Meeting Packet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Meeting Packet Page 1
South Carolina House of Representatives Legislative Oversight Committee Wednesday, June 30, 2021 at 9:00 a.m. in Room 110 - Blatt Building The meeting will stream online and be archived. A link to the stream can be accessed at https://scstatehouse.gov/. Ad Hoc Committee Review of the State Election Commission’s process for maintaining the accuracy of voter rolls with regards to qualified electors, including but not limited to, removing deceased people from the state’s active voter registration list Rep. Wm. Weston J. Newton (Chair) Rep. Joseph H. Jefferson, Jr. Rep. Kambrell H. Garvin Rep. Rosalyn D. Henderson-Myers Rep. William M. “Bill” Hixon Rep. Timothy A. “Tim” McGinnis Rep. Adam M. Morgan Rep. Russell L. Ott Rep. John Taliaferro “Jay” West AGENDA – PUBLIC INPUT OPPORTUNITY I. Discussion of ad hoc committee administrative matters II. Opportunity for public input about the State Election Commission’s process for maintaining the accuracy of voter rolls with regards to qualified electors, including but not limited to, removing deceased people from the state’s active voter registration list MEETING PROTOCOL: To provide testimony, you must register in advance no later than 9:00 a.m. on June 28, 2021. Click here to register online. o Registration asks for the name and contact information for the individual providing testimony. Testimony may be provided via digital means upon request in the registration. Click here for general information about providing testimony to the Committee. o Please plan to limit comments to three minutes. o Members may ask questions about your testimony. An ongoing opportunity to submit anonymous public input is available on the Committee’s website by clicking here. -
Legislative Update Debbie Elmore Director of Governmental Relations and Communication
South Carolina School Boards Association LegisLATIVE update Debbie Elmore Director of Governmental Relations and Communication inside Top legislative priorities, position statements and talking points K12 funding / Education funding reform ............1 School safety ....................................3 School bus safety .............................5 School start date ..............................5 Retired teacher salary cap ..............6 South Carolina legislators ................7 LEGISLATIVE update Top legislative priorities, position statements and talking points K12 funding/Education leases/purchases. In addition, transportation funding was transferred from the EIA to the funding reform General Fund. (SCSBA legislative priority) • $11 million to assist low performing schools With a projection of about $292 million in identified under the new accountability additional General Fund revenues and an system. (Note: The number of low performing estimated $39 million growth in Education schools is expected to double under the Improvement Act (EIA) funds, the prospect new system. $11 million is nearly half of the of tackling education funding reform this S.C. Department of Education’s (SCDE) legislative session is highly unlikely. budget request of $24 million.) The House Ways and Means Committee • $5 million to increase the starting teacher wrapped up its work February 22 to finalize its $8 annual salary from $30,000 to $32,000. billion state spending plan that, among other • $3 million for industrial credentials/ things, directs school districts to provide a two certification. percent teacher pay raise but adds no increase • $2 million for career and technology centers. in funding for the Base Student Cost (BSC). • $4.5 million for the Education Oversight Highlights of allocations for K12 education are Committee Partnerships for Innovation. -

