Back in Hawaiʻi! Professionals at Risk
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Volume XII, No
March 31—April 6, 2011 Volume XII, No. 13 Willie Nelson added to line-up for “Kokua For Japan” on April 10 World-renowned entertainer Willie Nelson will perform at “Kokua For Japan,” a Hawai‘i-based radio, television and Internet fund raising event for the victims of the earthquake and tsunami in Japan. The event, staged by Clear Channel Radio Hawaii and Oceanic Time Warner Cable, will take place at the Great Lawn at the Hilton Hawaiian Village Beach Resort & Spa on April 10, 2011 from noon to 5 p.m. All proceeds to benefit the American Red Cross for the Japan earthquake and Pacific tsunami relief efforts. Nelson will join previously announced entertainers including: Henry Kapono with special guests Michael McDonald and Mick Fleetwood; Loretta Ables Sayre; The Brothers Cazimero; Cecilio & Kapono; Kalapana; Cecilio & Kompany; Amy Hanaialii; Na Leo; John Cruz; Natural Vibrations; ManoaDNA; Robi Kahakalau; Mailani; Taimane; Go Jimmy Go; Jerry Santos; Gregg Hammer Band; and Kenny Endo Taiko. On-air personalities from Clear Channel Radio and local broadcast and cable TV stations will host the program. “Kokua For Japan,” a Hawai‘i-based radio, television and Internet fund raising event for the victims of the earthquake and tsunami in Japan, will be held on Sunday, April 10, 2011 from noon to 5 p.m. The event, staged by Clear Channel Radio Hawaii and Oceanic Time Warner Cable, will take place at the Great Lawn at the Hilton Hawaiian Village Beach Resort & Spa. Tickets are available for $15 via Honolulu Box Office. Visit HonoluluBoxOffice.com for on-line purchasing or call 808-550-8457 for charge-by-phone. -

State of Hawaii Office of Elections I I Election Information Services I Operators Manual I I I 1996 Elections I I I I I I I I
Date Printed: 06/16/2009 JTS Box Number: IFES 80 Tab Number: 74 Document Title: Election Information Services Operator's Manual Document Date: 1996 Document Country: United States -- Hawaii Document Language: English IFES ID: CE02160 I I I I I I State of Hawaii Office of Elections I I Election Information Services I Operators Manual I I I 1996 Elections I I I I I I I I I TABLE OF CONTENTS I General Information Objectives. ... .. 1 Reminders ...................................................................... 2 I Commonly Used Terms ........................................................... 3 Who's Who at Control Center . .. 3 I Standard Operating Procedures Buck Slip Calls . .. 4 Informational Calls. .. 6 I Commonly Asked Questions Am I registered to vote? : . .. 7 Who may register to vote? . .. 7 I Should I re-register to vote? ........................................................ 7 Willi be notified of my polling place? ............. .. 8 Where is my polling place? . .. 8 I What are the polling place hours? ................................................... 8 Do I need an 1.0. to vote on Election Day? ............................................. 8 Am I allowed to take time off from work for voting? . .. 8 Who will be running this year for the various political offices? .............................. 9 I What types of elections does Hawaii hold? ...................... :..................... 9 Registration Information I QAlAB ......................................................................... 10 Same Day Transfer of Registration -
HGEA Staff & Members Working for Our Legislative Priorities
JANUARY 2015 | VOLUME 50 | ISSUE 1 www.hgea.org Hawaii Government Employees Association AFSCME LOCAL 152, AFL-CIO HGEA Staff & Members Working For Our Legislative Priorities The bad old days of the Republican Lingle administration, economic distress, and legislative take-away bills are still fairly fresh memories even though we have now been experiencing a slow economic recovery. You may remember it was February 2009 when House Speaker Calvin Say introduced bills that would have stripped away public employee benefits. Those bills, introduced under the guise of cost saving measures, proposed to cut health insurance benefits, eliminate prescription drug coverage for all employees and cut dental, vision and life insurance benefit coverages. HGEA Legislative Officer Michele Kurihara-Klein said, State Rep. Mark Nakashima, chair of the House Committee on Labor & Public “HGEA members and staff unified and fought hard against Employment, and HGEA Legislative Officer Michele Kurihara-Klein the take-away bills through political action, which included submitting testimony, attending hearings, and lobbying Did you know Hawaii Government Employees Association legislators. All that hard work paid off in the end, however we staff will review every bill that is submitted during the 2015 must remain vigilant.” legislative session? That’s about 3,000 bills and several hundred resolutions. As we’ve seen in the past, when we are united, we This recent example highlights how all of our members’ can and do make a difference. Every HGEA member can be hard-earned benefits can be taken away by legislation. That’s part of the political process. Staff may need your help during why political action, supporting legislators who support the legislative session to attend hearings and submit testimony. -
114TH CONGRESS / First Session Available at Frcaction.Org/Scorecard
FRC ACTION VOTE SCORECARD 114TH CONGRESS / First Session Available at FRCAction.org/scorecard U.S. House of Representatives and U.S. Senate Dear Voter and Friend of the Family, FRC Action presents our Vote Scorecard for the First Session of the 114th Congress. This online Scorecard contains a compilation of significant votes on federal legislation affecting faith, family, and freedom that FRC Action either supported or opposed. These recorded votes span the 2015 calendar year and include the greatest number of pro-life votes in history, after the U.S. House increased its Republican membership and the U.S. Senate was returned to Republican control. The year began with a bipartisan effort in the House to prohibit federal funds from being used to pay for abortion coverage under Obamacare. Congress successfully fought to restrict FDA approval of some forms of embryo-destructive research. The House, once again, passed legislation that would prevent late abortions on 5 month old pain-capable unborn children, and although the Senate was unable to pass the bill due to the 60 vote threshold, for the first time, a majority of Senators voted in favor of the bill. The public release of videos revealing Planned Parenthood’s organ harvesting practices renewed efforts to defund this scandal-ridden organization and redirect funding towards community health centers. In an unprecedented victory, the House and Senate passed a budget reconciliation bill, the Restoring Ameri- cans’ Healthcare Freedom Reconciliation Act, which would have eliminated a significant portion of Planned Parenthood’s funding—roughly 80%— and repealed key provisions of Obamacare. -

