Abhiyaanmonitoringreport.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

INDIA YEAR BOOK-2017 Good Luck!
INDIA YEAR BOOK - 2017 INDIA YEAR BOOK-2017 Dear Students, With the focus on the provision of best study material to our students, Rau’s IAS Study Circle is innovatively presenting the voluminous INDIA YEAR BOOK-2017 in a very concise and lucid manner. Through this, efforts have been taken to circulate the best synopsis extracted from the Year Book-2017 for the benefit of the students. The abstract has been designed to present contents of the year book in most user-friendly manner. All the major and important points are given in bold and highlighted. The content is also supported by figures and pictures as per the requirement. The content has been chosen and compiled judiciously so that maximum coverage of all the relevant and significant material is presented within minimum readable pages. The issue titled ‘INDIA YEAR BOOK-2017 will be covering the following topics: 1. Land and the People 16. Health and Family Welfare 2. National Symbols 17. Housing 3. The Polity 18. India and the World 4. Agriculture 19. Industry 5. Culture and Tourism 20. Law and Justice 6. Basic Economic Data 21. Labour, Skill Development and Employment 7. Commerce 22. Mass Communication 8. Communications and Information Technology 23. Planning 9. Defence 24. Rural and Urban Development 10. Education 25. Scietific and Technological Developments 11. Energy 26. Transport 12. Environment 27. Water Resources 13. Finance 28. Welfare 14. Corporate Affairs 29. Youth Affairs and Sports 15. Food and Civil Supplies By providing this, the Study Circle hopes that all the students will be able to make the best use of it as a ready reference material and allay their fears of perusing and cramming the entire year book. -
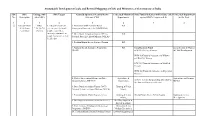
Sustainable Development Goals and Revised Mapping of Csss and Ministries of Government of India
Sustainable Development Goals and Revised Mapping of CSSs and Ministries of Government of India SDG SDG Linkage with SDG Targets Centrally Sponsored /Central Sector Concerned Ministries/ State Funded Schemes (with Scheme code) Concerned Department No. Description other SDGs Schemes (CSS) Departments against SDG's Targets (col. 4) in the State 1 2 3 4 5 6 7 8 ① End poverty in SDGs 1.1 By 2030, eradicate 1. Mahatma Gandhi National Rural RD all its forms 2,3,4,5,6,7,8, extreme poverty for all Employment Guarantee Act (MGNREGA) everywhere 10,11,13 people everywhere, currently measured as 2. Deen Dayal Antyodaya Yojana (DAY) - RD people living on less than National Rural Livelihood Mission (NRLM) $1.25 a day 3. Pradhan Mantri Awaas Yojana - Gramin RD 4. National Social Assistance Programme RD Social Security Fund Social Secuity & Women (NSAP) SSW-03) Old Age Pension & Child Development. WCD-03)Financial Assistance to Widows and Destitute women SSW-04) Financial Assistance to Disabled Persons WCD-02) Financial Assistance to Dependent Children 5. Market Intervention Scheme and Price Agriculture & Agriculture and Farmers Support Scheme (MIS-PSS) Cooperation, AGR-31 Scheme for providing debt relief to Welfare the distressed farmers in the state 6. Deen Dayal Antyodaya Yojana (DAY)- Housing & Urban National Urban Livelihood Mission (NULM) Affairs, 7. Pradhan Mantri Awaas Yojana -Urban Housing & Urban HG-04 Punjab Shehri Awaas Yojana Housing & Urban Affairs, Development 8. Development of Skills (Umbrella Scheme) Skill Development & Entrepreneurship, 9. Prime Minister Employment Generation Micro, Small and Programme (PMEGP) Medium Enterprises, 10. Pradhan Mantri Rojgar Protsahan Yojana Labour & Employment Sustainable Development Goals and Revised Mapping of CSSs and Ministries of Government of India SDG SDG Linkage with SDG Targets Centrally Sponsored /Central Sector Concerned Ministries/ State Funded Schemes (with Scheme code) Concerned Department No. -