Education and Public Works Committee H
Merita A. “Rita” Allison Ronnie Young Chairman Robert L. Brown First Vice Chairman Second Vice Chairman Education and Public Works Committee H. Pierce McNair, Jr. Richard P. Fulmer Director of Research Staff Attorney Terry Alexander Jerry N. Govan, Jr. Linda “Lin” Bennett Steven W. Long Wendy C. Brawley Timothy A. “Tim” McGinnis Paula R. Calhoon Tommy M. Stringer Converse A.“Con” Chellis, IV Bill Taylor Bobby J. Cox Ivory T. Thigpen Raye Felder South Carolina House of Representatives Christopher S. “Chris” Wooten P.O. Box 11867 Richard L. “Richie” Yow Virginia “Ginger” Lee Telephone: (803) 734-3053 Fax: (803) 734-2827 Lillian E. Hayes Executive Assistant Columbia, S.C. 29211 Research Analyst Room 429, Blatt Building TRANSPORTATION SUBCOMMITTEE MEETING NOTICE TUESDAY, FEBRUARY 4, 2020 IMMEDIATELY UPON ADJOURNMENT OF THE HOUSE ROOM 433, SOLOMON BLATT BUILDING The Subcommittee will consider the following bills: H. 3358 -- Reps. Yow, Thayer and Hewitt: A BILL TO AMEND THE CODE OF LAWS OF SOUTH CAROLINA, 1976, BY ADDING SECTION 57-23-810 SO AS TO PROVIDE THAT THE DEPARTMENT OF TRANSPORTATION SHALL REQUIRE A COMPANY THAT ENTERS INTO A CONTRACT TO MOW VEGETATION ALONG A DEPARTMENT-MAINTAINED HIGHWAY TO DISPOSE OF ALL TRASH AND OTHER DEBRIS FOUND ALONG THE HIGHWAY BEFORE THE VEGETATION IS MOWED. H. 4694 -- Reps. Allison, Clyburn and Hosey: A BILL TO AMEND SECTION 59-67-210, CODE OF LAWS OF SOUTH CAROLINA, 1976, RELATING TO THE UNLAWFUL PASSING OF A SCHOOL BUS BY ANOTHER SCHOOL BUS, SO AS TO PROVIDE THAT A SCHOOL BUS MAY LAWFULLY PASS ANOTHER SCHOOL BUS ON A MULTILANE HIGHWAY; AND TO REPEAL SECTION 59-67-515 RELATING TO SPEED LIMITS FOR PUBLIC SCHOOL BUSES. -

2020 Silver Elephant Dinner
SOUTH CAROLINA REPUBLICAN PARTY THE ROAD TO THE WHITE HOUSE 53rd ANNUAL SILVER ELEPHANT PRE-RECEPTION SOUTH CAROLINA REPUBLICAN PARTY THE ROAD TO THE WHITE HOUSE 53rd ANNUAL SILVER ELEPHANT GUEST SOUTH CAROLINA REPUBLICAN PARTY THE ROAD TO THE WHITE HOUSE 53rd ANNUAL SILVER ELEPHANT STAFF SOUTH CAROLINA REPUBLICAN PARTY THE ROAD TO THE WHITE HOUSE 53rd ANNUAL SILVER ELEPHANT PRESS SOUTH CAROLINA REPUBLICAN PARTY THE ROAD TO THE WHITE HOUSE 53RD ANNUAL SILVER ELEPHANT DINNER • 2020 FTS-SC-RepParty-2020-SilverElephantProgram.indd 1 9/8/20 9:50 AM never WELCOME CHAIRMAN DREW MCKISSICK Welcome to the 2020 Silver Elephant Gala! For 53 years, South Carolina Republicans have gathered together each year to forget... celebrate our party’s conservative principles, as well as the donors and activists who help promote those principles in our government. While our Party has enjoyed increasing success in the years since our Elephant Club was formed, we always have to remember that no victories are ever perma- nent. They are dependent on our continuing to be faithful to do the fundamen- tals: communicating a clear conservative message that is relevant to voters, identifying and organizing fellow Republicans, and raising the money to make it all possible. As we gather this evening on the anniversary of the tragic terrorists attacks on our homeland in 2001, we’re reminded about what’s at stake in our elections this year - the protection of our families, our homes, our property, our borders and our fundamental values. This year’s election offers us an incredible opportunity to continue to expand our Party. -
