Diseases of the Circulatory System (I00-I99) ICD-10-CM
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Effect of Captopril on Post-Infarction Remodelling Visualized by Light
www.nature.com/scientificreports OPEN Efect of captopril on post‑infarction remodelling visualized by light sheet microscopy and echocardiography Urmas Roostalu1*, Louise Thisted1, Jacob Lercke Skytte1, Casper Gravesen Salinas1, Philip Juhl Pedersen1, Jacob Hecksher‑Sørensen1, Bidda Rolin1,3, Henrik H. Hansen1, James G. MacKrell2, Robert M. Christie2, Niels Vrang1, Jacob Jelsing1 & Nora Elisabeth Zois1 Angiotensin converting enzyme inhibitors, among them captopril, improve survival following myocardial infarction (MI). The mechanisms of captopril action remain inadequately understood due to its diverse efects on multiple signalling pathways at diferent time periods following MI. Here we aimed to establish the role of captopril in late‑stage post‑MI remodelling. Left anterior descending artery (LAD) ligation or sham surgery was carried out in male C57BL/6J mice. Seven days post‑surgery LAD ligated mice were allocated to daily vehicle or captopril treatment continued over four weeks. To provide comprehensive characterization of the changes in mouse heart following MI a 3D light sheet imaging method was established together with automated image analysis workfow. The combination of echocardiography and light sheet imaging enabled to assess cardiac function and the underlying morphological changes. We show that delayed captopril treatment does not afect infarct size but prevents left ventricle dilation and hypertrophy, resulting in improved ejection fraction. Quantifcation of lectin perfused blood vessels showed improved vascular density in the infarct border zone in captopril treated mice in comparison to vehicle dosed control mice. These results validate the applicability of combined echocardiographic and light sheet assessment of drug mode of action in preclinical cardiovascular research. Although timely primary coronary percutaneous intervention has substantially improved patient survival post myocardial infarction (MI), the ofen-concomitant cardiac dysfunction and heart failure afect a signifcant num- ber of patients. -

The Pulmonary Manifestations of Left Heart Failure*
The Pulmonary Manifestations of Left Heart Failure* Brian K. Gehlbach, MD; and Eugene Geppert, MD Determining whether a patient’s symptoms are the result of heart or lung disease requires an understanding of the influence of pulmonary venous hypertension on lung function. Herein, we describe the effects of acute and chronic elevations of pulmonary venous pressure on the mechanical and gas-exchanging properties of the lung. The mechanisms responsible for various symptoms of congestive heart failure are described, and the significance of sleep-disordered breathing in patients with heart disease is considered. While the initial clinical evaluation of patients with dyspnea is imprecise, measurement of B-type natriuretic peptide levels may prove useful in this setting. (CHEST 2004; 125:669–682) Key words: Cheyne-Stokes respiration; congestive heart failure; differential diagnosis; dyspnea; pulmonary edema; respiratory function tests; sleep apnea syndromes Abbreviations: CHF ϭ congestive heart failure; CSR-CSA ϭ Cheyne-Stokes respiration with central sleep apnea; CPAP ϭ continuous positive airway pressure; Dlco ϭ diffusing capacity of the lung for carbon monoxide; DM ϭ membrane conductance; FRC ϭ functional residual capacity; OSA ϭ obstructive sleep apnea; TLC ϭ total lung ϭ ˙ ˙ ϭ capacity; VC capillary volume; Ve/Vco2 ventilatory equivalent for carbon dioxide early 5 million Americans have congestive heart For a detailed review of the pathophysiology of N failure (CHF), with 400,000 new cases diag- high-pressure pulmonary edema, the reader is re- nosed each year.1 Unfortunately, despite the consid- ferred to several excellent recent reviews.2–4 erable progress that has been made in understanding the pathophysiology of pulmonary edema, the pul- monary complications of this condition continue to The Pathophysiology of Pulmonary challenge the bedside clinician. -

