Identification of Genes Required for Enzalutamide Resistance in Castration-Resistant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Effect of Temperature Adaptation on the Ubiquitin–Proteasome Pathway in Notothenioid Fishes Anne E
© 2017. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2017) 220, 369-378 doi:10.1242/jeb.145946 RESEARCH ARTICLE The effect of temperature adaptation on the ubiquitin–proteasome pathway in notothenioid fishes Anne E. Todgham1,*, Timothy A. Crombie2 and Gretchen E. Hofmann3 ABSTRACT proliferation to compensate for the effects of low temperature on ’ There is an accumulating body of evidence suggesting that the sub- aerobic metabolism (Johnston, 1989; O Brien et al., 2003; zero Antarctic marine environment places physiological constraints Guderley, 2004). Recently, there has been an accumulating body – on protein homeostasis. Levels of ubiquitin (Ub)-conjugated proteins, of literature to suggest that protein homeostasis the maintenance of – 20S proteasome activity and mRNA expression of many proteins a functional protein pool has been highly impacted by evolution involved in both the Ub tagging of damaged proteins as well as the under these cold and stable conditions. different complexes of the 26S proteasome were measured to Maintaining protein homeostasis is a fundamental physiological examine whether there is thermal compensation of the Ub– process, reflecting a dynamic balance in synthetic and degradation proteasome pathway in Antarctic fishes to better understand the processes. There are numerous lines of evidence to suggest efficiency of the protein degradation machinery in polar species. Both temperature compensation of protein synthesis in Antarctic Antarctic (Trematomus bernacchii, Pagothenia borchgrevinki)and invertebrates (Whiteley et al., 1996; Marsh et al., 2001; Robertson non-Antarctic (Notothenia angustata, Bovichtus variegatus) et al., 2001; Fraser et al., 2002) and fish (Storch et al., 2005). In notothenioids were included in this study to investigate the zoarcid fishes, it has been demonstrated that Antarctic eelpouts mechanisms of cold adaptation of this pathway in polar species. -

Supplementary Materials
Supplementary Materials Identification of Compounds The connectivity map concept (C-Map) is based on gene expression profiles, also known as gene fingerprints, and is used to analyze similar effects of compounds and to find drugs for treating diseases [1]. The gene expression profiles in both the C-Map and the CLUE [2] websites were derived from the treatment of human cells with thousands of drugs. Therefore, the gene expression signatures of interest in any induced or organic cell state could be compared with one another to determine similar mechanisms or reverse signatures of drugs and shRNA. Pattern-matching algorithms were used to score each gene expression profile and provide strength of enrichment through query signatures. The results were ranked by “connectivity score (τ)”; a positive score of a signature denoted a similar effect, whereas a negative score indicated a contrary effect. A τ of 90 indicated that only 10% of all perturbations exhibited strong connectivity to the query [2]. Methodology of perturbagen classes (PCLs) To render the CLUE database relatively easy for users to quickly find the mechanism of action (MOA) of a target drug, codifying the class-level annotation required considerable effort. MOAs were adopted to identify groups of compounds with distinct chemical structures, and genetic perturbagens were grouped on the basis of their belonging to the same 1 gene family or being commonly targeted by the same compounds. Ultimately, CLUE named PCLs for their class-level annotations and further connected these cognate class members according to the results of L1000 connectivity analyses to predict the mechanism [2]. 2 A B 3 C D 4 E 5 Figure S1. -

View of HER2: Human Epidermal Growth Factor Receptor 2; TNBC: Triple-Negative Breast Resistance to Systemic Therapy in Patients with Breast Cancer
Wen et al. Cancer Cell Int (2018) 18:128 https://doi.org/10.1186/s12935-018-0625-9 Cancer Cell International PRIMARY RESEARCH Open Access Sulbactam‑enhanced cytotoxicity of doxorubicin in breast cancer cells Shao‑hsuan Wen1†, Shey‑chiang Su2†, Bo‑huang Liou3, Cheng‑hao Lin1 and Kuan‑rong Lee1* Abstract Background: Multidrug resistance (MDR) is a major obstacle in breast cancer treatment. The predominant mecha‑ nism underlying MDR is an increase in the activity of adenosine triphosphate (ATP)-dependent drug efux trans‑ porters. Sulbactam, a β-lactamase inhibitor, is generally combined with β-lactam antibiotics for treating bacterial infections. However, sulbactam alone can be used to treat Acinetobacter baumannii infections because it inhibits the expression of ATP-binding cassette (ABC) transporter proteins. This is the frst study to report the efects of sulbactam on mammalian cells. Methods: We used the breast cancer cell lines as a model system to determine whether sulbactam afects cancer cells. The cell viabilities in the present of doxorubicin with or without sulbactam were measured by MTT assay. Protein identities and the changes in protein expression levels in the cells after sulbactam and doxorubicin treatment were determined using LC–MS/MS. Real-time reverse transcription polymerase chain reaction (real-time RT-PCR) was used to analyze the change in mRNA expression levels of ABC transporters after treatment of doxorubicin with or without sulbactam. The efux of doxorubicin was measures by the doxorubicin efux assay. Results: MTT assay revealed that sulbactam enhanced the cytotoxicity of doxorubicin in breast cancer cells. The results of proteomics showed that ABC transporter proteins and proteins associated with the process of transcription and initiation of translation were reduced. -

