Restructuring the Medical Council of India
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gapsc Certificate Level Upgrade Rule Guidance
GaPSC Certificate Level Upgrade Rule 505-2-.41 GUIDANCE FOR EDUCATORS Introduction and Use of This Document In Georgia the Professional Standards Commission (GaPSC) is the state agency authorized to assume full responsibility for the certification, preparation and conduct of certified, licensed or permitted education personnel employed in Georgia, and the development and administration of educator certification testing. The GaPSC's authority applies to certified, licensed and permitted personnel employed in Georgia public schools and institutions of higher learning that prepare educators. This document is intended to provide guidance to educators regarding the implementation of GaPSC Rule 505-2-.41, Educator Certificate Upgrades. Foci of this guidance document include: Ensuring educators understand Rule 505-2-.41 Explaining how Rule 505-2-.41 affects Georgia educators; and Providing links to other relevant and important documents or resources. Organized by the foci listed above, topics and relevant links are provided in the order and locations referenced below. E-mail suggested additions or improvements to this document to Dr. Bobbi Ford at [email protected]. Topics Pages Section I: Key Components of Rule 505-2-.41 2 - 3 Section II: Advanced Degree Program Options and Requirements 3 - 9 A. Program Options B. In-Field Upgrade Requirements C. New Field Upgrade Requirements D. Three New Fields of Certification E. Grandfathering Timelines F. Voluntary Deletion of Certificate Section III: Seeking Advisement 9 - 10 Section IV: Appendices -
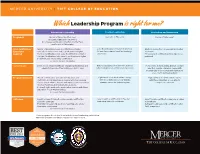
Whichleadership Program Is Right For
MERCER UNIVERSITY | TIFT COLLEGE OF EDUCATION Which Leadership Program is right for me? Educational Leadership Teacher Leadership Curriculum and Instruction Program(s) Master of Education (Tier One), Specialist in Education Doctor of Philosophy* Specialist in Education (Tier Two), Non-Degree Certification Only (Tier One, Tier Two), and Doctor of Philosophy* Prior Certification/ • Master of Education: Level 4 certification or higher • Level 5 certification or higher in any field • Master’s degree from a regionally accredited Experience • Specialist in Education: Level 5 certification or higher • At least three years of certified teaching institution Required • Tier One Certification Only: Level 5 certification or higher experience • Three years of certified teaching experience • Tier Two Certification Only: Level 6 certification or higher preferred • Doctoral: Level 6 leadership certification See reverse for more information. Career Goals Enter into or advance within an educational leadership and Enter a leadership or mentor role without Pursue roles at the building, district, or state administration role at the building or district level fully moving into an administration position level that require a terminal degree with an emphasis on curriculum and instruction assessment and development Program Structure • Master of Education, Specialist in Education, and Eight-week or 16-week online courses Eight-week or 16-week online courses Certification Only: Eight-week courses with four evening with three Saturdays on our Atlanta with three Saturdays on our Atlanta classes at our Atlanta, Macon, and Henry County locations† campus across the entire program campus per semester and four field-based clinical practice sessions • Doctoral: Eight-week or 16-week online courses with three Saturdays on our Atlanta campus See reverse for more information. -

The Graduate Faculty Handbook, 1992)
1 THE GRADUATE FACULTY HANDBOOK SCHOOL OF GRADUATE & PROFESSIONAL STUDIES TENNESSEE STATE UNIVERSITY NASHVILLE, TENNESSEE Revised 9/28/2018 2 TABLE OF CONTENTS SCHOOL OF GRADUATE & PROFESSION STUDIES ......................................................................... 3 Goals of the School of Graduate & Professional Studies................................................... 5 ADMINISTRATION OF THE GRADUATE PROGRAMS ..................................................................... 6 GRADUATE FACULTY ................................................................................................................... 7 Policy on Certification of Full Graduate Faculty Membership ........................................... 7 Application for Full Graduate Faculty Membership ........................................................ 10 Policy on Re-certification of Full Graduate Faculty membership .................................... 13 Application for Re-certification to Full Graduate Faculty Membership ........................... 15 Policy on Certification of Associate Graduate Faculty .................................................... 18 Application for Associate Level 1 Graduate Faculty Membership ................................... 19 Application For Associate Level 2 Graduate Faculty Membership .................................. 20 Policy on Adjunct Graduate Faculty Membership .......................................................... 22 Application For Adjunct Graduate Faculty Membership ................................................ -