Newly Elected Representatives in the 114Th Congress
Newly Elected Representatives in the 114th Congress Contents Representative Gary Palmer (Alabama-6) ....................................................................................................... 3 Representative Ruben Gallego (Arizona-7) ...................................................................................................... 4 Representative J. French Hill (Arkansas-2) ...................................................................................................... 5 Representative Bruce Westerman (Arkansas-4) .............................................................................................. 6 Representative Mark DeSaulnier (California-11) ............................................................................................. 7 Representative Steve Knight (California-25) .................................................................................................... 8 Representative Peter Aguilar (California-31) ................................................................................................... 9 Representative Ted Lieu (California-33) ........................................................................................................ 10 Representative Norma Torres (California-35) ................................................................................................ 11 Representative Mimi Walters (California-45) ................................................................................................ 12 Representative Ken Buck (Colorado-4) ......................................................................................................... -

September/October 2016 VOICE the ILWU Page 1
OF September/October 2016 VOICE THE ILWU page 1 HAWAII Volume 56 • No. 5 The VOICE of the ILWU—Published by Local 142, International Longshore & Warehouse Union September/October 2016 Please support candidates ADDRESS L A BE who support working people L The General Election is coming up on Tuesday, November 8. Don’t forget to vote! On the Inside A new ILWU Local in Hawaii ..... 2 Kauai pensioners enjoy their annual picnic ................. 3 Honolulu Mayor Kirk Caldwell (second from left), U.S. Senator Mazie Hirono (fourth from right), and Oahu Business ILWU members on Oahu Agent Wilfred Chang (second from right) with ILWU members from Unit 4526 - Pacific Beach Hotel at the Labor Unity celebrate Labor Day Picnic held on Saturday, September 17, 2016 at the Waikiki Shell. Caldwell is an ILWU-endorsed candidate, and all and Labor Unity ..................4-5 Oahu members are urged to support him for Mayor in the upcoming General Election on November 8. Caldwell is endorsed by the ILWU because he has made working families on Oahu his priority. Improving public safety, repaving Kauai teams take state roads, fixing sewers, and housing homeless veterans are some of Caldwell’s accomplishments during his first term as golf tournament by storm ...... 6 Honolulu mayor. He has always listened to and tried to address the needs of ILWU members and their communities. Charter Amendments: What are these questions Trade Adjustment Assistance on the ballot? .......................... 7 approved for more HC&S workers Who are the candidates who work for working families? Special benefits and By Joanne Kealoha petitions for other sugar companies that Constitutional Amendment Social Sevices Coordinator closed, but each of those petitions were services under TAA recommendations ................ -

