Central Venous Catheter Placement: Modified Seldinger Technique
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Central Venous Catheters Insertion – Assisting
Policies & Procedures Title:: CENTRAL VENOUS CATHETERS INSERTION – ASSISTING LPN / RN: Entry Level Competency I.D. Number: 1073 Authorization Source: Nursing Cross Index: [] Pharmacy Nursing Committee Date Revised: February 2018 [] MAC Motion #: Date Effective: March, 1997 [x] Former SHtnHR Nursing Practice Scope: SKtnHR Acute Care Committee Any PRINTED version of this document is only accurate up to the date of printing 13-May-19. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. HIGH ALERT: Central line-associated bloodstream infection (CLABSI) continues to be one of the most deadly and costly hospital-associated infections. – Institute for Healthcare Improvement DEFINITIONS Central Venous Catheter (CVC) - A venous access device whose tip dwells in a great vessel. Central Line Associated Blood Stream Infection (CLABSI)- is a primary blood stream infection (BSI) in a patient that had a central line within the 48-hour period before the development of a BSI and is not bloodstream related to an infection at another site. 1. PURPOSE 1.1 To minimize the risks of central line-associated bloodstream infections and other complications associated with the insertion of central venous catheters. 2. POLICY 2.1 This policy applies to insertion of all central venous catheters (CVCs). 2.2 All licensed staff assisting with the insertion of CVCs will be educated in CVC care and prevention of CLABSI. -
Central Venous Access with Accelerated Seldinger Technique Versus Modified Seldinger Technique
Central Venous Access with Accelerated Seldinger Technique versus Modified Seldinger Technique L A N E THAUT , D O , CAPT , M C , USAF SAN ANTONIO MILITARY MEDICAL CENTER CO- AUTHORS: WELLS WEYMOUTH, MD, DANIEL RESCHKE, MD, BRANDEN HUNSAKER,MD Disclosures Expired POWERWAND™ combination device kits were donated by Access Scientific for the express purpose to be used in this study; however, no other contributions were made. We approached Access Scientific to obtain the devices to conduct this study. No financial relationship with Access Scientific. Background Techniques Research and Outcomes Questions Background Air Force SAMMC San Antonio, TX Level 1 Trauma Center 85,000+ patients annually Central Access Common Procedure Approximately 8% of hospitalized patients Multiple indications Large volume fluid or blood product resuscitation Administration of central acting medications Multiple medications simultaneously Trans venous pacing Difficult peripheral access Quick Story What if there was a simpler/quicker way? Intra-osseous? Complications Slower Flow Rate Labs Traditional Central Line Multiple steps/parts Midlines Usually used for extended dwelling lines. Self contained, all in one device. Equivalent and sometimes superior flow rate. Question Will the use of combination devices (midline/POWERWAND™) and the associated accelerated technique reduce the time of CVC placement? VS What is Accelerated Seldinger Technique? Needle, guidewire, dilator, and sheath into one. The device needle is inserted into the target vein under ultrasound guidance and a flash is observed The internal guidewire is then advanced into the vein and snapped into the needle hub. Dilator collar is turned and the dilator and sheath are advanced The dilator hub is disengaged from the needle hub, and the guidewire, dilator, and needle are all removed as a single unit. -