Minimum Requirements for a Homeopathic Medical College in India & Qualification of Teaching Staff No
Minimum requirements for a Homeopathic Medical college in India & Qualification of Teaching Staff No. 7-1/83-CCH Central Council Of Homoeopathy. India New Delhi-110057 Dated The 11 May, 1983 Notification In exercise of the powers conferred by clauses (I), (j) and (k) of section 33 and sub-section (1) of section 20 of the Homoeopathy Central Council Act, 1973 (59 of 1973), the Central Council of Homoeopathy, the previous sanction of the Central Government hereby makes the following regulations, namely :- Part I - Short Title, Commencement and Definition Part II - Staff Equipments, Training and other facilities Part III - Accomodation Part IV - Residential Accomodation PART I .Preliminary 1. Short title and commencement: (i) These regulations may be called the Homoeopathy (Minimum Standards of Education) Regulations, 1983. (ii) They shall come into force on the date of their publication in the Gazette of India. 2. Definitions: In these regulations, unless the context otherwise requires - (i) "Act" means the Homoeopathy Central Council Act; 1973 (59 of 1973); (ii) "Courses" means the courses of study in Homoeopathy, namely :- (a) D.H.M.S. (Diploma in Homoeopathic Medicine and Surgery) and (b) B.H.M.S. (Bachelor of Homoeopathic Medicine and Surgery) (c) M.D.(Hom.) [Doctor of Medicine (Homoeopathic)] in various specialities (iii) "Diploma" means a Diploma in Homoeopathy as defined in clause (iii) of regulation 3 of the homoeopathy (Diploma Course) Regulation, 1983; (iv) "Degree" means a Degree in Homoeopathy as defined in clause (iv) of regulation 2 of the Homoeopathy (Graded Degree Course0 Regulations, 1983 or in clause (iv) of regulation 2 of the Homoeopathy (Degree Course) Regulations, 1983; (iv)(a) "Post Graduation in Homoeopathy" means a Post Graduate qualification in Homoeopathy recognized as per the provisions of the Act. -

Russia Country Statistics Population: 142,257,519 (July 2017 Est.) Ethnic Groups: Russian 78%, Tatar 4%, Other 18%
Russia Country Statistics Population: 142,257,519 (July 2017 est.) Ethnic Groups: Russian 78%, Tatar 4%, Other 18% Religions: Russian Orthodox 15-20%, Muslim 10-15%, Other 70-60% Languages: Russian (official) 86%, Tatar 4%, Other 10% Area: 17,098,242 sq km (approximately 1.8 times the size of the US) Government Type: Semi-Presidential Federation National Capital: Moscow Currency: Russian Rubles (RUB) Educational System Grading Scale – All Levels Secondary Reported Grade Translation US Certificate of Basic General Education Grades 1-9 Equiv Аттестат об основном общем образовании 5 Отлично Excellent A Attestat ob osnovnom obschem obrazovanii Otlichno Certificate of (Complete) General Secondary Education Grades 10-11 4 Хорошо Good B Аттестат о среднем (полном) общем образовании Khorosho Attestat o srednem (polnom) obschem obrazovanii 3 Удовлетворительно Satisfactory C Udovletvoritel’no Postsecondary 2 Неудовлетвори- Unsatisfactory F Russia is a member of the European Higher Education Area and is part of the Bologna Process as of 2003. тельно Bachelor’s Diploma 4 years Neudovletvoritel’no Диплом бакалавра 1 Неудовлетвори- Unsatisfactory F Diplom Bakalavra тельно Specialist’s Diploma 5-6 years Neudovletvoritel’no Диплом специалиста] – Зачет Pass P Diplom Spetsialista Zachet Master’s Diploma 2 years Диплом магистра Diplom Magistra Diploma of Candidate of Sciences 3 or more years Диплом кандидата наук Diplom Kandidata Nauk IU Placement Recommendations Freshman • Certificate of (Complete) General Secondary Education Transfer • 1-3 years undergraduate study • Specialist’s Degree program when a graduation certificate was not obtained Graduate • Bachelor’s Diploma • Specialist’s Diploma when a graduation certificate was obtained Required Academic Records Undergraduate Applications • Lower Secondary School Transcript o For Grade 9 • Upper Secondary Transcript • Certificate of (Complete) General Secondary Education Graduate Applications For transcripts, alternatively we can accept the Diploma Supplement if accompanied by the degree certificate. -

