Common Injuries of the Foot and Ankle in the Child and Adolescent Athlete Gerard A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Volume 15, Issue 1, January-April
Volume 15, Issue 1, January-April Osteochondral lesions of the talus in adults J. Batista, G. Joannas, L. Casola, L. Logioco, G. Arrondo 1A Traumatic lesion with isolated cartilage injury (flap) Tx: arthroscopy, curettage, and microfractures. 1B Traumatic lesion (cartilage and subchondral bone injury) 1B.1 Lesion <10mm in diameter and <5mm of depth (superficial lesion) Tx: arthroscopy, curettage, and microfractures. 1B.2 Lesion >10mm in diameter and >5mm in depth Tx: fragment fixation with osteosynthesis, open surgery, osteochondral graft, or mosaicoplasty. 2A Non-traumatic isolated bone injury, subchondral cyst. Tx: retrograde drilling. 2B Non-traumatic open subchondral bone cyst with articular connection (progression of type 2A). 2B.1 Lesion measuring <10mm in diameter and <5mm in depth (superficial lesion). Tx: arthroscopy, curettage, and microfractures. 2B.2 Lesion measuring >10mm in diameter and >5mm in depth. Tx: open surgery, osteochondral graft, or mosaicoplasty. 3 Type 1 or 2 lesions associated with lateral instability of the ankle Tx: ligament repair. 4 With limb deformities 4A Types 1 or 2 lesions with hindfoot deformity = varus or valgus calcaneus Tx: varus or valgus calcaneal osteotomy. 4B Type 1 or 2 lesion with supramalleolar deformity of distal tibia (varus or valgus) Tx: varus or valgus supramalleolar osteotomy. Tx: treatment. Volume 15, Issue 1, January-April The Journal of the Foot & Ankle (eISSN 2675-2980) is published quarterly in April, August, and December, with the purpose of disseminating papers on themes of Foot and Ankle Medicine and Surgery and related areas. The Journal offers free and open access to your content on our website. All papers are already published with active DOIs. -

Anterior Reconstruction Techniques for Cervical Spine Deformity
Neurospine 2020;17(3):534-542. Neurospine https://doi.org/10.14245/ns.2040380.190 pISSN 2586-6583 eISSN 2586-6591 Review Article Anterior Reconstruction Techniques Corresponding Author for Cervical Spine Deformity Samuel K. Cho 1,2 1 1 1 https://orcid.org/0000-0001-7511-2486 Murray Echt , Christopher Mikhail , Steven J. Girdler , Samuel K. Cho 1Department of Orthopedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA Department of Orthopaedics, Icahn 2 Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, School of Medicine at Mount Sinai, 425 NY, USA West 59th Street, 5th Floor, New York, NY, USA E-mail: [email protected] Cervical spine deformity is an uncommon yet severely debilitating condition marked by its heterogeneity. Anterior reconstruction techniques represent a familiar approach with a range Received: June 24, 2020 of invasiveness and correction potential—including global or focal realignment in the sagit- Revised: August 5, 2020 tal and coronal planes. Meticulous preoperative planning is required to improve or prevent Accepted: August 17, 2020 neurologic deterioration and obtain satisfactory global spinal harmony. The ability to per- form anterior only reconstruction requires mobility of the opposite column to achieve cor- rection, unless a combined approach is planned. Anterior cervical discectomy and fusion has limited focal correction, but when applied over multiple levels there is a cumulative ef- fect with a correction of approximately 6° per level. Partial or complete corpectomy has the ability to correct sagittal deformity as well as decompress the spinal canal when there is an- terior compression behind the vertebral body. -

