Minutes of the APPG on Baby Loss
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

'Engaging with Local Stakeholders: Surrey's Post-Covid Recovery Report'
‘Engaging with Local Stakeholders: Surrey’s Post-Covid Recovery Report’ – Launch Event Thursday 12th November 2020 Professor Max Lu – President and Vice Chancellor, University of Surrey Professor Lu began by congratulating those involved with the compiling of the report and speaking of the pride he has of his colleagues who have worked tirelessly around this issue for several months, in addition to voicing how the University of Surrey is proud of its association with both Guildford, and the county of Surrey as a whole. Professor Lu also made references to other areas such as: • Engagement within the county in a range of areas • Recommendations within the report for Surrey’s future • New possibilities for Surrey in knowledge and connectedness • Addressing issues and challenges which need to be overcome Professor Lu concluded on the note of how the University of Surrey hopes to be continually engaged with the county, and how it hopes it can work with local partners to support the county’s agenda, by supporting new research, shaping future knowledge and contributing new opportunities for innovation. Tim Oliver – Leader, Surrey County Council Mr Oliver began by discussing Surrey County Council’s ‘Community Vision 2030’, and its plans to attempt to tackle inequality in the areas of health, climate and community. He stated that the key element which runs through this vision is a ‘strong and sustainable economy,’ which is a foundation upon which the rest of the vision is to be built. Mr Oliver also mentioned a range of other areas, including: -

Committee of the Whole House Proceedings
1 House of Commons Thursday 11 February 2021 COMMITTEE OF THE WHOLE HOUSE PROCEEDINGS MINISTERIAL AND OTHER MATERNITY ALLOWANCES BILL GLOSSARY This document shows the fate of each clause, schedule, amendment and new clause. The following terms are used: Added: New Clause agreed without a vote and added to the Bill. Agreed to: agreed without a vote. Agreed to on division: agreed following a vote. Negatived: rejected without a vote. Negatived on division: rejected following a vote. Not called: debated in a group of amendments, but not put to a decision. Not moved: not debated or put to a decision. Question proposed: debate underway but not concluded. Withdrawn after debate: moved and debated but then withdrawn, so not put to a decision. Not selected: not chosen for debate by the Chair. Kirsten Oswald Negatived 3 Clause 1,page1, line 5, leave out “may” and insert “must” 2 Committee of the whole House Proceedings: 11 February 2021 Ministerial and Other Maternity Allowances Bill, continued Jackie Doyle-Price Sir John Hayes Ben Bradley Tonia Antoniazzi Rosie Duffield Cherilyn Mackrory Andrew Rosindell Fiona Bruce Stephen Metcalfe Bob Blackman Not called 15 Clause 1,page1, line 5, leave out “a person as” Jackie Doyle-Price Sir John Hayes Ben Bradley Tonia Antoniazzi Rosie Duffield Cherilyn Mackrory Andrew Rosindell Fiona Bruce Stephen Metcalfe Bob Blackman Not called 16 Clause 1,page1, line 14, leave out “person” and insert “minister” Sir John Hayes Miriam Cates Lee Anderson Alexander Stafford Ben Bradley Tom Hunt Sir Edward Leigh Karl McCartney -
What Does Ocean Recovery Mean for Your Constituency?