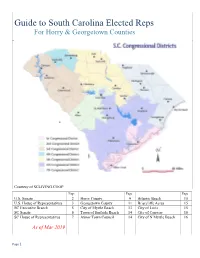
Guide to South Carolina Elected Reps for Horry & Georgetown Counties
Guide to South Carolina Elected Reps For Horry & Georgetown Counties Courtesy of SCLIVING.COOP Page Page Page U.S. Senate 2 Horry County 9 Atlantic Beach 15 U.S. House of Representatives 3 Georgetown County 11 Briarcliffe Acres 15 SC Executive Branch 5 City of Myrtle Beach 13 City of Loris 15 SC Senate 6 Town of Surfside Beach 14 City of Conway 16 SC House of Representatives 7 Aynor Town Council 14 City of N Myrtle Beach 16 As of Mar 2019 Page 1 U.S. Senate The Senate is composed of two senators from each state, elected by voters, for six-year terms. U. S. Senate Lindsey Graham [R] South Carolina 3rd 6-year ends Jan 2021 290 Russell Senate Office Building Served U.S. Senate since Washington, DC 20510-4001 2003 Phone: (202) 224-5972 Served U.S. House 1995- 2003 McMillan Federal Bldg 401 West Evans St, Suite 111 Committee Assignments: Florence SC 29501 -Appropriations 843-669-1505 -Foreign Relations -Budget 530 Johnnie Dodds Blvd, Suite 202 -Judiciary Chair Mt Pleasant SC 29464 843-849-3887 Website: lgraham.senate.gov Tim Scott [R] U. S. Senate Began Jan 2013; ends Jan 717 Hart Senate Office Building 2023 Washington, DC 20510 South Carolina Served U.S. House 2011- (202) 224-6121 2013 1901 Main St, Suite 1425 Committee Assignments: Columbia, SC 29201 (803) 771-6112x2500 -Finance Committee -Banking, Housing, Urban 2500 City Hall Lane, 3rd Floor Suite Affairs North Charleston, SC 29406 -Health, Education, Labor (843) 727-4525 & Pensions -Small Business & Website: www.scott.senate.gov Entrepreneurship -Aging Page 2 U.S. -

The General Assembly of South Carolina 124Th Session List of Members
THE GENERAL ASSEMBLY OF SOUTH CAROLINA 124TH SESSION LIST OF MEMBERS FIRST REGULAR SESSION Convening Tuesday, January 12, 2021 in Columbia (CORRECTED TO DECEMBER 31, 2020) Published by: Charles F. Reid, Clerk South Carolina House of Representatives Members of the 124th General Assembly of South Carolina The Senate 30 Republicans, 16 Democrats, Total 46. All Senators elected in 2020 to serve until Monday after the General Election in November of 2024. Pursuant to Section 2-1-60 of the 1976 Code, as last amended by Act 513 of 1984, Senators are elected from 46 single member districts. [D] after the name indicates Democrat and [R] indicates Republican. Explanation of Reference Marks ✶ Indicates 2020 Senators re-elected . 40 Without previous legislative service (unmarked) . 6 Vacancies . 0 Total Membership 2020-2024 . 46 Information Telephones President's Office . (803) 212-6430 President Pro Tempore Emeritus' Office (111 Gressette Bldg.). (803) 212-6455 Clerk's Office (401 Gressette Bldg.) . (803) 212-6200 (1st Floor, State House) . (803) 212-6700 Agriculture & Natural Resources Com. (402 Gressette Bldg.) . (803) 212-6230 Banking & Insurance Com. (410 Gressette Bldg.) . (803) 212-6240 Bookkeeping (534 Brown Bldg.) . (803) 212-6550 Corrections & Penology Com. (211 Gressette Bldg.) . (803) 212-6420 Education Com. (404 Gressette Bldg.) . (803) 212-6250 Ethics Com. (205 Gressette Bldg.) . (803) 212-6410 Family and Veterans' Services (303 Gressette Bldg.) . (803) 212-6320 Finance Com. (111 Gressette Bldg.) . (803) 212-6640 Fish, Game & Forestry Com. (305 Gressette Bldg.) . (803) 212-6340 Health Care (Nurse) (511-B Gressette Bldg.) . (803) 212-6175 Interstate Cooperation Com. (213 Gressette Bldg.) . -