Original Article Pictorial Atlas of Symptomatic Accessory Ossicles by 18F-Sodium Fluoride (Naf) PET-CT
Am J Nucl Med Mol Imaging 2017;7(6):275-282 www.ajnmmi.us /ISSN:2160-8407/ajnmmi0069278 Original Article Pictorial atlas of symptomatic accessory ossicles by 18F-Sodium Fluoride (NaF) PET-CT Sharjeel Usmani1, Cherry Sit2, Gopinath Gnanasegaran2, Tim Van den Wyngaert3, Fahad Marafi4 1Department of Nuclear Medicine & PET/CT Imaging, Kuwait Cancer Control Center, Khaitan, Kuwait; 2Royal Free Hospital NHS Trust, London, UK; 3Antwerp University Hospital, Belgium; 4Jaber Al-Ahmad Molecular Imaging Center, Kuwait Received August 7, 2017; Accepted December 15, 2017; Epub December 20, 2017; Published December 30, 2017 Abstract: Accessory ossicles are developmental variants which are often asymptomatic. When incidentally picked up on imaging, they are often inconsequential and rarely a cause for concern. However, they may cause pain or discomfort due to trauma, altered stress, and over-activity. Nuclear scintigraphy may play a role in the diagnosis and localizing pain generators. 18F-Sodium Fluoride (NaF) is a PET imaging agent used in bone imaging. Although commonly used in imaging patients with cancer imaging malignancy, 18F-NaF may be useful in the evaluation of benign bone and joint conditions. In this article, we would like to present a spectrum of clinical cases and review the potential diagnostic utility of 18F-NaF in the assessment of symptomatic accessory ossicles in patients referred for staging cancers. Keywords: 18F-NaF PET/CT, accessory ossicles, hybrid imaging Introduction Accessory ossicles are developmental variants which are often asymptomatic. When inciden- Bone and joint pain is a common presentation tally picked up on imaging, they are often incon- in both primary and secondary practice. -
Subtalar Joint Version 1.0 Effective June 15, 2021
CLINICAL GUIDELINES CMM-407: Arthroscopy: Subtalar Joint Version 1.0 Effective June 15, 2021 Clinical guidelines for medical necessity review of Comprehensive Musculoskeletal Management Services. © 2021 eviCore healthcare. All rights reserved. Comprehensive Musculoskeletal Management Guidelines V1.0 CMM-407: Arthroscopy: Subtalar Joint Definitions 3 General Guidelines 3 Indications 4 Non-Indications 5 Procedure (CPT®) Codes 5 References 6 ______________________________________________________________________________________________________ ©2021 eviCore healthcare. All Rights Reserved. Page 2 of 6 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Comprehensive Musculoskeletal Management Guidelines V1.0 Definitions Red flags indicate comorbidities that require urgent/emergent diagnostic imaging and/or referral for definitive therapy. Clinically meaningful improvement is defined as at least 50% improvement noted on global assessment. General Guidelines Either of the following are considered red flag conditions for subtalar joint arthroscopy: Post-reduction evaluation and management of the subtalar dislocation Septic arthritis in the subtalar joint Although imaging may be normal, prior to subtalar joint arthroscopy, radiographic imaging should be performed and include both of the following: Plain X-rays with one or more views (anteroposterior, lateral, axial, and/or Broden’s) to confirm and differentiate any of the following: Degenerative joint changes Loose bodies Osteochondral lesions Impingement -