What does Ocean Recovery mean for your Constituency? 16th September 2020 Virtual Meeting: Zoom 10am – 11am ATTENDEES Steve Double MP (Chair) (SD) Oliver Kerr Communications & Hugo Tagholm, CEO Surfers Engagement Manager to Against Sewage (HT) Selaine Saxby MP (OK) Kerry McCarthy MP (Vice Sam Browse Chris Tuckett, Chair of Marine Chair) (KM) Senior Parliamentary Assistant Group at the Wildlife and to Olivia Blake MP (SB) Countryside Link (CT) Cherilyn Mackrory MP (Vice Elinor Cope Parliamentary Alec Taylor, Head of Ocean Chair) (CM) Assistant to Policy WWF UK (AT) Caroline Dinenage MP (EC) Scott Mann MP (Treasurer) Nicole Zandi Senior Ruth Williams, Marine (SM) Parliamentary Assistant to Conservation Manager, Geraint Davies MP (NZ) Cornwall Wildlife Trust (RW) Sir Peter Bottomley MP Huw David for Cherilyn Alice Tebb, Agents for Change (PB) Mackrory MP (HD) Coordinator, Marine Conservation Society (AT) Martyn Day MP Samuel Yung Senior Henry Swithinbank, Surfers (MD) Parliamentary Assistant Against Sewage (HS) to Steve Double MP (SY) Liz Twist MP Chad Male Parliamentary Amy Slack, Surfers Against (LT) Assistant Sewage (AS) to Liz Twist MP (CM) Stephen Crabb MP Natasha Ikners Senior Alice Field, Surfers Against (SC) Parliamentary Assistant to Sewage (AF) Duncan Baker MP(NI) Duncan Baker MP Richard Watt Matt Browne, Wildlife and (DB) Parliamentary Assistant to Countryside Link (MB) Stephen Crabb MP (RW) Megan Randles, WWF UK (MR) Tamara Abidi – WWF UK (TA) MINUTES Welcome and Opening Remarks Steve Double MP, Chair of the APPG welcomed the attendees to the first ever digital Ocean Conservation APPG and set out the role of the group as the voice of the ocean in parliament. -
View Future Day Orals PDF File 0.11 MB
Published: Monday 28 September 2020 Questions for oral answer on a future day (Future Day Orals) Questions for oral answer on a future day as of Monday 28 September 2020. The order of these questions may be varied in the published call lists. [R] Indicates that a relevant interest has been declared. Questions for Answer on Tuesday 29 September Oral Questions to the Secretary of State for Business, Energy and Industrial Strategy Grahame Morris (Easington): Whether he plans to prioritise the development and uptake of human-relevant new approach methodologies in the forthcoming UK research and development roadmap. (906764) Craig Williams (Montgomeryshire): What steps his Department is taking to support businesses during the covid-19 outbreak. (906765) David Mundell (Dumfriesshire, Clydesdale and Tweeddale): What steps his Department is taking to support the Department for International Trade in removing tariffs on Scotch malt whisky. (906766) Neil Parish (Tiverton and Honiton): What steps his Department is taking to help businesses reduce emissions. (906767) Miriam Cates (Penistone and Stocksbridge): What steps his Department is taking to support manufacturing. (906768) Sally-Ann Hart (Hastings and Rye): What steps his Department is taking to support the marine energy sector. (906769) Joy Morrissey (Beaconsfield): What steps his Department is taking to support an environmentally sustainable economic recovery in the automotive sector. (906770) Mrs Emma Lewell-Buck (South Shields): What recent discussions he has had with representatives from those business sectors most affected by the covid-19 outbreak. (906771) 2 Monday 28 September 2020 QUESTIONS FOR ORAL ANSWER ON A FUTURE DAY Neale Hanvey (Kirkcaldy and Cowdenbeath): What recent discussions he has had with (a) Cabinet colleagues and (b) the Scottish Government on the economic effect on businesses of the UK Internal Market Bill. -
Members of the House of Commons December 2019 Diane ABBOTT MP
Members of the House of Commons December 2019 A Labour Conservative Diane ABBOTT MP Adam AFRIYIE MP Hackney North and Stoke Windsor Newington Labour Conservative Debbie ABRAHAMS MP Imran AHMAD-KHAN Oldham East and MP Saddleworth Wakefield Conservative Conservative Nigel ADAMS MP Nickie AIKEN MP Selby and Ainsty Cities of London and Westminster Conservative Conservative Bim AFOLAMI MP Peter ALDOUS MP Hitchin and Harpenden Waveney A Labour Labour Rushanara ALI MP Mike AMESBURY MP Bethnal Green and Bow Weaver Vale Labour Conservative Tahir ALI MP Sir David AMESS MP Birmingham, Hall Green Southend West Conservative Labour Lucy ALLAN MP Fleur ANDERSON MP Telford Putney Labour Conservative Dr Rosena ALLIN-KHAN Lee ANDERSON