Graduate Curriculum Development & Change
GRADUATE CURRICULUM DEVELOPMENT AND CHANGE POLICIES AND PROCEDURES MANUAL OFFICE OF ACADEMIC AFFAIRS AND THE GRADUATE SCHOOL 2017 TABLE OF CONTENTS Introduction ....................................................................................................................................1 Standards of Excellence in Graduate Programs .........................................................................2 Program-Related Actions New and Spin-off Degree Program Proposals .................................................................5 Proposed Timetable ..............................................................................................10 Degree Program Modification ........................................................................................11 Program Merger ..............................................................................................................13 Program Discontinuation or Curtailment .....................................................................17 Course-Related Actions Proposing New Courses and Modifying or Deactivating Current Courses................21 Concentrations .............................................................................................................................23 Certificates: Credit and Non-Credit ..........................................................................................25 Appendices ....................................................................................................................................26 APPENDICES -

(Ed.S.) in Curriculum & Instruction Major in Mathematics
Florida State University School of Teacher Education Specialist (Ed.S.) in Curriculum & Instruction Major in Mathematics Education The Ed.S. is intended to provide advance studies with more in-depth opportunities to further knowledge and practice in the areas of mathematics teaching and learning. Applicants for this program should have substantial teaching experience. There are two specific profiles of applicants that the program is designed to serve: Secondary Mathematics Education The applicant is certified to teach high school mathematics and may have experience teaching middle or high school mathematics as a full-time classroom teacher. The applicant also has substantial coursework in undergraduate mathematics, having successfully completed at least 12 units of mathematics beyond Calculus III with grades of “B” or better. Coursework will include graduate courses in mathematics, as well as advanced courses in Mathematics Education. Middle Grades Mathematics Education The applicant is certified to teach middle grades mathematics and may have experience teaching K-12 mathematics. The applicant must have completed substantial coursework in undergraduate mathematics and has completed at least Calculus II with a grade of “B” or better. Coursework may include graduate mathematics content courses designed especially for teachers, as well as courses in advance studies of Mathematics Education. Florida State University School of Teacher Education Specialist (Ed.S.) in Curriculum & Instruction Major in Mathematics Education Program Element Credits Element Description Interdepartmental Core (see advisor for list 9 This element represents an opportunity to gain of specific courses) insights from faculty external to the School of Curriculum Theory (3) Teacher Education, as well as departmental faculty Learning Theory (3) outside of the Mathematics Education major. -