In Patients with End-Stage Ankle Arthritis, How Does Total Ankle Arthroplasty Compared to Arthrodesis Affect Ankle Pain and Function?
University of the Pacific Scholarly Commons Physician's Assistant Program Capstones School of Health Sciences 4-1-2020 In Patients with End-Stage Ankle Arthritis, How Does Total Ankle Arthroplasty Compared to Arthrodesis Affect Ankle Pain and Function? Zachary Whipple University of the Pacific, [email protected] Follow this and additional works at: https://scholarlycommons.pacific.edu/pa-capstones Part of the Medicine and Health Sciences Commons Recommended Citation Whipple, Zachary, "In Patients with End-Stage Ankle Arthritis, How Does Total Ankle Arthroplasty Compared to Arthrodesis Affect Ankle Pain and Function?" (2020). Physician's Assistant Program Capstones. 84. https://scholarlycommons.pacific.edu/pa-capstones/84 This Capstone is brought to you for free and open access by the School of Health Sciences at Scholarly Commons. It has been accepted for inclusion in Physician's Assistant Program Capstones by an authorized administrator of Scholarly Commons. For more information, please contact [email protected]. In Patients with End-Stage Ankle Arthritis, How Does Total Ankle Arthroplasty Compared to Arthrodesis Affect Ankle Pain and Function? By Zachary Whipple Capstone Project Submitted to the Faculty of the Department of Physician Assistant Education of the University of the Pacific in partial fulfilment of the requirements for the degree of MASTER OF PHYSICIAN ASSISTANT STUDIES April 2020 Introduction End-stage ankle arthritis is a debilitating degenerative disease commonly located at the tibiotalar joint. The prevalence of symptomatic arthritis is about nine times lower than the rates associated with those of the knee or hip.1 Though less common than knee and hip arthritis, the US estimates greater than 50,000 new cases are reported each year.2 The most common etiology of ankle arthritis is post-traumatic pathology. -
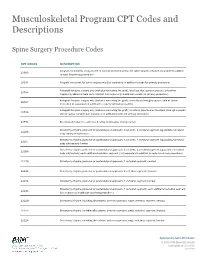
Musculoskeletal Program CPT Codes and Descriptions
Musculoskeletal Program CPT Codes and Descriptions Spine Surgery Procedure Codes CPT CODES DESCRIPTION Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition 20930 to code for primary procedure) 20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar 20936 fragments) obtained from same incision (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial 20937 incision) (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate 20938 skin or fascial incision) (List separately in addition to code for primary procedure) 20974 Electrical stimulation to aid bone healing; noninvasive (nonoperative) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22206 body subtraction); thoracic Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22207 body subtraction); lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22208 body subtraction); each additional vertebral segment (List separately in addition to code for -

Differences Between Subtotal Corpectomy and Laminoplasty for Cervical Spondylotic Myelopathy
Spinal Cord (2010) 48, 214–220 & 2010 International Spinal Cord Society All rights reserved 1362-4393/10 $32.00 www.nature.com/sc ORIGINAL ARTICLE Differences between subtotal corpectomy and laminoplasty for cervical spondylotic myelopathy S Shibuya1, S Komatsubara1, S Oka2, Y Kanda1, N Arima1 and T Yamamoto1 1Department of Orthopaedic Surgery, School of Medicine, Kagawa University, Kagawa, Japan and 2Oka Orthopaedic and Rehabilitation Clinic, Kagawa, Japan Objective: This study aimed to obtain guidelines for choosing between subtotal corpectomy (SC) and laminoplasty (LP) by analysing the surgical outcomes, radiological changes and problems associated with each surgical modality. Study Design: A retrospective analysis of two interventional case series. Setting: Department of Orthopaedic Surgery, Kagawa University, Japan. Methods: Subjects comprised 34 patients who underwent SC and 49 patients who underwent LP. SC was performed by high-speed drilling to remove vertebral bodies. Autologous strut bone grafting was used. LP was performed as an expansive open-door LP. The level of decompression was from C3 to C7. Clinical evaluations included recovery rate (RR), frequency of C5 root palsy after surgery, re-operation and axial pain. Radiographic assessments included sagittal cervical alignment and bone union. Results: Comparisons between the two groups showed no significant differences in age at surgery, preoperative factors, RR and frequency of C5 palsy. Progression of kyphotic changes, operation time and volumes of blood loss and blood transfusion were significantly greater in the SC (two- or three- level) group. Six patients in the SC group required additional surgery because of pseudoarthrosis, and four patients underwent re-operation because of adjacent level disc degeneration. -