Percutaneous Mitral Valve Therapies: State of the Art in 2020 LA ACP Annual Meeting
Percutaneous Mitral Valve Therapies: State of the Art in 2020 LA ACP Annual Meeting Steven R Bailey MD MSCAI, FACC, FAHA,FACP Professor and Chair, Department of Medicine Malcolm Feist Chair of Interventional Cardiology LSU Health Shreveport Professor Emeritus, UH Health San Antonio [email protected] SRB March 2020 Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship Company • Grant/Research Support • None • Consulting Fees/Honoraria • BSCI, Abbot DSMB • Intellectual Property Rights • UTHSCSA • Other Financial Benefit • CCI Editor In Chief SRB March 2020 The 30,000 Ft View Maria SRB March 2020 SRB March 2020 Mitral Stenosis • The most common etiology of MS is rheumatic fever, with a latency of approximately 10 to 20 years after the initial streptococcal infection. Symptoms usually appear in adulthood • Other etiologies are rare but include: congenital MS radiation exposure atrial myxoma mucopolysaccharidoses • MS secondary to calcific annular disease is increasingly seen in elderly patients, and in patients with advanced chronic kidney disease. SRB March 2020 Mitral Stenosis • Mitral stenosis most commonly results from rheumatic heart disease fusion of the valve leaflet cusps at the commissures thickening and shortening of the chordae calcium deposition within the valve leaflets • Characteristic “fish-mouth” or “hockey stick” appearance on the echocardiogram (depending on view) SRB March 2020 Mitral Stenosis: Natural History • The severity of symptoms depends primarily on the degree of stenosis. • Symptoms often go unrecognized by patient and physician until significant shortness of breath, hemoptysis, or atrial fibrillation develops. -
Currentstateofknowledgeonaetiol
European Heart Journal (2013) 34, 2636–2648 ESC REPORT doi:10.1093/eurheartj/eht210 Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases Downloaded from Alida L. P. Caforio1†*, Sabine Pankuweit2†, Eloisa Arbustini3, Cristina Basso4, Juan Gimeno-Blanes5,StephanB.Felix6,MichaelFu7,TiinaHelio¨ 8, Stephane Heymans9, http://eurheartj.oxfordjournals.org/ Roland Jahns10,KarinKlingel11, Ales Linhart12, Bernhard Maisch2, William McKenna13, Jens Mogensen14, Yigal M. Pinto15,ArsenRistic16, Heinz-Peter Schultheiss17, Hubert Seggewiss18, Luigi Tavazzi19,GaetanoThiene4,AliYilmaz20, Philippe Charron21,andPerryM.Elliott13 1Division of Cardiology, Department of Cardiological Thoracic and Vascular Sciences, University of Padua, Padova, Italy; 2Universita¨tsklinikum Gießen und Marburg GmbH, Standort Marburg, Klinik fu¨r Kardiologie, Marburg, Germany; 3Academic Hospital IRCCS Foundation Policlinico, San Matteo, Pavia, Italy; 4Cardiovascular Pathology, Department of Cardiological Thoracic and Vascular Sciences, University of Padua, Padova, Italy; 5Servicio de Cardiologia, Hospital U. Virgen de Arrixaca Ctra. Murcia-Cartagena s/n, El Palmar, Spain; 6Medizinische Klinik B, University of Greifswald, Greifswald, Germany; 7Department of Medicine, Heart Failure Unit, Sahlgrenska Hospital, University of Go¨teborg, Go¨teborg, Sweden; 8Division of Cardiology, Helsinki University Central Hospital, Heart & Lung Centre, -

View Pdf Copy of Original Document
Phenotype definition for the Vanderbilt Genome-Electronic Records project Identifying genetics determinants of normal QRS duration (QRSd) Patient population: • Patients with DNA whose first electrocardiogram (ECG) is designated as “normal” and lacking an exclusion criteria. • For this study, case and control are drawn from the same population and analyzed via continuous trait analysis. The only difference will be the QRSd. Hypothetical timeline for a single patient: Notes: • The study ECG is the first normal ECG. • The “Mildly abnormal” ECG cannot be abnormal by presence of heart disease. It can have abnormal rate, be recorded in the presence of Na-channel blocking meds, etc. For instance, a HR >100 is OK but not a bundle branch block. • Y duration = from first entry in the electronic medical record (EMR) until one month following normal ECG • Z duration = most recent clinic visit or problem list (if present) to one week following the normal ECG. Labs values, though, must be +/- 48h from the ECG time Criteria to be included in the analysis: Criteria Source/Method “Normal” ECG must be: • QRSd between 65-120ms ECG calculations • ECG designed as “NORMAL” ECG classification • Heart Rate between 50-100 ECG calculations • ECG Impression must not contain Natural Language Processing (NLP) on evidence of heart disease concepts (see ECG impression. Will exclude all but list below) negated terms (e.g., exclude those with possible, probable, or asserted bundle branch blocks). Should also exclude normalization negations like “LBBB no longer present.” -