The Evolution of the Digital Political Advertising Network
PLATFORMS AND OUTSIDERS IN PARTY NETWORKS: THE EVOLUTION OF THE DIGITAL POLITICAL ADVERTISING NETWORK Bridget Barrett A thesis submitted to the faculty at the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Master of Arts at the Hussman School of Journalism and Media. Chapel Hill 2020 Approved by: Daniel Kreiss Adam Saffer Adam Sheingate © 2020 Bridget Barrett ALL RIGHTS RESERVED ii ABSTRACT Bridget Barrett: Platforms and Outsiders in Party Networks: The Evolution of the Digital Political Advertising Network (Under the direction of Daniel Kreiss) Scholars seldom examine the companies that campaigns hire to run digital advertising. This thesis presents the first network analysis of relationships between federal political committees (n = 2,077) and the companies they hired for electoral digital political advertising services (n = 1,034) across 13 years (2003–2016) and three election cycles (2008, 2012, and 2016). The network expanded from 333 nodes in 2008 to 2,202 nodes in 2016. In 2012 and 2016, Facebook and Google had the highest normalized betweenness centrality (.34 and .27 in 2012 and .55 and .24 in 2016 respectively). Given their positions in the network, Facebook and Google should be considered consequential members of party networks. Of advertising agencies hired in the 2016 electoral cycle, 23% had no declared political specialization and were hired disproportionately by non-incumbents. The thesis argues their motivations may not be as well-aligned with party goals as those of established political professionals. iii TABLE OF CONTENTS LIST OF TABLES AND FIGURES .................................................................................................................... V POLITICAL CONSULTING AND PARTY NETWORKS ............................................................................... -

Making Honolulu an Age-Friendly City: an Action Plan
Making Honolulu an Age-Friendly City: An Action Plan Final June 2015 Making Honolulu an Age-Friendly City: An Action Plan Prepared by: Final The University of Hawai‘i Center on Aging June 2015 Mayor's Letter i This page is intentionally left blank. ii Mayor's Letter Congressman Takai Letter iii This page is intentionally left blank. iv Congressman Takai Letter Mahalo to our Sponsors! Visionary Sponsor Fiscal Sponsor Leader Sponsors Friend Sponsor Sponsor Brought to Hawaii by Mahalo to our Sponsors! v Acknowledgements Th e Steering Committee acknowledges the following with our thanks: Honolulu City Council Citizen's Advisory Committee Members Technical Committee Members Kaiser Permanente Hawaii Key Informant Interviewees Focus Group Participants AARP City and County of Honolulu Departments and Staff Department of Business, Economic Development, and Tourism, State of Hawai`i Department of Health, State of Hawai`i `Iolani School O`ahu Metropolitan Planning Organization (OMPO) Momi Cazimero Printing of this report was made possible through in-kind support from Kaiser Permanente Hawaii vi Acknowledgements Table of Contents Letter from the Mayor ................................................................................................i Letter from U.S. Congressman Mark Takai ............................................................ iii Mahalo to our Sponsors ............................................................................................v Acknowledgements ...................................................................................................vi -