Analysis of the Stability of 70 Housekeeping Genes During Ips Reprogramming Yulia Panina1,2*, Arno Germond1 & Tomonobu M
www.nature.com/scientificreports OPEN Analysis of the stability of 70 housekeeping genes during iPS reprogramming Yulia Panina1,2*, Arno Germond1 & Tomonobu M. Watanabe1 Studies on induced pluripotent stem (iPS) cells highly rely on the investigation of their gene expression which requires normalization by housekeeping genes. Whether the housekeeping genes are stable during the iPS reprogramming, a transition of cell state known to be associated with profound changes, has been overlooked. In this study we analyzed the expression patterns of the most comprehensive list to date of housekeeping genes during iPS reprogramming of a mouse neural stem cell line N31. Our results show that housekeeping genes’ expression fuctuates signifcantly during the iPS reprogramming. Clustering analysis shows that ribosomal genes’ expression is rising, while the expression of cell-specifc genes, such as vimentin (Vim) or elastin (Eln), is decreasing. To ensure the robustness of the obtained data, we performed a correlative analysis of the genes. Overall, all 70 genes analyzed changed the expression more than two-fold during the reprogramming. The scale of this analysis, that takes into account 70 previously known and newly suggested genes, allowed us to choose the most stable of all genes. We highlight the fact of fuctuation of housekeeping genes during iPS reprogramming, and propose that, to ensure robustness of qPCR experiments in iPS cells, housekeeping genes should be used together in combination, and with a prior testing in a specifc line used in each study. We suggest that the longest splice variants of Rpl13a, Rplp1 and Rps18 can be used as a starting point for such initial testing as the most stable candidates. -

Hematopoietic Differentiation
Hematopoietic Differentiation A number of lineages of mature cells are derived by a series of steps from a common stem cell precursor. Myeloid cells including neutrophils and monocytes are important for early defense against infection and because of the occurrence of myeloid leukemias. Myeloid differentiation and activation offers a favorable system for experimental investigation. Some Models of Gene Expression in Myeloid Cells 1. Compare resting neutrophils with neutrophils exposed for two hours to either. – A. Non-pathogenic E. coli. – B. Yersinia pestis D27 (plague bacillus). – C. Non-pathogenic Yersinia D28. 2. Induced differentiation of MPRO promyelocytic cells. NeutrophilsNeutrophils Major frontline defense cells against invading pathogens. – Constitute 70% of the total blood leukocytes. – Terminally differentiated professional phagocytic cells with an antibacterial arsenal. – Use both oxygen dependent and oxygen independent killing mechanisms. Play a central role in 2000X mag inflammation. Distribution of IL-8 transcripts on neutrophils (in situ hybridization) A combination of two Cy3 (red)- A labeled oligonucleotides complementary to IL-8 transcripts were used for in situ hybridization with neutrophils incubated in the absence (A) or presence (B) of ten E. coli K12 organisms per neutrophil. BB Methods of Analysis 1. mRNA analysis. – A. 3’ end restriction fragment gel display. – B. Affymetrix 60k or 42k oligonucleotide arrays. 2. Protein analysis. 2D gel electrophoresis using a variety of ph ranges for isoelectric focusing. MALDI-TOF identification of proteins. Representative Segments of Display Gels of cDNA Fragments: (Left) Neutrophils and Monocytes Exposed to E. coli for 2 H; (Right) Neutrophils Exposed to Various Bacteria for 2 H Ec: E. coli K12; Yp (KIM5): Y. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Proteasome Subunit Beta Type 2 (PSMB2) Rabbit Polyclonal Antibody Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA332716 Proteasome subunit beta type 2 (PSMB2) Rabbit Polyclonal Antibody Product data: Product Type: Primary Antibodies Applications: IF, IHC, WB Recommended Dilution: WB 1:500 - 1:2000, IHC 1:50- 1:200, IF 1:50- 1:200 Reactivity: Human, Mouse, Rat Host: Rabbit Isotype: IgG Clonality: Polyclonal Immunogen: Recombinant protein of human PSMB2 Formulation: Store at -20°C (regular) and -80°C (long term). Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide, 50% glycerol, pH7.3. Concentration: lot specific Purification: Affinity purification Conjugation: Unconjugated Storage: Store at -20°C as received. Stability: Stable for 12 months from date of receipt. Predicted Protein Size: 201 Gene Name: proteasome subunit beta 2 Database Link: NP_002785 Entrez Gene 26445 MouseEntrez Gene 29675 RatEntrez Gene 5690 Human P49721 This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 3 Proteasome subunit beta type 2 (PSMB2) Rabbit Polyclonal Antibody – TA332716 Background: The proteasome is a multicatalytic proteinase complex with a highly ordered ring-shaped 20S core structure. The core structure is composed of 4 rings of 28 non-identical subunits; 2 rings are composed of 7 alpha subunits and 2 rings are composed of 7 beta subunits. Proteasomes are distributed throughout eukaryotic cells at a high concentration and cleave peptides in an ATP/ubiquitin-dependent process in a non-lysosomal pathway. -