Senate Filings March 30.Xlsx
SC ALLIANCE TO FIX OUR ROADS 2020 SENATE FILINGS APRIL 2, 2020 District Counties Served First (MI) Last / Suffix Party Primary Election General Election 1 OCONEE,PICKENS Thomas C Alexander Republican unopposed unopposed 2 PICKENS Rex Rice Republican unopposed unopposed Craig Wooten Republican Richard Cash* (R) Winner of Republican Primary 3 ANDERSON Richard Cash Republican Craig Wooten (R) Judith Polson (D) Judith Polson Democrat Mike Gambrell Republican Mike Gambrell* (R) 4 ABBEVILLE,ANDERSON,GREENWOOD Jose Villa (D) Jose Villa Democrat Tom Corbin Republican Tom Corbin* (R) Winner of Republican Primary 5 GREENVILLE,SPARTANBURG Dave Edwards (R) Michael McCord (D) Michael McCord Democrat Dave Edwards Republican Dwight A Loftis Republican Dwight Loftis* (R) 6 GREENVILLE Hao Wu (D) Hao Wu Democrat Karl B Allen Democrat Karl Allen* (D) Winner of Democratic Primary 7 GREENVILLE Fletcher Smith Democrat Fletcher Smith (D) Jack Logan (R) Jack Logan Republican Ross Turner Republican Ross Turner* (R) 8 GREENVILLE Janice Curtis (R) Janice S Curtis Republican 9 GREENVILLE,LAURENS Danny Verdin Republican unopposed unopposed Floyd Nicholson Democrat Bryan Hope (R) Winner of Republican Primary 10 ABBEVILLE,GREENWOOD,MCCORMICK,SALUDA Bryan Hope Republican Billy Garrett (R) Floyd Nicholson*(D) Billy Garrett Republican Josh Kimbrell Republican Glenn Reese* (D) 11 SPARTANBURG Glenn Reese Democrat Josh Kimbrell (R) Scott Talley Republican Scott Talley*(R) Winner of Republican Primary 12 GREENVILLE,SPARTANBURG Mark Lynch Republican Mark Lynch (R) Dawn Bingham -

JOURNAL of the HOUSE of REPRESENTATIVES of the STATE
NO. 29 JOURNAL of the HOUSE OF REPRESENTATIVES of the STATE OF SOUTH CAROLINA REGULAR SESSION BEGINNING TUESDAY, JANUARY 8, 2019 ________ TUESDAY, MARCH 3, 2020 (STATEWIDE SESSION) TUESDAY, MARCH 3, 2020 Indicates Matter Stricken Indicates New Matter The House assembled at 12:00 noon. Deliberations were opened with prayer by Rev. Charles E. Seastrunk, Jr., as follows: Our thought for today is from 1 Corinthians 1:4: “I give thanks to my God always for you because of the grace of God.” Let us pray. God of Grace and Glory, come to us today and lead these Representatives and staff to do the great things planned for them. Keep them in Your care this week as they continue the work set before them. Bless our defenders of freedom and first responders as they protect and care for us. Bless our Nation, President, State, Governor, Speaker, staff, and all who give of their time and talents to this great cause. Heal the wounds, those seen and those hidden of our brave warriors who suffer and sacrifice for our freedom. Lord, in Your mercy, hear our prayers. Amen. Pursuant to Rule 6.3, the House of Representatives was led in the Pledge of Allegiance to the Flag of the United States of America by the SPEAKER. After corrections to the Journal of the proceedings of Friday, the SPEAKER ordered it confirmed. MOTION ADOPTED Rep. KING moved that when the House adjourns, it adjourn in memory of Kevin Caldwell, which was agreed to. SILENT PRAYER The House stood in silent prayer for the family and friends of Bobby Bowers. -

April 12, 2018 2DAC Handout