Economic Survey and Challenges in Indian Economy
ECONOMIC SURVEY AND CHALLENGES IN INDIAN ECONOMY Ramesh Chand Member, NITI Aayog The year 2015-16 has been a very difficult year for the Indian economy. The global environment remained unfavourable for exports and slowdown in the major economies, put downward pressure on the growth rate of Indian economy as well. India faced four consecutive unfavourable weather seasons which hit agricultural and rural economy hard. The country received below normal monsoon rain and experienced drought in many parts during 2014 and again in 2015. The crop output during rabi season last year (2014-15) suffered due to untimely and excessive rainfall, hailstorms and freak weather. Again in year 2015-16, many parts of the country remained highly deficit in winter rains. The temperature has been ruling much higher than normal. As a result, crop output in rabi season of year 2015-16 is expected to be lower than the normal. The rainfall deficiency has not only affected agricultural output, it has also affected other economic activities due to low availability of water. The adverse climatic factors not only affected output of agriculture sector but also caused adverse effect on non-agriculture sector due to depressed demand in rural India. If agriculture output was normal, it would have pushed the growth rate in total GDP up by 0.30 percentage points. Despite these odds the growth rate in total GDP is estimated to accelerate to 7.6 per cent. It is remarkable that despite negative growth of agriculture output during 2014-15 and below normal output in year 2015-16 food inflation has remained below 6 per cent. -

Current Affairs-July 2019 the Capital City of Rajasthan-Jaipur Has Been
Current Affairs-July 2019 ❏ The capital city of Rajasthan-Jaipur has been granted the status of World Heritage Site by UNESCO, becoming the 38th site from India to be so tagged. The city was nominated for its value of being an exemplary development in town planning and architecture(Govind Dev temple, City Palace, Jantar Mantar and Hawa Mahal). ➢ Jaipur: It is also known as the Walled City, the Pink City. It was founded in 1727 by Sawai Jai Singh II. ➢ Ahmedabad became the first Indian city to get into the list. ❏ Bimal Jalan panel that was set up to review the economic capital framework of the Reserve Bank of India (RBI) has decided to recommend transfer of surplus reserves to the government . According to Section 47 of the RBI Act, profits of the RBI are to be transferred to the government, after making various contingency provisions. In the past, the issue of the ideal size of RBI's reserves was examined by three committees,V Subrahmanyam (1997) 2. Usha Thorat (2004), Y H Malegam (2013). ❏ The three-year road map launched by Reserve Bank of India board to improve regulation and supervision is named – Utkarsh 2022. ❏ Andhra Bank launched its Artificial Intelligence interactive assistant — ABHi. ❏ According to the RBI data, Maharashtra topped in ATM frauds in 2018-19 with 233 cases. Delhi grabbed the second spot followed by Tamil Nadu. ❏ ICICI Bank has launched the digital platform called ‘InstaBIZ’ for MSME & self-employed customers. ❏ RBI slapped a penalty of Rs 7 crore on SBI.The penalty has been imposed on SBI for noncompliance of income recognition & asset classification norms, code of conduct for opening & operating current accounts and reporting of data on (CRILC). -
Estimates of Multidimensional Poverty for India Using NSSO-71 and -75
WIDER Working Paper 2021/1 Estimates of multidimensional poverty for India using NSSO-71 and -75 Venugopal Mothkoor* and Nina Badgaiyan* January 2021 Abstract: We measure multidimensional poverty in India using National Sample Survey Organization data from 2014–15 to 2017–18. We use income, health, education, and standard of living to measure the MPI. The MPI headcount declined from 26.9 to 13.75 per cent over the study period. The all-India estimates indicate that 144 million people were lifted from poverty during this period. We include different health dimensions, factoring in insurance, institutional coverage, antenatal care, and chronic conditions. Income is the dominant instrument with the highest contribution to the MPI, followed by insurance. Cooking, sanitation, and education also have significant weights. The decline in deprivation is steeper in rural areas than urban areas. Our state-level estimates reveal that 20 states report less than 10 per cent headcount poverty, up from six states. COVID-19 may lead to reversals of these gains, with poverty rising to pre-2014–15 levels, rising more steeply in rural areas. Key words: MPI, income, poverty, India, deprivation, rural, urban, COVID-19 JEL classification: I14, I30, I32, I38 Disclaimer: The views expressed in this paper are those of the authors, and do not necessarily reflect the views of Niti Aayog. * Niti Aayog, New Delhi, India; corresponding author: [email protected] This study has been prepared within the UNU-WIDER project Addressing group-based inequalities. Copyright © UNU-WIDER 2021 UNU-WIDER employs a fair use policy for reasonable reproduction of UNU-WIDER copyrighted content—such as the reproduction of a table or a figure, and/or text not exceeding 400 words—with due acknowledgement of the original source, without requiring explicit permission from the copyright holder. -