Isolation and Characterization of Lymphocyte-Like Cells from a Lamprey
Isolation and characterization of lymphocyte-like cells from a lamprey Werner E. Mayer*, Tatiana Uinuk-ool*, Herbert Tichy*, Lanier A. Gartland†, Jan Klein*, and Max D. Cooper†‡ *Max-Planck-Institut fu¨r Biologie, Abteilung Immungenetik, Corrensstrasse 42, D-72076 Tu¨bingen, Germany; and †Howard Hughes Medical Institute, University of Alabama, 378 Wallace Tumor Institute, Birmingham, AL 35294 Contributed by Max D. Cooper, August 30, 2002 Lymphocyte-like cells in the intestine of the sea lamprey, Petro- existence of the adaptive immune system in jawless fishes, myzon marinus, were isolated by flow cytometry under light- the identity of these cells has remained in doubt. The aim of the scatter conditions used for the purification of mouse intestinal present study was to exploit contemporary methods of cell lymphocytes. The purified lamprey cells were morphologically separation to isolate the agnathan lymphocyte-like cells to indistinguishable from mammalian lymphocytes. A cDNA library characterize them morphologically and by the genes they was prepared from the lamprey lymphocyte-like cells, and more express. than 8,000 randomly selected clones were sequenced. Homology searches comparing these ESTs with sequences deposited in the Materials and Methods databases led to the identification of numerous genes homologous Source and Preparation of Cell Suspension. Ammocoete larvae to those predominantly or characteristically expressed in mamma- (8–13 cm long) of the sea lamprey, Petromyzon marinus (from lian lymphocytes, which included genes controlling lymphopoiesis, Lake Huron, MI) were dissected along the ventral side to extract intracellular signaling, proliferation, migration, and involvement the intestine and the associated typhlosole (spiral valve). Cells of lymphocytes in innate immune responses. -

Cellular and Molecular Signatures in the Disease Tissue of Early
Cellular and Molecular Signatures in the Disease Tissue of Early Rheumatoid Arthritis Stratify Clinical Response to csDMARD-Therapy and Predict Radiographic Progression Frances Humby1,* Myles Lewis1,* Nandhini Ramamoorthi2, Jason Hackney3, Michael Barnes1, Michele Bombardieri1, Francesca Setiadi2, Stephen Kelly1, Fabiola Bene1, Maria di Cicco1, Sudeh Riahi1, Vidalba Rocher-Ros1, Nora Ng1, Ilias Lazorou1, Rebecca E. Hands1, Desiree van der Heijde4, Robert Landewé5, Annette van der Helm-van Mil4, Alberto Cauli6, Iain B. McInnes7, Christopher D. Buckley8, Ernest Choy9, Peter Taylor10, Michael J. Townsend2 & Costantino Pitzalis1 1Centre for Experimental Medicine and Rheumatology, William Harvey Research Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, Charterhouse Square, London EC1M 6BQ, UK. Departments of 2Biomarker Discovery OMNI, 3Bioinformatics and Computational Biology, Genentech Research and Early Development, South San Francisco, California 94080 USA 4Department of Rheumatology, Leiden University Medical Center, The Netherlands 5Department of Clinical Immunology & Rheumatology, Amsterdam Rheumatology & Immunology Center, Amsterdam, The Netherlands 6Rheumatology Unit, Department of Medical Sciences, Policlinico of the University of Cagliari, Cagliari, Italy 7Institute of Infection, Immunity and Inflammation, University of Glasgow, Glasgow G12 8TA, UK 8Rheumatology Research Group, Institute of Inflammation and Ageing (IIA), University of Birmingham, Birmingham B15 2WB, UK 9Institute of -