TWO DAYS @ THE CAPITOL april 12, 2018 inside Steps to take before you arrive ........1 Meeting location, logistics ...............1 Agenda .............................................1 Map ...................................................2 Top legislative priorities, position statements and talking points new location! K12 funding / Education funding reform ............3 Columbia Metropolitan Fiscal accountability revisions .........7 Convention Center School safety ....................................8 (See map on page 2) School bus safety .............................9 School start date ..............................9 Retired teacher salary cap ............10 #sc2dac South Carolina legislators ..............11 SCSBA looks forward to seeing you Thursday As a school board member, administrator or a local public school advocate, your presence at the State House standing up for public schools makes a difference. Leaders of local school districts, school board members and administrators know best the impact state policy proposals can have on their schools. To help prepare for discussions with lawmakers on Thursday, this handout provides information on the legislative issues you will be discussing with your legislators. Each issue includes an overview, position statement and talking points. Please note that legislation can change quickly as it moves through the process. SCSBA will be sure to pass along any changes or updates. #sc2dac TWO DAYS @ THE CAPITOL Before you arrive State House visits 1. Contact members of your legislative delegation After the morning’s legislative briefing, to arrange a meeting between 10:30 a.m. and participants will head to the State House (see 11:45 a.m. at the State House. map of State House complex) and have a little 2. Study the legislative issues, position statements more than one hour to meet with legislators and talking points to prepare for your meetings and attend any scheduled committee with legislators. -

Legislative Oversight Committee
Chair Wm. Weston J. Newton First Vice-Chair: Joseph H. Jefferson, Jr. Legislative Oversight Committee Kambrell H. Garvin Gil Gatch Rosalyn D. Henderson- William M. “Bill” Hixon Myers Kimberly O. Johnson Jeffrey E. “Jeff” Johnson Josiah Magnuson John R. McCravy, III Timothy A. “Tim” McGinnis Adam M. Morgan Travis A. Moore Melissa Lackey Oremus Russell L. Ott Marvin R. Pendarvis Michael F. Rivers, Sr. Tommy M. Stringer South Carolina House of Representatives John Taliaferro (Jay) West, IV Chris Wooten Post Office Box 11867 Charles L. Appleby, IV Jennifer L. Dobson Legal Counsel Research Director Columbia, South Carolina 29211 Telephone: (803) 212-6810 • Fax: (803) 212- Lewis Carter Cathy A. Greer Research Analyst/Auditor Administration 6811 Coordinator Riley E. McCullough Room 228 Blatt Building Research Analyst Economic Development, Transportation, and Natural Resources Subcommittee Thursday, May 12, 2021 8:30 a.m. Blatt Room 321 Archived Video Available I. Pursuant to House Legislative Oversight Committee Rule 6.8, South Carolina ETV was allowed access for streaming the meeting. You may access an archived video of this meeting by visiting the South Carolina General Assembly’s website (http://www.scstatehouse.gov) and clicking on Committee Postings and Reports, then under House Standing Committees click on Legislative Oversight. Then, click on Video Archives for a listing of archived videos for the Committee. Attendance I. The Economic Development, Transportation, and Natural Resources Subcommittee meeting was called to order by Chairman William M. (Bill) Hixon, on Thursday, May 12, 2021, in Room 321 of the Blatt Building. The following members of the Subcommittee were present for either all or a portion of the meeting: Chairman Hixon, Representative Russell L. -