MP MP Ashfield Tooting Members of the House of Commons December 2019 A Conservative Conservative Stuart ANDERSON MP Edward ARGAR MP Wolverhampton South Charnwood West Conservative Labour Stuart ANDREW MP Jonathan ASHWORTH Pudsey MP Leicester South Conservative Conservative Caroline ANSELL MP Sarah ATHERTON MP Eastbourne Wrexham Labour Conservative Tonia ANTONIAZZI MP Victoria ATKINS MP Gower Louth and Horncastle B Conservative Conservative Gareth BACON MP Siobhan BAILLIE MP Orpington Stroud Conservative Conservative Richard BACON MP Duncan BAKER MP South Norfolk North Norfolk Conservative Conservative Kemi BADENOCH MP Steve BAKER MP Saffron Walden Wycombe Conservative Conservative Shaun BAILEY MP Harriett BALDWIN MP West Bromwich West West Worcestershire Members of the House of Commons December 2019 B Conservative Conservative -
View Call Lists: Westminster Hall PDF File 0.05 MB
Issued on: 27 April at 3.32pm Call lists for Westminster Hall Wednesday 28 April 2021 A list of Members, both virtually and physically present, selected to participate in 60- and 90-minute Westminster Hall debates. 30-minute debates do not have a call list. All Members wishing to speak in the debate must be present from the beginning of the debate. For 60-minute and 90-minute debates, only Members on the call list will be called to speak, and they will be called in the order they appear on the call list, subject to discretion of the Chair. Members who are not on the call list are not permitted to attend debates. For 30-minute debates, there will not be a call list. Members may attend to intervene or make a short speech. Members wishing to make a speech should follow existing conventions about contacting the Member in charge of the debate, the Speaker’s Office [email protected]( ) and the Minister. If sittings are suspended for divisions in the House, additional time is added. Call lists are compiled and published incrementally as information becomes available. For the most up-to-date information see the parliament website: https://commonsbusiness.parliament.uk/ CONTENTS 1. Proposed closure of GKN Automotive plant in Birmingham 1 2. Extending redundancy protection for women and new parents 2 3. British meat and dairy products 2 4. Protecting consumers from online scams 3 5. District heat networks 3 PROPOSED CLOSURE OF GKN AUTOMOTIVE PLANT IN BIRMINGHAM 9.25am to 10.55am Order Member Party Virtual/ Physical 1 Jack Dromey (Birmingham, -
Putting Nature and Net Zero at the Heart of the Economic Recovery
House of Commons Environmental Audit Committee Growing back better: putting nature and net zero at the heart of the economic recovery Third Report of Session 2019–21 Report and Appendix, together with formal minutes relating to the report Ordered by the House of Commons to be printed 10 February 2021 HC 347 Published on 17 February 2021 by authority of the House of Commons Environmental Audit Committee The Environmental Audit Committee is appointed by the House of Commons to consider to what extent the policies and programmes of government departments and non-departmental public bodies contribute to environmental protection and sustainable development; to audit their performance against such targets as may be set for them by Her Majesty’s Ministers; and to report thereon to the House. Current membership Rt Hon Philip Dunne MP (Conservative, Ludlow) (Chair) Duncan Baker MP (Conservative, North Norfolk) Sir Christopher Chope MP (Conservative, Christchurch) Feryal Clark MP (Labour, Enfield North) Barry Gardiner MP (Labour, Brent North) Rt Hon Robert Goodwill MP (Conservative, Scarborough and Whitby) Ian Levy MP (Conservative, Blyth Valley) Marco Longhi MP (Conservative, Dudley North) Caroline Lucas MP (Green Party, Brighton, Pavilion) Cherilyn Mackrory MP (Conservative, Truro and Falmouth) Jerome Mayhew MP (Conservative, Broadland) John McNally MP (Scottish National Party, Falkirk) Dr Matthew Offord MP (Conservative, Hendon) Alex Sobel MP (Labour (Co-op), Leeds North West) Claudia Webbe MP (Independent, Leicester East) Nadia Whittome MP (Labour, Nottingham East) The following Member is a former member of the Committee: Mr Shailesh Vara MP (Conservative, North West Cambridgeshire) Powers The constitution and powers of the Committee are set out in House of Commons Standing Orders, principally in SO No 152A. -

Daily Report Wednesday, 20 May 2020 CONTENTS