Procedure Coding in ICD-9-CM and ICD- 10-PCS
Procedure Coding in ICD-9-CM and ICD- 10-PCS ICD-9-CM Volume 3 Procedures are classified in volume 3 of ICD-9-CM, and this section includes both an Alphabetic Index and a Tabular List. This volume follows the same format, organization and conventions as the classification of diseases in volumes 1 and 2. ICD-10-PCS ICD-10-PCS will replace volume 3 of ICD-9-CM. Unlike ICD-10-CM for diagnoses, which is similar in structure and format as the ICD-9-CM volumes 1 and 2, ICD-10-PCS is a completely different system. ICD-10-PCS has a multiaxial seven-character alphanumeric code structure providing unique codes for procedures. The table below gives a brief side-by-side comparison of ICD-9-CM and ICD-10-PCS. ICD-9-CM Volume3 ICD-10-PCS Follows ICD structure (designed for diagnosis Designed and developed to meet healthcare coding) needs for a procedure code system Codes available as a fixed or finite set in list form Codes constructed from flexible code components (values) using tables Codes are numeric Codes are alphanumeric Codes are 3-4 digits long All codes are seven characters long ICD-9-CM and ICD-10-PCS are used to code only hospital inpatient procedures. Hospital outpatient departments, other ambulatory facilities, and physician practices are required to use CPT and HCPCS to report procedures. ICD-9-CM Conventions in Volume 3 Code Also In volume 3, the phrase “code also” is a reminder to code additional procedures only when they have actually been performed. -

Knee Arthrodesis After Failed Total Knee Arthroplasty
650 COPYRIGHT Ó 2019 BY THE JOURNAL OF BONE AND JOINT SURGERY,INCORPORATED Current Concepts Review Knee Arthrodesis After Failed Total 04/12/2019 on 1mhtSo9F6TkBmpGAR5GLp6FT3v73JgoS8Zn360/N4fAEQXu6c15Knc+cXP2J5+wvbQY2nVcoOF2DIk3Zd0BSqmOXRD8WUDFCPOJ9CnEHMNOmtIbs3S0ykA== by http://journals.lww.com/jbjsjournal from Downloaded Knee Arthroplasty Downloaded Asim M. Makhdom, MD, MSc, FRCSC, Austin Fragomen, MD, and S. Robert Rozbruch, MD from http://journals.lww.com/jbjsjournal Investigation performed at the Hospital for Special Surgery, Weill Cornell Medicine, Cornell University, New York, NY ä Knee arthrodesis after failure of a total knee arthroplasty (TKA) because of periprosthetic joint infection (PJI) may provide superior functional outcome and ambulatory status compared with above-the-knee amputation. by 1mhtSo9F6TkBmpGAR5GLp6FT3v73JgoS8Zn360/N4fAEQXu6c15Knc+cXP2J5+wvbQY2nVcoOF2DIk3Zd0BSqmOXRD8WUDFCPOJ9CnEHMNOmtIbs3S0ykA== ä The use of an intramedullary nail (IMN) for knee arthrodesis following removal of TKA components because of a PJI may result in higher fusion rates compared with external fixation devices. ä The emerging role of the antibiotic cement-coated interlocking IMN may expand the indications to achieve knee fusion in a single-stage intervention. ä Massive bone defects after failure of an infected TKA can be managed with various surgical strategies in a single- stage intervention to preserve leg length and function. Primary total knee arthroplasty (TKA) is a common procedure suppressive antibiotics for recurrent PJIs are generally reserved with a reported increase of 162% from 1991 to 2010 in the for patients with more severe preoperative disability and United States1,2. From 2005 to 2030, it is projected that the medical comorbidity and those who are not candidates to number of TKA procedures will grow by 673% or 3.5 million. -