Directorate of Medical Education
1 Directorate of Medical Education Hand Book on Right to Information Act - 2005 2 CHAPT ER DETAILS PAGE NO NO. 1. INTRODUCTION 3 2 PARTICULARS OF ORGANISATION, FUNCTIONS AND DUTIES 5 3 POWERS AND DUTIES OF OFFICERS AND EMPLOYEES 80 4 RULES, REGULATIONS,INSTRUCTIONS, MANUAL AND RECORDS 91 FOR DISCHARGING FUNCTIONS 5 PARTICULARS OF ANY ARRANGEMENT THAT EXISTS FOR 93 CONSULTATION WITH OR REPRESENTATION BY THE MEMBERS OF THE PUBLIC IN RELATION TO THE FORMULATION OF ITS POLICY OR IMPLEMENTATION THEREOF 6 A STATEMENT OF THE CATEGORIES OF DOCUMENTS THAT ARE 94 HELD BY IT OR UNDER ITS CONTROL 7 A STATEMENT OF BOARDS, COUNCIL, COMMITTEES AND OTHER 95 BODIES CONSTITUTED AS ITS PART 8 THE NAMES, DESIGNATION AND OTHER PARTICULARS OF THE 96 PUBLIC INFORMATION OFFICER 9 PROCEDURE FOLLOWED IN DECISION MAKING PROCESS 107 10 DIRECTORY OF OFFICERS AND EMPLOYEES 108 11 THE MONTHLY REMUNERATION RECEIVED BY EACH OF ITS 110 OFFICERS AND EMPLOYEES INCLUDING THE SYSTEM OF COMPENSATION AS PROVIDED IN REGULATIONS. 12 THE BUDGET ALLOCATED TO EACH AGENCY/OFFICERS 111 (PARTICULARS OF ALL PLANS, PROPOSED EXPENDITURES AND REPORTS ON DISBURSEMENT MADE 116 13 THE MANNER OF EXECUTION OR SUBSIDY PROGRAMME 14 PARTICULARS OF RECEIPIENTS OF CONCESSIONS, PERMITS OR 117 AUTHORISATION GRANTED BY IT 15 NORMS SET BY IT FOR THE DISCHARGE OF ITS FUNCTIONS 118 16 INFORMATION AVAILABLE IN AN ELECTRONIC FORM 119 17 PARTICULARS OF THE FACILITIES AVAILABLE TO CITIZENS FOR 120 OBTAINING THE INFORMATION 18 OTHER USEFUL INFORMATION 121 3 CHAPTER-1 - INTRODUCTION 1.1This handbook is brought out by the Directorate of Medical Education (Government of Tamil Nadu) , Chennai as required by the Right to Information Act, 2005. -

Instructions for Applying for the Title of Docent
INSTRUCTIONS 1 (4) Faculty of Medicine and Health Technology INSTRUCTIONS FOR APPLYING FOR THE TITLE OF DOCENT 1. Title of docent According to Section 89 of the Universities Act (558/2009), a university may award the title of docent to a person who has comprehensive knowledge of their field, a capacity for independent research or artistic work as demonstrated through publications or in some other manner, and good teaching skills. On 12 February 2019, the president issued instructions on the granting of the title of docent at Tampere University. 2. Requirements for the granting of the title of docent Tampere University has set out the following university-level requirements for the granting of the title of docent: - doctoral degree - comprehensive knowledge of their own field - a capacity for independent research as demonstrated through publications or in some other manner - significant scientific publications produced primarily after a dissertation. It is recommended that the title of docent not be applied for at too early a stage. - good teaching skills - other field-specific criteria: Besides the university-level requirements mentioned above, the Faculty of Medicine and Health Technology has the following requirements for the granting of the title of docent: Scientific publications The applicant’s scientific publications must show that the applicant has comprehensive knowledge of the field in which the title is being sought and the capacity for independent scientific research. The applicant’s scientific publications must show that the applicant has created their own line of research and that the applicant's research is actively ongoing. The evaluation primarily considers original articles that have been published or approved for publication in international, peer-reviewed publication series. -

EDUCATIONAL SPECIALIST (Ed.S.) Superintendent Curriculum Leadership Online
EDUCATIONAL SPECIALIST (Ed.S.) Superintendent Curriculum Leadership Online www.hsu.edu To ensure that graduate candidates preparing for senior level educational administration positions or superintendency have the opportunity to gain knowledge and skills and dispositions necessary to be productive and successful school leaders, Henderson is committed to the development and delivery of an exemplary post master’s degree program in educational leadership. In order to meet the needs of a diverse and wide-spread cohort of candidates, the Henderson Ed. Specialist program is offered fully online via Blackboard Collaborate, using an internet/webcam delivery system. The Educational Leadership Department supports the Teachers College mission by focusing on communication, professionalism, knowledge and best practices. The department also focuses on the following dispositions: 1. Valuing diversity 2. Fairness to all 3. Having a sense of efficacy 4. Being reflective learners 5. Emphasizing professionalism The Henderson State University Educational Leadership program offers an Educational Specialist in District Leadership (Ed.S.) that prepares graduate students for superintendent licensure. The degree and the program of study driven by standards are delivered through online courses aligned to the Interstate School Leaders Licensure Consortium (ISLLC), the Educational Leadership Constituent Council (ELCC) and the International Society for Technology in Education (ISTE). Mission Statement: The HSU Educational Leadership Educational Specialist program prepares candidates for P-12 district level leadership roles and empowers them to work collaboratively with diverse populations. Our stakeholders include parents, community, civic organizations, business, media, teachers, and students. The program is designed to improve the leader’s skills in impacting student achievement and the quality of life for students through excellence in teaching, learning, service, technology, and leadership. -