Economic Bulletin CONSULATE GENERAL of INDIA, TORONTO
January - February 2021, Issue 5 Economic Bulletin CONSULATE GENERAL OF INDIA, TORONTO ECONOMIC LANDSCAPE IN INDIA Start-ups are playing a crucial role in making India self-reliant: PM Modi In his address at ‘Prarambh: Startup India International Summit’, Prime Minister Modi appreciated the startup spirit of finding opportunity in adversity. He pointed out that 45 per cent startups in India are in tier 2 and tier 3 cities, working as the brand ambassadors of the local products. He added that every state was supporting and incubating startups as per local possibilities and 80 percent of districts of the country were now part of the Startup India mission. He said that Startups played a major role in ensuring availability of sanitizers, PPE kits and related supply chain and also in meeting local needs like grocery, medicine delivery at doorstep, transportation of frontline workers and online study material. Click here to read the article. DISCLAIMER: The data used in this bulletin has been obtained from various open/published sources. The Consulate General of India, Toronto does not accept any responsibility for accuracy/authenticity of this information. 1 India is on the path to reclaim its title as the world’s fastest-growing major economy: IMF The International Monetary fund (IMF) has projected an impressive 11.5% growth rate for India in 2021, which will make the country the only major world economy to register a double-digit growth. The high growth has been projected on account of stronger than expected recovery, strong GST collections & good agricultural growth. With the latest projections, India would regain the tag of the fastest developing economies of the world followed by anticipated growth of China at 8.1 per cent, Spain at 5.9 per cent and France at 5.5 per cent. -

NEWS U CAN USE August 28, 2020
NEWS U CAN USE August 28, 2020 Mutual Fund Investments are subject to market risks, read all scheme related documents carefully. The Week that was… 24th Aug to 28th Aug 2 Mutual Fund Investments are subject to market risks, read all scheme related documents carefully. Indian Economy • According to corporate affairs ministry numbers, corporate incorporations in Jul 2020 reached a seven-year high of 16,487, or 530 per day, which is 50% increase from a year earlier. • According to media reports, the government proposes to bring within the scope of the proposed social security code at least half a dozen social security schemes, including old age pension and insurance schemes. The move aims to universalize by putting all current programs under one umbrella without any extra costs to the exchequer and is projected to cover more than 20% of the population's edge. • According to a major credit rating agency, Indian economy could have contracted by 25% in the first quarter of the FY21 making it one of the most negative estimates for Asia's third largest economy. The agency also cautioned that recovery could take some time as the virus spreads and numbers of infections increase, causing more localized closures. • According to a report by Niti Aayog, Gujarat has topped the Niti Aayog's Export Preparedness Index 2020 followed by Maharashtra and Tamil Nadu. A favorable environment helps a country to make a major contribution to global supply chains and benefit internationally from interconnected production networks. 3 Mutual Fund Investments are subject to market risks, read all scheme related documents carefully. -