Incomplete Versus Complete Myocardial Infarction
Henry Ford Hospital Medical Journal Volume 39 Number 3 Article 20 9-1991 Incomplete Versus Complete Myocardial Infarction Mihai Gheorghiade Sidney Goldstein Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Gheorghiade, Mihai and Goldstein, Sidney (1991) "Incomplete Versus Complete Myocardial Infarction," Henry Ford Hospital Medical Journal : Vol. 39 : No. 3 , 263-264. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol39/iss3/20 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. Incomplete Versus Complete Myocardial Infarction Mihai Gheorghiade, MD,* and Sidney Goldstein, MD* Incomplete myocardial infarction (MI), when compared with a complete Ml. is characterized by a small infarct size and a large mass of viable hut jeopardized myocardium within the perfusion zone of the infarct-related vessel that is manifested ctinicalty hy early recurrent infarction. The pathophysiology involves earty spontaneous or thrombolytic reperfusion. Clinical (i.e., residual ischemia), electrocardiographic, and echocardiographic findings and magnitude of serum cardiac enzyme elevatitms should be taken into account in diagnosing an incomplete Ml. (Heniy Ford Hosp MedJ 1991;39:263-4) he observation that the ischemic event associated with on the ECG may not properly identify patients with incomplete Tthrombotic occlusion of the coronary artery can be inter infarction. rupted with thrombolytic therapy has led to the recognition of a When applied to the individual patient, it is therefore more new ischemic syndrome, the incomplete myocardial infarction useful to divide postinfarction patients, regardless of whether or (MI) (1). -
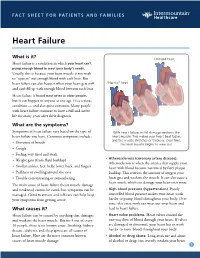
Heart Failure
FACT SHEET FOR PATIENTS AND FAMILIES Heart Failure What is it? Enlarged heart Heart failure is a condition in which your heart can’t pump enough blood to meet your body’s needs. Usually, this is because your heart muscle is too weak to “squeeze” out enough blood with each beat. But heart failure can also happen when your heart gets stiff “Normal” heart and can’t fill up with enough blood between each beat. Heart failure is found most often in older people, but it can happen to anyone at any age. It’s a serious condition — and also quite common. Many people with heart failure continue to have a full and active life for many years after their diagnosis. What are the symptoms? Symptoms of heart failure vary based on the type of With heart failure, initial damage weakens the heart failure you have. Common symptoms include: heart muscle. This makes your heart beat faster, and the muscle stretches or thickens. Over time, • Shortness of breath the heart muscle begins to wear out. • Cough • Feeling very tired and weak • Atherosclerosis (coronary artery disease). • Weight gain (from fluid buildup) Atherosclerosis is when the arteries that supply your • Swollen ankles, feet, belly, lower back, and fingers heart with blood become narrowed by fatty plaque • Puffiness or swelling around the eyes buildup. This restricts the amount of oxygen your • Trouble concentrating or remembering heart gets and weakens the muscle. It can also cause a heart attack, which can damage your heart even more. The main cause of heart failure (heart muscle damage and weakness) cannot be cured, but symptoms can be • High blood pressure (hypertension). -