Intubation Through a Laryngeal Mask Airway by Fiberoptic Bronchoscope in an Infant with a Mass at the Base of the Tongue − a Case Report −
대한마취과학회지 2008; 54: S 43~6 □ 영문논문 □ Korean J Anesthesiol Vol. 54, No. 3, March, 2008 Intubation through a Laryngeal Mask Airway by Fiberoptic Bronchoscope in an Infant with a Mass at the Base of the Tongue − A case report − Department of Anesthesiology and Pain Medicine, Anesthesiology and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea Ji Eun Kim, M.D., Chul Ho Chang, M.D., and Yong-Taek Nam, M.D. Failed or difficult tracheal intubation remains an important cause of mortality and morbidity during anesthesia, especially in infants with anatomical or pathological abnormalities of the airway. We report on a 4.1 kg, 85-day-male infant with a thyroglossal duct cyst at the tongue base who could not be conventionally ventilated and intubated in the supine position. The infant was intubated with a 3-mm endotracheal tube through the laryngeal mask airway (LMA) with guidance of a fiberoptic bronchoscope (FOB). However, the pilot balloon did not pass through the 1.5-mm LMA conduit. After cutting the pilot balloon, we removed the LMA and inserted a central venous catheter guide-wire through the endotracheal tube to increase the endotracheal tube to 3.5 mm. This maneuver allowed us to secure the airway without further problems. (Korean J Anesthesiol 2008; 54: S 43~6) Key Words: fiberoptic bronchoscope, infant, intubation, laryngeal mask airway, thyroglossal duct cyst. Failed or difficult tracheal intubation is an important cause conventional laryngoscopy.8) of mortality and morbidity during anesthesia.1-3) Difficulties are In the present report, we describe the successful intubation more frequent in pediatric patients because of their anatomical with LMA and FOB under the aid of central venous catheter variations.4) Tracheal intubation of infants with various anato- guide wire in a 4.1 kg, 85-day-male infant, who could not be mical and pathological abnormalities of the airway can be a conventionally ventilated and intubated. -

The Nurses Group Poster Session
THE NURSES GROUP POSTER SESSION NP001 This abstract outlines the development and testing of an Family members’ experiences of different caring education program for family carers of individuals about to organizations during allogeneic hematopoietic stem cells undergo BMT. The project aimed to increase carer confidence transplantation - A qualitative interview study in supporting newly discharged blood and marrow transplant K. Bergkvist1,*, J. Larsen2, U.-B. Johansson1, J. Mattsson3, (BMT) recipients through an interactive education program. B. Fossum1 Method: Evaluation methodology was used to examine the 1 2 impact on carer confidence. Brief questionnaires to assess level Sophiahemmet University, Red Cross University College, fi 3Oncology and Pathology, Karolinska Institutet, Stockholm, of con dence were implemented pre- and post- each session; fi Sweden questions were speci c to the content of that session. Following completion of the program an overall evaluation Introduction: Home care after allogeneic hematopoietic stem survey was also completed. The education sessions were developed drawing on evidence from literature, unit specific cell transplantation (HSCT) has been an option for over ’ 15 years. Earlier studies have shown that home care is safe practice guidelines and the team s expertise. Carers of and has medical advantages. Because of the complex and individuals who were about to receive, or currently receiving intensive nature of the HSCT, most patients require a family BMT, were invited to attend the education program. member to assist them with their daily living. Today, there is a Completing the evaluation was not a program requirement. limited knowledge about family members’ experiences in Results: Up to 14 carers attended each session. -

Practice Parameter for the Use of Ultrasound to Guide Vascular Access Procedures
PRACTICE GUIDELINES AIUM Practice Parameter for the Use of Ultrasound to Guide Vascular Access Procedures I. Introduction he clinical aspects of this parameter were developed collaboratively among the AIUM and other organizations whose members use ultrasound for guidance in vascular T “ ” access procedures (see Acknowledgments ). Recommendations for practitioner requirements, the written request for the examination, procedure documentation, and quality control vary among the organizations and are addressed by each separately. This parameter has been developed by and for clinicians from diverse specialties and practitioner levels who perform vascular access. While vascular access may be performed using external landmarks, point-of-care ultrasound is now increasingly available.1 Appropriately used, ultrasound guidance for vascular access has been shown to improve success rates while reducing iatrogenic injury, the number of needle passes, and infection rates.2 Addition- ally, it may improve patient comfort and satisfaction. This parameter is intended to be evidence based when possi- ble and to include selected references of importance, but it is not meant to be a comprehensive or rigorous literature review, as this has been accomplished elsewhere.3 The intent of this document is to highlight appropriate evidence while also providing a practical, real-world expert consensus from clinicians with diverse back- grounds on the best use and techniques for incorporating ultra- sound into vascular access procedures with the ultimate goal of improving the care of our patients. II. Indications/Contraindications Ultrasound should be used to aid in central venous, peripheral venous, and arterial access procedures.4 When used appropriately by qualified personnel, there are no absolute contraindications to using ultrasound as a procedural adjunct for vascular guidance. -