Urban Development in India: a Special Focus Public Finance Newsletter
Urban development in India: A special focus Public Finance Newsletter Issue XI March 2016 In this issue 2 Feature article 10 Pick of the quarter 20 Round the corner 22 Potpourri 24 PwC updates Knowledge is the only instrument of production that is not subject to diminishing returns. J M Clark Dear readers, ‘Round the corner’ provides news updates in the area of government finances and policies across the The above quotation from the globe and key paper releases in the public finance American economist still domain during the recent months, along with holds true. Knowledge reference links. The ‘Our work’ section presents a increases by sharing and our mid-term review of the Support Program for Urban initiative to share knowledge, Reforms (SPUR), Bihar, which was conducted by views and experiences in the our team for the Department for International public finance domain Development (DFID). SPUR is a six-year through this newsletter has given us returns in the programme being implemented by the Government form of readers and contributors from across the of Bihar in partnership with DFID in 29 urban local globe. In continuation with our efforts in this bodies of Bihar. direction, I welcome you to the eleventh issue of the Public Finance Newsletter. I would like to thank you for your overwhelming support and response. Your suggestions urge us to The feature article in this issue aims to delve continuously improve this newsletter to ensure deeper into India’s urban development agenda. effective information sharing. Last year, we witnessed the launch of new missions such as Atal Mission for Rejuvenation and Urban We would like to invite you to contribute and share Transformation (AMRUT), which replaced the your experiences in the public finance space with Jawaharlal Nehru National Urban Renewal Mission us. -

Task Force on Elimination of Poverty in India
Task Force on Elimination of Poverty in India Regional Consultation Meeting 1 Based on the work of the Task Force, prepared a paper on ‘Eliminating Poverty : Creating Jobs and Strengthening Social Programs’ 2 Task Force Meetings, Consultation and Approach • NITI Aayog’s Taskforce constituted in March 2015 under the Chairmanship of Vice Chairman, NITI Aayog • Members include one NITI Member, CEA, experts and Secretaries of the relevant ministries. • Parallel Task Forces were to be constituted in all States/Uts. • Three meetings of the Task Force were held. • Consultations were held with economists, journalists and NGOs. • Selected a small number of most important topics instead of being comprehensive. 3 Broad Issues 1. Measuring Poverty in India: A Brief History 2. Assessing the Need for an Official Poverty Line 3. Combating Poverty: Employment-intensive Sustained Rapid Growth 4. Combating Poverty: Making Social Programs More Effective 5. Combating Poverty: New Approaches 4 1. MEASURING POVERTY IN INDIA: A BRIEF HISTORY 5 Poverty Line, Poverty Line Basket and Poverty Ratio • The conventional approach to measuring poverty is to specify a minimum expenditure (or income) required to purchase a basket of goods and services necessary to satisfy basic human needs. • This minimum expenditure is called the poverty line. • The basket of goods and services necessary to satisfy basic human needs is the poverty line basket or PLB. • The proportion of population below the poverty line is called the poverty ratio or headcount ratio (HCR). 6 Measuring Poverty in India: A Brief History (1 of 2) • Most countries and international institutions (WB, UN) follow similar approach for counting the poor. -
Artificial Intelligence and Healthcare in India
CSD Working Paper Series: Towards a New Indian Model of Information and Communications Technology-Led Growth and Development Artificial Intelligence and Healthcare in India ICT India Working Paper #43 Nirupam Bajpai and Manisha Wadhwa January 2020 CSD Working Paper Series – Artificial Intelligence and Healthcare in India Abstract Artificial Intelligence (AI), also referred to as the new electricity, is the emerging focus area in India. AI refers to the ability of machines to perform cognitive tasks like thinking, perceiving, learning, problem solving and decision making. Most of the AI systems rely on historical large datasets for predicting future trends and outcomes at a pace which humans would not be able to match. The development of AI in India is in the initial stages and there is no regulatory body focused solely on AI. However, recently, Government of India has taken various initiatives related to AI such as establishment of Artificial Intelligence Task Force, formulation of NITI Aayog's National Strategy for Artificial Intelligence #AIFORALL, setting up of four Committees for AI under Ministry of Electronics and Information technology etc. Some of India’s state governments have also taken few initiatives, such as establishment of Centre of Excellence for Data Science and Artificial Intelligence (CoE-DS&AI) by Karnataka, Safe and Ethical Artificial Intelligence Policy 2020 and Face Recognition Attendance System by Tamil Nadu, AI-Powered System for monitoring driving behaviour by West Bengal, AI System to fight agricultural risks by Maharashtra etc. As with any other technology, AI brings with it a span of opportunities and challenges. In healthcare, AI could be beneficial in mining medical records; designing treatment plans; forecasting health events; assisting repetitive jobs; doing online consultations; assisting in clinical decision making; medication management; drug creation; making healthier choices and decisions; and solving public health problems etc. -