Heart Disease and Diseases of the Circulatory System in Westchester
Westchester County 2016.01 Department of Health KEEP HEALTHY @wchealthdept AND Community Health Assessment Data Update GET #keephealthy THE STATS Heart Disease and Diseases of the Circulatory System in Westchester In this issue: Heart disease as a Heart disease is the number one cause of death in Westchester County. leading cause of death in Westchester county In 2012, heart disease accounted for 2,113 deaths or 31% of all deaths Deaths due to heart disease across different in the county. Adding in 490 deaths due to stroke and other diseases population and risk of the circulatory system, total deaths from circulatory disease are groups 60% higher than the next leading cause of death - cancer. Hospitalizations due to cardiovascular disease- related conditions, Selected Causes of Death in Westchester County, 2012 including diseases of the heart Emergency room visits 2% 3% 7% due to cardiovascular disease-related 3% conditions Selected risk factors 4% that contribute to Heart Disease, cardiovascular disease 4% in Westchester county 31% 5% 9% Cerebrovascular Jiali Li, Ph.D. Director of Disease (Stroke), Research & Evaluation Neoplasms 5% Planning & Evaluation (Cancer), 24% Other Circulatory, Renee Recchia, MPH 3% Acting Deputy Commissioner of Administration Heart Disease Cerebrovascular Disease (Stroke) Project Staff: Other Circulatory Neoplasms (Cancer) Bonnie Lam, MPH Respiratory Diseases External Causes (e.g. accidents) Medical Data Analyst Communicable Diseases Nervous System Diseases Milagros Venuti, MPA Digestive System Diseases -

ST-Elevation Myocardial Infarction Due to Acute Thrombosis in an Adolescent with COVID-19
Prepublication Release ST-Elevation Myocardial Infarction Due to Acute Thrombosis in an Adolescent With COVID-19 Jessica Persson, MD, Michael Shorofsky, MD, Ryan Leahy, MD, MS, Richard Friesen, MD, Amber Khanna, MD, MS, Lyndsey Cole, MD, John S. Kim, MD, MS DOI: 10.1542/peds.2020-049793 Journal: Pediatrics Article Type: Case Report Citation: Persson J, Shorofsky M, Leahy R, et al. ST-elevation myocardial infarction due to acute thrombosis in an adolescent with COVID-19. Pediatrics. 2021; doi: 10.1542/peds.2020- 049793 This is a prepublication version of an article that has undergone peer review and been accepted for publication but is not the final version of record. This paper may be cited using the DOI and date of access. This paper may contain information that has errors in facts, figures, and statements, and will be corrected in the final published version. The journal is providing an early version of this article to expedite access to this information. The American Academy of Pediatrics, the editors, and authors are not responsible for inaccurate information and data described in this version. Downloaded from©202 www.aappublications.org/news1 American Academy by of guest Pediatrics on September 27, 2021 Prepublication Release ST-Elevation Myocardial Infarction Due to Acute Thrombosis in an Adolescent With COVID-19 Jessica Persson, MD1, Michael Shorofsky, MD1, Ryan Leahy, MD, MS1, Richard Friesen, MD1, Amber Khanna, MD, MS1,2, Lyndsey Cole, MD3, John S. Kim, MD, MS1 1Division of Cardiology, Department of Pediatrics, University of Colorado School of Medicine, Aurora, Colorado 2Division of Cardiology, Department of Medicine, University of Colorado School of Medicine, Aurora, Colorado 3Section of Infectious Diseases, Department of Pediatrics, University of Colorado School of Medicine, Aurora, Colorado Corresponding Author: John S. -