Catheter Associated Urinary Tract Infection (CAUTI) Prevention
Catheter Associated Urinary Tract Infection (CAUTI) Prevention System CAUTI Prevention Team 1 Objectives At the end of this module, the participant will be able to: Identify risk factors for CAUTI Explain the relationship between catheter duration and CAUTI risk List the appropriate indications for urinary catheter insertion and continued use Implement evidence-based nursing practice to decrease the risk and incidence of CAUTI 2 The Problem All patients with an indwelling urinary catheter are at risk for developing a CAUTI. CAUTI increases pain and suffering, morbidity & mortality, length of stay, and healthcare costs. Appropriate indwelling catheter use can prevent about 400,000 infections and 9,000 deaths every year! (APIC, 2008; Gould et al, 2009) 3 2012 National Patient Safety Goal Implement evidence-based practices to prevent indwelling catheter associated urinary tract infections (CAUTI) Insert indwelling urinary catheters according to evidence-based guidelines Limit catheter use and duration Use aseptic technique for site preparation, equipment, and supplies (The Joint Commission (TJC), 2011) 4 2012 National Patient Safety Goal Manage indwelling urinary catheters according to evidence-based guidelines Secure catheters for unobstructed urine flow and drainage Maintain the sterility of the urine collection system Replace the urine collection system when required Collect urine samples using aseptic technique (TJC, 2011) 5 Sources of CAUTI Microorganisms Endogenous Meatal, rectal, or vaginal colonization Exogenous -

ADOPTED REGULATION of the STATE BOARD of NURSING LCB File No. R122-01 Effective December 14, 2001 AUTHORITY: §§1-7, 13 And
ADOPTED REGULATION OF THE STATE BOARD OF NURSING LCB File No. R122-01 Effective December 14, 2001 EXPLANATION – Matter in italics is new; matter in brackets [omitted material] is material to be omitted. AUTHORITY: §§1-7, 13 and 14, NRS 632.120; §§8-12, NRS 632.120 and 632.237. Section 1. Chapter 632 of NAC is hereby amended by adding thereto a new section to read as follows: “Physician assistant” means a person who is licensed as a physician assistant by the board of medical examiners pursuant to chapter 630 of NRS. Sec. 2. NAC 632.010 is hereby amended to read as follows: 632.010 As used in this chapter, unless the context otherwise requires, the words and terms defined in NAC 632.015 to 632.101, inclusive, and section 1 of this regulation have the meanings ascribed to them in those sections. Sec. 3. NAC 632.071 is hereby amended to read as follows: 632.071 “Prescription” means authorization to administer medications or treatments issued by an advanced practitioner of nursing, a licensed physician, a licensed physician assistant, a licensed dentist or a licensed podiatric physician in the form of a written or oral order, a policy or procedure of a facility or a written protocol developed by the prescribing practitioner. Sec. 4. NAC 632.220 is hereby amended to read as follows: 632.220 1. A registered nurse shall perform or supervise: --1-- Adopted Regulation R122-01 (a) The verification of an order given for the care of a patient to ensure that it is appropriate and properly authorized and that there are no documented contraindications in carrying out the order; (b) Any act necessary to understand the purpose and effect of medications and treatments and to ensure the competence of the person to whom the administration of medications is delegated; and (c) The initiation of intravenous therapy and the administration of intravenous medication. -