Hawaii Clean Energy Final PEIS
1 APPENDIX A 2 3 Public Notices Notices about the Draft Programmatic EIS Appendix A The following Notice of Availability appeared in the Federal Register on April 18, 2014. Hawai‘i Clean Energy Final PEIS A-1 September 2015 DOE/EIS-0459 Appendix A Hawai‘i Clean Energy Final PEIS A-2 September 2015 DOE/EIS-0459 Appendix A DOE-Hawaii placed the following advertisement in The Garden Island on May 5 and 9, 2014. Hawai‘i Clean Energy Final PEIS A-3 September 2015 DOE/EIS-0459 Appendix A DOE-Hawaii placed the following advertisement in the West Hawaii Today on May 6 and 12, 2014. Hawai‘i Clean Energy Final PEIS A-4 September 2015 DOE/EIS-0459 Appendix A DOE-Hawaii placed the following advertisement in the Hawaii Tribune Herald on May 7 and 12, 2014. Hawai‘i Clean Energy Final PEIS A-5 September 2015 DOE/EIS-0459 Appendix A DOE-Hawaii placed the following advertisement in the Maui News on May 8, 2014. Hawai‘i Clean Energy Final PEIS A-6 September 2015 DOE/EIS-0459 Appendix A DOE-Hawaii placed the following advertisement in the Maui News on May 13, 2014. Hawai‘i Clean Energy Final PEIS A-7 September 2015 DOE/EIS-0459 Appendix A DOE-Hawaii placed the following advertisement in the Maui News on May 18, 2014. Hawai‘i Clean Energy Final PEIS A-8 September 2015 DOE/EIS-0459 Appendix A DOE-Hawaii placed the following advertisement in the Molokai Dispatch on May 7 and 14, 2014. Hawai‘i Clean Energy Final PEIS A-9 September 2015 DOE/EIS-0459 Appendix A DOE-Hawai‘i placed the following advertisement in the Star-Advertiser on May 14 and 19, 2014. -
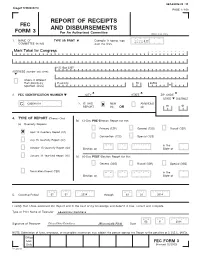
Report of Receipts and Disbursements
04/14/2014 23 : 33 Image# 14960684214 PAGE 1 / 159 REPORT OF RECEIPTS FEC AND DISBURSEMENTS FORM 3 For An Authorized Committee Office Use Only 1. NAME OF TYPE OR PRINT Example: If typing, type 12FE4M5 COMMITTEE (in full) over the lines. Mark Takai for Congress P.O. Box 2267 ADDRESS (number and street) Check if different than previously Pearl City HI 96782 reported. (ACC) 2. FEC IDENTIFICATION NUMBER CITY STATE ZIP CODE STATE DISTRICT C C00548131 3. IS THIS NEW AMENDED REPORT (N) OR (A) HI 01 4. TYPE OF REPORT (Choose One) (b) 12-Day PRE -Election Report for the: (a) Quarterly Reports: Primary (12P) General (12G) Runoff (12R) April 15 Quarterly Report (Q1) Convention (12C) Special (12S) July 15 Quarterly Report (Q2) M M / D D / Y Y Y Y in the October 15 Quarterly Report (Q3) Election on State of January 31 Year-End Report (YE) (c) 30-Day POST -Election Report for the: General (30G) Runoff (30R) Special (30S) Termination Report (TER) M M / D D / Y Y Y Y in the Election on State of M M / D D / Y Y Y Y M M / D D / Y Y Y Y 5. Covering Period 01 2014 through 03 31 2014 I certify that I have examined this Report and to the best of my knowledge and belief it is true, correct and complete. Type or Print Name of Treasurer Edward Dion Kaimihana M M / D D / Y Y Y Y 03 31 2014 Signature of Treasurer Edward Dion Kaimihana [Electronically Filed] Date NOTE: Submission of false, erroneous, or incomplete information may subject the person signing this Report to the penalties of 2 U.S.C. -
2006 October Engineers News
newsnews VOL. 64, #10 • OPERATING ENGINEERS LOCAL UNION NO 3 • ALAMEDA, CA • OCTOBER 2006 Generations of Strength • A new beginning for Local 3 • A new governor for California Get out the vote – Nov. 7 OE3 endorsements inside! 2 E NGINEERS N EWS E O CTOBER 2006 For The Good & Welfare By Russ Burns, business manager From left: Forty-year-member Hank Gutierrez tries a special tension-relieving oil from BeautiControl specialists Kristina In high gear Turner and Kendra Ollar. .11 It was good to see all of you last month at • Mel Brown for House District 53 the September Semi-Annual. We had a great • Jay Seegmiller for House District 49 turnout and lots of Local 3 families joining us, • Trisha Beck for Senate District 9 Contents which was nice to see. I know many of you As I’ve mentioned, a complete list of elec- (myself included) enjoyed hearing from Phil Angelides. His attendance says quite a lot about tion recommendations is listed on pages 4-7. Under the Dome . .4 the political power and significance of Local 3, Rancho Murieta . .8 especially at this point in the campaign, so Attend your district meeting Fringe Benefits . .9 close to Election Day. In addition to this month’s political spread, If you weren’t able make it to the Semi- Credit Union . .10 we’re talking politics (and much more) during Annual, we have full coverage for you in this our fall round of district meetings across the ju- Safety . .10 issue of Engineers News, beginning on page 11. Semi-Annual . -

Ho'omalimali and the Succession Model of Political Inheritance In
Ho'omalimali and the Succession Model of Political Inheritance in Hawai'i: A Study of the Electoral Dominance of Americans of Japanese Ancestry in State and Congressional Politics Skyler Allyn Korgel ANS 678H Departmental Honors in Asian Studies The University of Texas at Austin May 2018 Dr. Chiu-Mi Lai Department of Asian Studies Thesis Supervisor Dr. Patricia Maclachlan Department of Government Second Reader Abstract “Ho’omalimali” and the Succession Model of Political Inheritance in Hawai'i: A Study of the Electoral Dominance of Americans of Japanese Ancestry in State and Congressional Politics Author: Skyler Korgel Thesis Supervisor: Dr. Chiu-Mi Lai Second Reader: Dr. Patricia Maclachlan This thesis seeks to discover the underlying causes and factors for the unique political situation in Hawai'i where a minority demographic has been historically dominant. In researching historical and political contexts, as well as institutional and electoral factors, analysis of all these findings has shown a constructed “succession model” behind the dominance of Americans of Japanese Ancestry (AJA) through the Democratic Party. The thesis also examines the implications of the disrupted and further divisive political climate of the Hawai'i Democratic Party since the death of universally respected and revered Senator Daniel Inouye (1924-2012). Senator Inouye’s death brought to an end a political career that spanned nearly six decades, and commenced a new era for Hawai'i political leadership. Quite possibly, this new era has also fractured the succession model. In a 75% minority state, throughout the past 65 years, Americans of Japanese ancestry have managed to gain a stranglehold over the Hawai'i Democratic Party, and therefore the Hawai’i state government itself.