Early Outcomes of Percutaneous Pulmonary Valve Implantation with Pulsta and Melody Valves: the First Report from Korea
Journal of Clinical Medicine Article Early Outcomes of Percutaneous Pulmonary Valve Implantation with Pulsta and Melody Valves: The First Report from Korea Ah Young Kim 1,2 , Jo Won Jung 1,2, Se Yong Jung 1,2 , Jae Il Shin 1,2 , Lucy Youngmin Eun 1,2 , Nam Kyun Kim 3 and Jae Young Choi 1,2,* 1 Division of Pediatric Cardiology, Center for Congenital Heart Disease, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul 03722, Korea; [email protected] (A.Y.K.); [email protected] (J.W.J.); [email protected] (S.Y.J.); [email protected] (J.I.S.); [email protected] (L.Y.E.) 2 Department of Pediatrics, Yonsei University College of Medicine, Seoul 03722, Korea 3 Department of Pediatrics, Emory University, Atlanta, GA 30322, USA; [email protected] * Correspondence: [email protected] Received: 25 July 2020; Accepted: 24 August 2020; Published: 26 August 2020 Abstract: Percutaneous pulmonary valve implantation (PPVI) is used to treat pulmonary stenosis (PS) or pulmonary regurgitation (PR). We described our experience with PPVI, specifically valve-in-valve transcatheter pulmonary valve replacement using the Melody valve and novel self-expandable systems using the Pulsta valve. We reviewed data from 42 patients undergoing PPVI. Twenty-nine patients had Melody valves in mostly bioprosthetic valves, valved conduits, and homografts in the pulmonary position. Following Melody valve implantation, the peak right ventricle-to-pulmonary artery gradient decreased from 51.3 11.5 to 16.7 3.3 mmHg and right ventricular systolic pressure ± ± fell from 70.0 16.8 to 41.3 17.8 mmHg. -

Myocardial Infarction Does Not Accelerate Atherosclerosis in a Mouse Model of Type 1 Diabetes
Diabetes Volume 69, October 2020 2133 Myocardial Infarction Does Not Accelerate Atherosclerosis in a Mouse Model of Type 1 Diabetes Farah Kramer,1 Amy M. Martinson,2 Thalia Papayannopoulou,3 and Jenny E. Kanter1 Diabetes 2020;69:2133–2143 | https://doi.org/10.2337/db20-0152 In addition to increasing the risk of an initial myocardial observed in response to the acute ischemic event was pos- infarction (MI), diabetes increases the risk of a recur- tulated to be driven by enhanced extramedullary hemato- rent MI. Previous work suggests that an experimental poiesis resulting in increased levels of circulating monocytes MI can accelerate atherosclerosis via monocytosis. To available for recruitment into the nascent atherosclerotic test whether diabetes and experimental MI synergize to lesion, thereby accelerating atherosclerosis (9). accelerate atherosclerosis, we performed ligation of Diabetes accelerates atherosclerosis lesion initiation and the left anterior descending coronary artery to induce progression and hinders lesion regression in response to experimental MI or sham surgery in nondiabetic and dramatic lipid lowering (10–13). Changes in monocyte and diabetic mice with preexisting atherosclerosis. All mice macrophage phenotype are believed to contribute to the COMPLICATIONS fi subjected to experimental MI had signi cantly reduced acceleration of atherosclerosis in diabetes. In both mouse left ventricular function. In our model, in comparisons and human studies, diabetes results in increased macro- with nondiabetic sham mice, neither diabetes nor MI phage accumulation within the artery wall (10,14,15). For resulted in monocytosis. Neither diabetes nor MI led to example, autopsy and atherectomy samples from humans increased atherosclerotic lesion size, but diabetes ac- celerated lesion progression, exemplified by necrotic have shown that lesions from subjects with diabetes have core expansion. -

Cardiovascular Disease: a Costly Burden for America. Projections
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA PROJECTIONS THROUGH 2035 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american table of contents INTRODUCTION ...................................................................................5 ABOUT THIS STUDY ................................................................................................... 6 WHAT IS CVD? ......................................................................................................... 6 Atrial Fibrillation Congestive Heart Failure Coronary Heart Disease High Blood Pressure Stroke PROJECTIONS: PREVALENCE OF CVD .............................................................7 Latest Projections Age, Race, Sex – Differences That Matter PROJECTIONS: COSTS OF CVD ................................................................. 8-11 The Cost Generators: Aging Baby Boomers Medical Costs Breakdown Direct Costs + Indirect Costs RECOMMENDATIONS .............................................................................13-14 Research Prevention Affordable Health Care 3 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american Introduction Cardiovascular disease (CVD) has been the leading killer In addition, CVD has become our nation’s costliest chronic of Americans for decades. In years past, a heart attack disease. In 2014, stroke and heart