Too Many Twos in One Patient: Two Central Venous Catheters, Two
& Experim l e ca n i t in a l l C Journal of Clinical and Experimental C f a o r d l i a o Chalwade, J Clin Exp cardiolog 2018, 9:9 n l o r g u y o Cardiology DOI: 10.4172/2155-9880.1000605 J ISSN: 2155-9880 Case Report Open Access Too Many Twos in One Patient: Two Central Venous Catheters, Two Routes, Two Hospitals, Two Lost Guidewires, Two Vascular Systems, One Patient Rahul Chalwade* Department of Cardiology, Felix Health Care, Noida, Uttar Pradesh, India *Corresponding author: Rahul Chalwade, Department of Cardiology, Felix Health Care, Noida, Uttar Pradesh, India, Phone: +919717053558; E-mail: [email protected] Received date: September 05, 2018; Accepted date: September 10, 2018; Published date: September 17, 2018 Copyright: © 2018 Chalwade R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Central venous catheter insertion by Seldinger's technique is a very common procedure nowadays. The technique though considered safe, is associated with potential dreaded complications. One such complication is intravascular loss of guidewire during insertion. We describe one unusual case of two chronically lost guidewires in venous and arterial system with successful retrieval by innovative interventional techniques. Keywords: Lost guidewire; Interventional cardiology; Interventionl AORTA-ARCH OF AORTA-LOOPING IN DESCENDING AORTA- radiology; Central venous catheter complications; Anaesthesiology; OPENING OF LT SCA (straight tip of guidewire). Snare We did routine blood evaluation, all were normal, venous and arterial Doppler and echo was done to rule out thrombus. -

Caring for Your Urinary (Foley) Catheter
Caring for Your Urinary (Foley) Catheter This information will help you care for your urinary (Foley) catheter while you’re at home. You have had a urinary catheter (a thin, flexible tube) placed in your bladder to drain your urine (pee). It’s held inside your bladder by a balloon filled with water. The parts of the catheter outside your body are shown in Figure 1. Catheter Care ● You need to clean your catheter, change your drainage bags, and wash your drainage bags every day. ● You may see some blood or urine around where the catheter enters your body, especially when walking or having a bowel movement. This is normal, as long as there’s urine draining into the drainage bag. If there’s not, call your healthcare provider. ● While you have your catheter, drink 1 to 2 glasses of liquids every 2 hours while you’re awake. ● Make sure that the catheter is in place in a tension free manner. The catheter should not be tight and should sit loosely. Showering ● You can shower while you have your catheter in place. Don’t take a bath until after your catheter is removed. ● Make sure you always shower with your night bag. Don’t shower with your leg bag. You may find it easier to shower in the morning. Cleaning Your Catheter You can clean your catheter while you’re in the shower. You will need the following supplies: 1. Gather your supplies. You will need: ○ Mild soap ○ Water 2. Wash your hands with soap and water for at least 20 seconds. -