Restructuring the Medical Council of India
IMPACT SERIES NO. 082017 | AUGUST 2017 Restructuring the Medical Council of India Shamika Ravi, Dhruv Gupta, Jaclyn Williams Brookings India IMPACT Series © 2017 Brookings Institution India Center No. 6, Second Floor, Dr. Jose P Rizal Marg Chanakyapuri, New Delhi - 110021 www.brookings.in Recommended citation: Ravi, Shamika; Gupta, Dhruv; Williams, Jaclyn (2017). “Restructuring the Medical Council of India ,” Brookings India IMPACT Series No. 082017. August 2017. The Brookings Institution India Center serves as a platform for cutting-edge, independent, policy- relevant research and analysis on the opportunities and challenges facing India and the world. The Center is based in New Delhi, and registered as a company limited by shares and not for profit, under Section 8 of the Companies Act, 1956. Our work is centered on the motto of “Quality, Independence, Impact.” All content reflects the individual views of the author(s). Brookings India does not hold an institutional view on any subject. Restructuring the Medical Council of India Shamika Ravi1 Dhruv Gupta Jaclyn Williams We are grateful to Srinath Reddy, Sujatha Rao, Preyanuj Yamwong and Bhargava Anantha Swamy for detailed discussions and comments that have enriched this paper. We also thankfully acknowledge all the doctors who participated in our survey across the country. 1 Corresponding author: [email protected] Key Recommendations Excluding/Limiting the number of National Medical Commission representatives in the Medical Advisory Council in order to divide power, promote autonomy, and prevent corruption. Creation of Regional Medical Councils across regions of India, instead of having the Medical Assessment and Rating Board hire third party assessment agencies. This will promote competition amongst the regions to improve quality and process of assessment. -

Auto Certificazione Titolo Accademico
ALLEGATO AL BANDO INTERNAZIONALE PROMETEO WORLD ONU 2019 ATTACHMENT TO THE INTERNATIONAL CALL PROMETEO WORLD ONU 2019 AUTOCERTIFICAZIONE TITOLO ACCADEMICO/ESAMI SOSTENUTI SELF-CERTIFICATION OF ACCADEMIC TITLES/EXAMS TAKEN New Humanity via Piave, 15 Grottaferrata (Roma), Italia e-mail [email protected] Io sottoscritto/a / I, the undersigned ……….…………………………………………………………………. DICHIARO SOTTO LA MIA RESPONSABILITÀ / DECLARE UNDER MY OWN RESPONSIBIITY I miei dati anagrafici / My personal data: Nome/Name …………...…………..…….…………, Cognome/Surname ..………………...……….……….., nato a/born in ………………………………………..…………..………………… il/on ……/……/………… cittadinanza/ citizenship ………………………….. residenza/ city of residency ….…………..………..…….. via/ address …………………….………………….… n.…..… CAP/Post code. ……… … Prov. ……..…..… I dati relativi al mio percorso formativo/ data relating to my training path1: (autocertificazione LAUREA/DIPLOMA UNIVERSITARIO) ho superato presso la Facoltà di / (self-certification MASTER”S/UNIVERSITY DEGREE) completed at the Faculty of ………………………………..…….………… …………………….……… dell'Ateneo di/of the University of ………………….……………………………… l'esame/prova finale nel corso di/the final exam in the course of - (laurea, diploma universitario, laurea specialistica, laurea specialistica a ciclo unico, laurea magistrale, laurea magistrale a ciclo unico) / (bachelor degree, specialist degree, single -cycle specialist degree, master’s degree, single-cycle master’s degree)2 in……………….…...……… …………………………... classe/ year ……………..………………….. nel giorno/ on the day ..……/…../….……. con voto/punteggio/with