Daily Report Wednesday, 20 May 2020 This report shows written answers and statements provided on 20 May 2020 and the information is correct at the time of publication (07:20 P.M., 20 May 2020). For the latest information on written questions and answers, ministerial corrections, and written statements, please visit: http://www.parliament.uk/writtenanswers/ CONTENTS ANSWERS 6 Joint Strike Fighter Aircraft 14 BUSINESS, ENERGY AND Maritime Patrol Aircraft: INDUSTRIAL STRATEGY 6 Procurement 14 Coronavirus Business Military Aid: Coronavirus 14 Interruption Loan Scheme: Royal Fleet Auxiliary: Tankers 15 Dental Services 6 DIGITAL, CULTURE, MEDIA AND Department for Business, SPORT 15 Energy and Industrial Strategy: Correspondence 6 Arts: Coronavirus 15 Hospitality Industry and Retail Department for Digital, Trade 6 Culture, Media and Sport: Public Service Broadcasting 16 Manufacturing Industries: Coronavirus 7 Leisure: Coronavirus 16 Small Businesses: Non- Musicians: Visas 16 domestic Rates 7 Television: Licensing 17 WH Smith: Post Offices 8 EDUCATION 17 CHURCH COMMISSIONERS 8 Children: Coronavirus 17 Church Services: Attendance 8 Free School Meals: Churches: Coronavirus 9 Coronavirus 19 DEFENCE 11 Nurseries: Coronavirus 20 Armed Forces: Recruitment 11 Pre-school Education: Coronavirus 20 Army 12 Schools: Coronavirus 21 Army Reserve 12 Students: Coronavirus 24 British Overseas Territories: Coronavirus 13 ENVIRONMENT, FOOD AND RURAL AFFAIRS 25 Global Navigation Satellite Systems 13 Agricultural Products: Prices 25 2 Wednesday, 20 May 2020 Daily -

Frohe Weinachten Feliz Navidad Joyeux Noël Buon Natale Καλά
Volume 37 Number 3 Success at CoP26 starts at home: Leading by example on Net Zero - Steve Holliday FREng FEI Transport and Heating towards Net Zero – Hydrogen update December 2020 Renewables: leading transitions to a more sustainable energy system – Dr Fatih Birol, IEA Launch of PGES 40th Anniversary Inquiry ENERGY FOCUS Frohe Weinachten καλά Χριστούγεννα Feliz Navidad Bożego Narodzenia Joyeux Noël Vrolijk kerstfeest Buon Natale Wesołych świąt Veselé Vianoce Veselé Vánoce Crăciun fericit Glædelig jul Vesel božič Feliz Natal God Jul This is not an official publication of the House of Commons or the House of Lords. It has not been approved by either House or its committees. All-Party Parliamentary Groups are informal groups of Members of both Houses with a common interest in particular issues. The views expressed in Energy Focus are those of the individual organisations and contributors Back to Contents and doBack not necessarily to Contents represent the views held by the All-Party Parlia- mentary Group for Energy Studies. The journal of The All-Party Parliamentary Group for Energy Studies Established in 1980, the Parliamentary Group for Energy Studies remains the only All-Party Parliamentary Group representing the entire energy industry. PGES aims to advise the Government of the day of the energy issues of the day. The Group’s membership is comprised of over 100 parliamentarians, 100 associate bodies from the private, public and charity sectors and a range of individual members. Published three times a year, Energy Focus records the Group’s activities, tracks key energy and environmental developments through parliament, presents articles from leading industry contributors and provides insight into the views and interests of both parliamentarians and officials. -

The Government's Independent Review of the Human Rights
House of Commons House of Lords Joint Committee on Human Rights The Government’s Independent Review of the Human Rights Act Third Report of Session 2021–22 Report, together with formal minutes relating to the report Ordered by the House of Commons to be printed 23 June 2021 Ordered by the House of Lords to be printed 23 June 2021 HC 89 HL Paper 31 Published on 8 July 2021 by authority of the House of Commons and House of Lords Joint Committee on Human Rights The Joint Committee on Human Rights is appointed by the House of Lords and the House of Commons to consider matters relating to human rights in the United Kingdom (but excluding consideration of individual cases); proposals for remedial orders, draft remedial orders and remedial orders. The Joint Committee has a maximum of six Members appointed by each House, of whom the quorum for any formal proceedings is two from each House. Current membership House of Commons Harriet Harman QC MP (Labour, Camberwell and Peckham) (Chair) Karen