Received 17 August 2010; Accepted 7 September 2010 Academic Editor: Simon J. Morley Copyright © 2011 Mallory Gough et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Alzheimer’s disease is a neurodegenerative condition characterized by an accumulation of toxic amyloid beta- (Aβ-)peptides in the brain causing progressive neuronal death. Aβ-peptides are produced by aspartyl proteinase-mediated cleavage of the larger amyloid precursor protein (APP). In contrast to this detrimental “amyloidogenic” form of proteolysis, a range of zinc metalloproteinases can process APP via an alternative “nonamyloidogenic” pathway in which the protein is cleaved within its Aβ region thereby precluding the formation of intact Aβ-peptides. In addition, other members of the zinc metalloproteinase family can degrade preformed Aβ-peptides. As such, the zinc metalloproteinases, collectively, are key to downregulating Aβ generation and enhancing its degradation. It is the role of zinc metalloproteinases in this “positive side of proteolysis in Alzheimer’s disease” that is discussed in the current paper. 1. Introduction of 38–43 amino acid peptides called amyloid beta (Aβ)- peptides. -

Genome-Wide Mega-Analysis Identifies 16 Loci and Highlights Diverse Biological Mechanisms in the Common Epilepsies." (2018)
Follow this and additional works at: https://jdc.jefferson.edu/neurologyfp Part of the Neurology Commons Let us know how access to this document benefits ouy Recommended Citation Abou-Khalil, Bassel; Auce, Pauls; Avbersek, Andreja; Bahlo, Melanie; ThomasBalding, JeffDaviderson J.; Bast, Univ ersity Thomas; Baum, Larry; Becker, Albert J.; Becker, Felicitas;Jeff Berghuis,erson Bianca; Digital Berkovic, Commons Samuel F.; Boysen, Katja E.; Bradfield, Jonathan .;P Brody, Lawrence C.; Buono, Russell J.; Campbell, Ellen; Cascino, Gregory D.; Catarino, Claudia B.; Cavalleri, Gianpiero L.; Cherny, Stacey S.; Chinthapalli, Krishna;Department Coff ofey Neur, Alisonology J.; CompstFaculty Pon,apers Alastair; Coppola, Antonietta; Cossette,Depar Ptmentatrick; of Cr Neuraig, ologyJohn J.; de Haan, Gerrit-Jan; De Jonghe, Peter; de Kovel, Carolien G.F.; Delanty, Norman; Depondt, 12-10-2018Chantal; De vinsky, Orrin; Dlugos, Dennis J.; Doherty, Colin P.; Elger, Christian E.; Eriksson, Johan G.; Ferraro, Thomas N.; Feuch, Martha; Francis, Ben; Franke, Andre; French, Jacqueline A.; Genome-wideFreytag, Saskia; Gaus, mega-analysis Verena; Geller, Eric B.; identifies Gieger, Christian; 16 Glauserloci and, Tracy; highlights Glynn, Simon; Goldstein, David B.; Gui, Hongsheng; Guo, Youling; Haas, Kevin F.; Hakonarson, Hakon; Hallmann, Kdiverstin;erse Haut, biological Sheryl; Heinz mechanismsen, Erin L.; Helbig, Ingo; in the Hengsbach, common Christian; epilepsies. Hjalgrim, Helle; BasselIacomino, Abou-Khalil Michele; Ingason, Andrés; Jamnadas-Khoda, Jennifer; Johnson, -

Zinc Metalloproteinases and Amyloid Beta-Peptide Metabolism: the Positive Side of Proteolysis in Alzheimer’S Disease
Hindawi Publishing Corporation Biochemistry Research International Volume 2011, Article ID 721463, 13 pages doi:10.1155/2011/721463 Review Article Zinc Metalloproteinases and Amyloid Beta-Peptide Metabolism: The Positive Side of Proteolysis in Alzheimer’s Disease Mallory Gough, Catherine Parr-Sturgess, and Edward Parkin Division of Biomedical and Life Sciences, School of Health and Medicine, Lancaster University, Lancaster LA1 4YQ, UK Correspondence should be addressed to Edward Parkin, [email protected] Received 17 August 2010; Accepted 7 September 2010 Academic Editor: Simon J. Morley Copyright © 2011 Mallory Gough et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Alzheimer’s disease is a neurodegenerative condition characterized by an accumulation of toxic amyloid beta- (Aβ-)peptides in the brain causing progressive neuronal death. Aβ-peptides are produced by aspartyl proteinase-mediated cleavage of the larger amyloid precursor protein (APP). In contrast to this detrimental “amyloidogenic” form of proteolysis, a range of zinc metalloproteinases can process APP via an alternative “nonamyloidogenic” pathway in which the protein is cleaved within its Aβ region thereby precluding the formation of intact Aβ-peptides. In addition, other members of the zinc metalloproteinase family can degrade preformed Aβ-peptides. As such, the zinc metalloproteinases, collectively, are key to downregulating Aβ generation and enhancing its degradation. It is the role of zinc metalloproteinases in this “positive side of proteolysis in Alzheimer’s disease” that is discussed in the current paper. 1. Introduction of 38–43 amino acid peptides called amyloid beta (Aβ)- peptides.