First Simulator for Seldinger Technique and Angiography Training
This is a repository copy of ImaGiNe Seldinger: first simulator for Seldinger Technique and Angiography Training. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/79950/ Version: Accepted Version Article: Luboz, V, Zhang, Y, Johnson, S et al. (20 more authors) (2013) ImaGiNe Seldinger: first simulator for Seldinger Technique and Angiography Training. Computer Methods and Programs in Biomedicine, 111 (2). 419 - 434. ISSN 0169-2607 https://doi.org/10.1016/j.cmpb.2013.05.014 Reuse Unless indicated otherwise, fulltext items are protected by copyright with all rights reserved. The copyright exception in section 29 of the Copyright, Designs and Patents Act 1988 allows the making of a single copy solely for the purpose of non-commercial research or private study within the limits of fair dealing. The publisher or other rights-holder may allow further reproduction and re-use of this version - refer to the White Rose Research Online record for this item. Where records identify the publisher as the copyright holder, users can verify any specific terms of use on the publisher’s website. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ ImaGiNe Seldinger: first simulator for Seldinger technique and angiography training V. Luboz, Y. Zhang, S. Johnson, Y. Song, C. Kilkenny, C. Hunt, H. Woolnough, S. Guediri, J. Zhai, T. Odetoyinbo, P. Littler, A. -
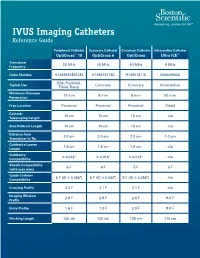
IVUS Imaging Catheters Reference Guide
IVUS Imaging Catheters Reference Guide Peripheral Catheter Coronary Catheter Coronary Catheter Intracardiac Catheter OptiCross™ 18 OptiCross 6 OptiCross Ultra ICE™ Transducer 30 MHz 40 MHz 40 MHz 9 MHz Frequency Order Number H7493932800180 H7495181160 H749518110 M00499000 SFA, Popliteal, Typical Use Coronary Coronary Intracardiac Tibial, Renal Maximum Diameter 12 mm 6 mm 6 mm 50 mm Penetration Prep Location Proximal Proximal Proximal Distal Catheter 15 cm 15 cm 15 cm n/a Telescoping Length Sled Pullback Length 10 cm 10 cm 10 cm n/a Distance from 2.0 cm 2.0 cm 2.0 cm 1.0 cm Transducer to Tip Guidewire Lumen 1.6 cm 1.6 cm 1.6 cm n/a Length Guidewire ≤ 0.018" ≤ 0.014" ≤ 0.014" n/a Compatibility Sheath Compatibility 6 F 6 F 5 F 9 F (with max wire) Guide Catheter 6 F (ID ≥ 0.068") 6 F (ID ≥ 0.064") 5 F (ID ≥ 0.058") n/a Compatibility Crossing Profile 3.5 F 3.1 F 3.1 F n/a Imaging Window 2.9 F 2.9 F 2.6 F 9.0 F Profile Entry Profile 1.6 F 1.3 F 2.0 F 9.0 F Working Length 135 cm 135 cm 135 cm 110 cm OPTICROSS™ 18 CATHETER AND MDU5 PLUS BAG OPTICROSS 6 40 MHZ CORONARY IMAGING CATHETER CAUTION Federal law (USA) restricts this device to sale by or on the order of a physician. Rx only. Prior to use, please see the CAUTION: Federal law (USA) restricts this device to sale by or on the order of a physician. -

Coding Billing
Coding&Billing Quarterly FEBRUARY 2015 EDITOR ALAN L. PLUMMER, MD ATS RUC Advisor Letter from the Editor Welcome to the January 2015 edition of the ATS Coding ADVISORY BOARD MEMBERS: and Billing Quarterly. The New Year will bring a number of KATINA NICOLACAKIS, MD important changes to medicine for practitioners of pulmonary, Chair, ATS Clinical Practice Committee ATS Alternate RUC Advisor critical care and sleep medicine. Below are some issues that ATS STEPHEN P. HOFFMANN, MD members and their staff need to be aware of and prepared for: Member, ATS Clinical Practice Committee ATS CPT Advisor ICD-10 Transition – Barring another last minute intervention MICHAEL NELSON, MD by Congress (which is possible but very unlikely), 2015 will Member, ATS Clinical Practice Committee be the year of the ICD-10 transition. I hope providers and ATS Alternate CPT Advisor practices are well underway preparing for the transition. Over the past year, the STEVE G. PETERS, MD Member, ATS Clinical Practice Committee ATS Coding and Billing Quarterly has featured articles on the transition. The April 2015 edition will cover ICD-10 for pediatric pulmonary services. Lung Cancer Screening Coverage – Earlier this month, the Centers for Medicare In This Issue and Medicaid Services (CMS) released its final coverage policy for lung cancer Low Dose CT Lung Cancer screening. In this issue, Dr. Kovitz describes the final coverage policy, its impact Screening Coverage - Implications on Medicare and private coverage, as well as tips for coding services related to for the Practitioner, page 2 screening. 2015 Brings New Extracorporeal Membrane Oxygenation New ECMO codes – Also covered in this issue is the new and expanded family of (ECMO)/Extracorporeal Life codes for EMCO services.