Buck MP (Labour, Westminster North) Joanna Cherry QC MP (Scottish National Party, Edinburgh South West) Angela Richardson MP (Conservative, Guildford) Dean Russell MP (Conservative, Watford) David Simmonds MP (Conservative, Ruislip, Northwood and Pinner) House of Lords Lord Brabazon of Tara (Conservative) Lord Dubs (Labour) Lord Henley (Conservative) Baroness Ludford (Liberal Democrat) Baroness Massey of Darwen (Labour) Lord Singh of Wimbledon (Crossbench) Powers The Committee has the power to require the submission of written evidence and documents, to examine witnesses, to meet at any time (except when Parliament is prorogued or dissolved), to adjourn from place to place, to appoint specialist advisers, and to make Reports to both Houses. -
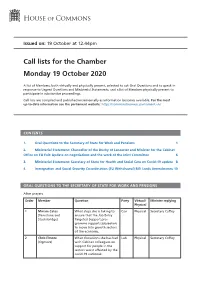
View Call Lists
Issued on: 19 October at 12.44pm Call lists for the Chamber Monday 19 October 2020 A list of Members, both virtually and physically present, selected to ask Oral Questions and to speak in response to Urgent Questions and Ministerial Statements; and a list of Members physically present to participate in substantive proceedings. Call lists are compiled and published incrementally as information becomes available. For the most up-to-date information see the parliament website: https://commonsbusiness.parliament.uk/ CONTENTS 1. Oral Questions to the Secretary of State for Work and Pensions 1 2. Ministerial Statement: Chancellor of the Duchy of Lancaster and Minister for the Cabinet Office on EU Exit: Update on negotiations and the work of the Joint Committee 6 3. Ministerial Statement: Secretary of State for Health and Social Care on Covid-19 update 8 4. Immigration and Social Security Co-ordination (EU Withdrawal) Bill: Lords Amendments 10 ORAL QUESTIONS TO THE SECRETARY OF STATE FOR WORK AND PENSIONS After prayers Order Member Question Party Virtual/ Minister replying Physical 1 Miriam Cates What steps she is taking to Con Physical Secretary Coffey (Penistone and ensure that the Job Entry Stocksbridge) Targeted Support pro- gramme supports jobseekers to move into growth sectors of the economy. 2 Chris Elmore What discussions she has had Lab Physical Secretary Coffey (Ogmore) with Cabinet colleagues on support for people in the sectors worst affected by the covid-19 outbreak. 2 Call lists for the Chamber Monday 19 October 2020 Order Member Question Party Virtual/ Minister replying Physical 3 Neil Gray (Airdrie and Supplementary SNP Virtual Secretary Coffey Shotts) 4 Alison McGovern What recent assessment she Lab Physical Minister Quince (Wirral South) has made of the effect of the covid-19 outbreak on levels of child poverty. -

Local Electricity Bill
Local Electricity Bill A B I L L TO Enable electricity generators to become local electricity suppliers; and for connected purposes. 1 Purpose The purpose of this Act is to encourage and enable the local supply of electricity. 2 Local electricity suppliers (1) An electricity generator may be a local electricity supplier. (2) In this section “electricity generator” has the same meaning as in section 6 of the Electricity Act 1989. (3) A local supplier must – (a) hold a local electricity supply licence, and (b) adhere to the conditions of that local electricity supply licence. 3 Amendment of the Electricity Act 1989 (1) The Electricity Act 1989 is amended as follows. (2) In section 6 (licences authorising supply, etc.), after subsection (1)(d), insert – “(da) a licence authorising a person to supply electricity to premises within a designated local area (“a local electricity supply licence”); (3) After section 6 insert – “6ZA Local electricity supply licences (1) Subject to it exercising its other functions under this Act the Gas and Electricity Markets Authority (“the Authority”) may grant a local electricity supply licence to a person who meets local electricity supply licence conditions. (2) The Authority must set local electricity supply licence conditions. (3) The Authority must specify the designated local area for each local electricity supply licence. (4) Before making any specification under subsection (3) the Authority must consult – (a) any relevant local authority; (b) any existing local electricity suppliers; (c) any persons who have, to the knowledge of the Authority, expressed an interest in becoming local electricity suppliers; (d) any other person who, in its opinion, has an interest in that matter.