Education and Public Works Committee H
Merita A. “Rita” Allison Ronnie Young Chairman Robert L. Brown First Vice Chairman Second Vice Chairman Education and Public Works Committee H. Pierce McNair, Jr. Richard P. Fulmer Director of Research Staff Attorney Terry Alexander Jerry N. Govan, Jr. Linda “Lin” Bennett Steven W. Long Wendy C. Brawley Timothy A. “Tim” McGinnis Paula R. Calhoon Tommy M. Stringer Converse A.“Con” Chellis, IV Bill Taylor Bobby J. Cox Ivory T. Thigpen Raye Felder South Carolina House of Representatives Christopher S. “Chris” Wooten P.O. Box 11867 Richard L. “Richie” Yow Virginia “Ginger” Lee Telephone: (803) 734-3053 Fax: (803) 734-2827 Lillian E. Hayes Executive Assistant Columbia, S.C. 29211 Research Analyst Room 429, Blatt Building K-12 SUBCOMMITTEE MEETING NOTICE WEDNESDAY, APRIL 24, 2019 AT 2 HOURS UPON ADJOURNMENT ROOM 433, SOLOMON BLATT BUILDING The Subcommittee will consider the following bills: H. 4403 -- Reps. Bennett and Brown: A BILL TO AMEND SECTION 59-63-120, CODE OF LAWS OF SOUTH CAROLINA, 1976, RELATING TO BULLYING PROHIBITION POLICIES ADOPTED BY SCHOOL DISTRICTS, SO AS TO PROVIDE PROCEDURES FOR RESPONDING TO AND REMEDIATING ALLEGATIONS OF BULLYING, TO REQUIRE AN APPEALS PROCEDURE, AND TO PROVIDE CERTAIN ADDITIONAL REQUIREMENTS OF SCHOOL DISTRICTS AND THE SUPERINTENDENT OF EDUCATION. H. 3199 -- Reps. Govan and Clyburn: A BILL TO AMEND SECTION 59-29-410, CODE OF LAWS OF SOUTH CAROLINA, 1976, RELATING TO INSTRUCTIONAL TOPICS REQUIRED IN HIGH SCHOOL FINANCIAL LITERACY PROGRAMS, SO AS TO ALSO REQUIRE INSTRUCTION ON THE TOPICS OF COLLEGE AND EDUCATION LOANS, KEY LOAN TERMS, MONTHLY PAYMENT OBLIGATIONS, REPAYMENT OPTIONS, CREDIT, AND EDUCATION LOAN DEBT. -
List of Members of the South Carolina General Assembly
THE GENERAL ASSEMBLY OF SOUTH CAROLINA 124TH SESSION LIST OF MEMBERS FIRST REGULAR SESSION Convening Tuesday, January 12, 2021 in Columbia (CORRECTED TO SEPTEMBER 24, 2021) Published by: Charles F. Reid, Clerk South Carolina House of Representatives Members of the 124th General Assembly of South Carolina The Senate 30 Republicans, 16 Democrats, Total 46. All Senators elected in 2020 to serve until Monday after the General Election in November of 2024. Pursuant to Section 2-1-60 of the 1976 Code, as last amended by Act 513 of 1984, Senators are elected from 46 single member districts. [D] after the name indicates Democrat and [R] indicates Republican. Explanation of Reference Marks ✶ Indicates 2020 Senators re-elected . 40 Without previous legislative service (unmarked) . 6 Vacancies . 0 Total Membership 2020-2024 . 46 Information Telephones President's Office . (803) 212-6430 President Pro Tempore Emeritus' Office (111 Gressette Bldg.). (803) 212-6455 Clerk's Office (401 Gressette Bldg.) . (803) 212-6200 (1st Floor, State House) . (803) 212-6700 Agriculture & Natural Resources Com. (402 Gressette Bldg.) . (803) 212-6230 Banking & Insurance Com. (410 Gressette Bldg.) . (803) 212-6240 Bookkeeping (534 Brown Bldg.) . (803) 212-6550 Corrections & Penology Com. (211 Gressette Bldg.) . (803) 212-6420 Education Com. (404 Gressette Bldg.) . (803) 212-6250 Ethics Com. (205 Gressette Bldg.) . (803) 212-6410 Family and Veterans' Services (303 Gressette Bldg.) . (803) 212-6320 Finance Com. (111 Gressette Bldg.) . (803) 212-6640 Fish, Game & Forestry Com. (305 Gressette Bldg.) . (803) 212-6340 Health Care (Nurse) (511-B Gressette Bldg.) . (803) 212-6175 Interstate Cooperation Com. (213 Gressette Bldg.) .