India's Electric Mobility Transformation
INDIA’S ELECTRIC MOBILITY TRANSFORMATION PROGRESS TO DATE AND FUTURE OPPORTUNITIES NITI AAYOG & ROCKY MOUNTAIN INSTITUTE INDIA’S ELECTRIC MOBILITY TRANSFORMATION PROGRESS TO DATE AND FUTURE OPPORTUNITIES NITI AAYOG & ROCKY MOUNTAIN INSTITUTE APRIL 2019 AUTHORS AND ACKNOWLEDGEMENTS AUTHORS: NITI AAYOG ACKNOWLEDGEMENTS Aakaash Singh The authors would like to thank Dr. Rajiv Abhishek Saxena Kumar, Vice Chairman, NITI Aayog and Anil Srivastava Mr. Amitabh Kant, CEO, NITI Aayog for Apoorva Bhandari their support that made this report possible. Harkiran K. Sanjeevi Joseph Teja SUGGESTED CITATION NITI Aayog and Rocky Mountain AUTHORS: RMI Institute (RMI). India’s Electric Mobility Akshima Ghate Transformation: Progress to date and future Aman Chitkara opportunities. 2019. Clay Stranger Emily Goldfield “The views and opinions expressed in this Robert McIntosh document are those of the authors and do not Samhita Shiledar necessarily reflect the positions of their instit- utions or governments. While every effort has (Listed alphabetically) been made to verify the data and information contained in this report, any mistakes or omis- CONTACTS sions are attributed solely to the authors and NITI Aayog: [email protected] not to the organizations they represent.” www.niti.gov.in IMAGE CREDITS RMI: [email protected] Shutterstock www.rmi.org INDIA’S ELECTRIC MOBILITY TRANSFORMATION TABLE OF CONTENTS ————————————————————————— EXECUTIVE SUMMARY ............................... .................................................................... 06 CHAPTER -

1. AK Mohanty Appointed As Director in Bhabha Atomic
Current Affairs - March 2019 Month All Type All 163 Current Affairs were found in Period - March 1 - 10, 2019 for Type - All Appointments 1. A.K. Mohanty appointed as Director in Bhabha Atomic Research Centre (BARC). 2. Ajit Singh (Former Chief Justice of Gauhati HC) has been appointed as first Lokayukta of Odisha. 3. Bhagwan Lal Sahni appointed as Chairman of National Commission for Backward Classes. 4. Former Indian cricketer Anil Kumble has been reappointed as Chairman of the ICC Cricket Committee for 3rd consecutive term. 5. Government Appointed P V Ramesh as director-general of National Archives of India. 6. Government appointed Subhash Chandra Garg as Finance Secretary, replacing Ajay Narayan Jha who retired recently. Conventionally, senior-most among 5 secretaries in Finance Ministry is designated as Finance Secretary. 7. Indian Scientist Soumya Swaminathan has been named Chief Scientist at WHO (World Health Organization). 8. Indian-American Padma Lakshmi appointed by United Nations Development Programme (UNDP) as its Goodwill Ambassador, supporting agency’s fight against inequality and discrimination around the world. 9. Jagdish Mukhi has been appointed as Governor of Mizoram, after Kummanam Rajasekharan Resigned from post. 10. Kaja Kallas, leader of the Reform Party has been appointed as first female Prime Minister of Estonia (Northern Europe). 11. Macky Sall re-elected as President of Senegal (West Africa). 12. Mohammad Shtayyeh has been named as new Palestinian Prime Minister, by President of Palestinian Authority Mahmoud Abbas. 13. P K Bezbaruah has been reappointed as Chairman of Tea Board for 2nd tenure. He is first non-IAS chairman of the Tea Board.