Foot and Ankle Systems Coding Reference Guide
Foot and Ankle Systems Coding Reference Guide Physician CPT® Code Description Arthrodesis 27870 Arthrodesis, ankle, open 27871 Arthrodesis, tibiofibular joint, proximal or distal 28705 Arthrodesis; pantalar 28715 Arthrodesis; triple 28725 Arthrodesis; subtalar 28730 Arthrodesis, midtarsal or tarsometatarsal, multiple or transverse 28735 Arthrodesis, midtarsal or tarsometatarsal, multiple or transverse; with osteotomy (eg, flatfoot correction) 28737 Arthrodesis, with tendon lengthening and advancement, midtarsal, tarsal navicular-cuneiform (eg, miller type procedure) 28740 Arthrodesis, midtarsal or tarsometatarsal, single joint 28750 Arthrodesis, great toe; metatarsophalangeal joint 28755 Arthrodesis, great toe; interphalangeal joint 28760 Arthrodesis, with extensor hallucis longus transfer to first metatarsal neck, great toe, interphalangeal joint (eg, jones type procedure) Bunionectomy 28292 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with resection of proximal phalanx base, when performed, any method 28295 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with proximal metatarsal osteotomy, any method 28296 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with distal metatarsal osteotomy, any method 28297 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with first metatarsal and medial cuneiform joint arthrodesis, any method 28298 Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with -

The Skeletal System
Essentials of Human Anatomy & Physiology Seventh Edition Foundation • Physical Foundation of the Body The Skeletal System – 206 Bones • Osteology – science of the anatomy, structure, and function of bones – “Os” means Bone • With the exception of teeth, bone IS the hardest substance in the body Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings The Skeletal System • Parts of the skeletal system • Bones (skeleton) • Joints • Cartilages • Ligaments (bone to bone)(tendon=bone to muscle) • Divided into two divisions • Axial skeleton • Copyright © 2003Appendicular Pearson Education, Inc. publishing as Benjaminskeleton Cummings – limbs and girdle 1 Functions of Bones Bones of the Human Body • The skeleton has 206 bones • Support of the body • Two basic types of bone tissue • Protection of soft organs • Compact bone • Movement due to attached skeletal • Homogeneous muscles • Spongy bone • Storage of minerals and fats (K, Mg, • Small needle-like pieces of bone Na) Figure 5.2b • Many open spaces • Blood cell formation (White and Red) Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Classification of Bones Classification of Bones • Long bones • Short bones • Typically longer than wide • Generally cube-shape • Have a shaft with heads at both ends • Contain mostly spongy bone • Contain mostly compact bone •Examples: Carpals, tarsals • Examples: Femur, humerus Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings 2 Classification of Bones on the Classification of Bones Basis of Shape • Flat bones • Thin and flattened • Usually curved • Thin layers of compact bone around a layer of spongy bone •Examples: Skull, ribs, sternum Figure 5.1 Copyright © 2003 Pearson Education, Inc. -

Osteotomy Around the Knee: Evolution, Principles and Results
Knee Surg Sports Traumatol Arthrosc DOI 10.1007/s00167-012-2206-0 KNEE Osteotomy around the knee: evolution, principles and results J. O. Smith • A. J. Wilson • N. P. Thomas Received: 8 June 2012 / Accepted: 3 September 2012 Ó Springer-Verlag 2012 Abstract to other complex joint surface and meniscal cartilage Purpose This article summarises the history and evolu- surgery. tion of osteotomy around the knee, examining the changes Level of evidence V. in principles, operative technique and results over three distinct periods: Historical (pre 1940), Modern Early Years Keywords Tibia Osteotomy Knee Evolution Á Á Á Á (1940–2000) and Modern Later Years (2000–Present). We History Results Principles Á Á aim to place the technique in historical context and to demonstrate its evolution into a validated procedure with beneficial outcomes whose use can be justified for specific Introduction indications. Materials and methods A thorough literature review was The concept of osteotomy for the treatment of limb defor- performed to identify the important steps in the develop- mity has been in existence for more than 2,000 years, and ment of osteotomy around the knee. more recently pain has become an additional indication. Results The indications and surgical technique for knee The basic principle of osteotomy (osteo = bone, tomy = osteotomy have never been standardised, and historically, cut) is to induce a surgical transection of a bone to allow the results were unpredictable and at times poor. These realignment and a consequent transfer of weight bearing factors, combined with the success of knee arthroplasty from a damaged area to an undamaged area of joint surface.