Role of Phytochemicals in Colon Cancer Prevention: a Nutrigenomics Approach
Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Marjan J van Erk Promotor: Prof. Dr. P.J. van Bladeren Hoogleraar in de Toxicokinetiek en Biotransformatie Wageningen Universiteit Co-promotoren: Dr. Ir. J.M.M.J.G. Aarts Universitair Docent, Sectie Toxicologie Wageningen Universiteit Dr. Ir. B. van Ommen Senior Research Fellow Nutritional Systems Biology TNO Voeding, Zeist Promotiecommissie: Prof. Dr. P. Dolara University of Florence, Italy Prof. Dr. J.A.M. Leunissen Wageningen Universiteit Prof. Dr. J.C. Mathers University of Newcastle, United Kingdom Prof. Dr. M. Müller Wageningen Universiteit Dit onderzoek is uitgevoerd binnen de onderzoekschool VLAG Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Marjan Jolanda van Erk Proefschrift ter verkrijging van graad van doctor op gezag van de rector magnificus van Wageningen Universiteit, Prof.Dr.Ir. L. Speelman, in het openbaar te verdedigen op vrijdag 1 oktober 2004 des namiddags te vier uur in de Aula Title Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Author Marjan Jolanda van Erk Thesis Wageningen University, Wageningen, the Netherlands (2004) with abstract, with references, with summary in Dutch ISBN 90-8504-085-X ABSTRACT Role of phytochemicals in colon cancer prevention: a nutrigenomics approach Specific food compounds, especially from fruits and vegetables, may protect against development of colon cancer. In this thesis effects and mechanisms of various phytochemicals in relation to colon cancer prevention were studied through application of large-scale gene expression profiling. Expression measurement of thousands of genes can yield a more complete and in-depth insight into the mode of action of the compounds. -

Reference Gene Validation Via RT–Qpcr for Human Ipsc-Derived Neural Stem Cells and Neural Progenitors
Molecular Neurobiology https://doi.org/10.1007/s12035-019-1538-x Reference Gene Validation via RT–qPCR for Human iPSC-Derived Neural Stem Cells and Neural Progenitors Justyna Augustyniak1 & Jacek Lenart2 & Gabriela Lipka1 & Piotr P. Stepien3 & Leonora Buzanska1 Received: 26 November 2018 /Accepted: 22 February 2019 # The Author(s) 2019 Abstract Correct selection of the reference gene(s) is the most important step in gene expression analysis. The aims of this study were to identify and evaluate the panel of possible reference genes in neural stem cells (NSC), early neural progenitors (eNP) and neural progenitors (NP) obtained from human-induced pluripotent stem cells (hiPSC). The stability of expression of genes commonly used as the reference in cells during neural differentiation is variable and does not meet the criteria for reference genes. In the present work, we evaluated the stability of expression of 16 candidate reference genes using the four most popular algorithms: the ΔCt method, BestKeeper, geNorm and NormFinder. All data were analysed using the online tool RefFinder to obtain a comprehensive ranking. Our results indicate that NormFinder is the best tool for reference gene selection in early stages of hiPSC neural differentiation. None of the 16 tested genes is suitable as reference gene for all three stages of development. We recommend using different genes (panel of genes) to normalise RT–qPCR data for each of the neural differentiation stages. Keywords human induced Pluripotent Stem Cell (hiPSC) . Neural Stem Cells . Neural -
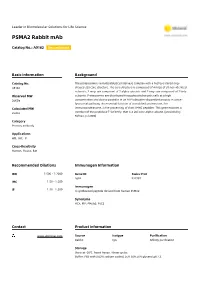
PSMA2 Rabbit Mab
Leader in Biomolecular Solutions for Life Science PSMA2 Rabbit mAb Catalog No.: A9182 Recombinant Basic Information Background Catalog No. The proteasome is a multicatalytic proteinase complex with a highly ordered ring- A9182 shaped 20S core structure. The core structure is composed of 4 rings of 28 non-identical subunits; 2 rings are composed of 7 alpha subunits and 2 rings are composed of 7 beta Observed MW subunits. Proteasomes are distributed throughout eukaryotic cells at a high 26KDa concentration and cleave peptides in an ATP/ubiquitin-dependent process in a non- lysosomal pathway. An essential function of a modified proteasome, the Calculated MW immunoproteasome, is the processing of class I MHC peptides. This gene encodes a 25kDa member of the peptidase T1A family, that is a 20S core alpha subunit. [provided by RefSeq, Jul 2008] Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 5683 P25787 IHC 1:50 - 1:200 Immunogen 1:50 - 1:200 IF A synthesized peptide derived from human PSMA2 Synonyms HC3; MU; PMSA2; PSC2 Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,0.05% BSA,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using PSMA2 Rabbit mAb (A9182) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST.