The Superoxide Anion Donor, Potassium Superoxide, Induces Pain and Inflammation in Mice Through Production of Reactive Oxygen Species and Cyclooxygenase-2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The History of Dräger Johann Heinrich Dräger (1847–1917) Dr
D The History of Dräger Johann Heinrich Dräger (1847–1917) Dr. Bernhard Dräger (1870–1928) Dr. Heinrich Dräger (1898–1986) Contents 04 The Early Years: From Inventor’s Workshop to Medical and Safety Technology Specialist 10 Turbulent Times: Between Innovation Challenges and Political Constraints 20 New Beginnings: Transformation to a Modern Technology Group 30 Globalization: Realignment as a Global Technology Leader Dr. Christian Dräger (*1934) Theo Dräger (*1938) Stefan Dräger (*1963) Technology for Life for over 120 years Dräger is technology for life. Every day we take on the responsibility and put all our passion, know-how and experience into making life better: With outstanding, pioneering technology which is 100 percent driven by life. We do it for all the people around the world who entrust their lives to our technology, for the environment and for our common future. The key to the continued success of the Company, based in Lübeck, Germany, is its clear focus on the promising growth industries of medical and safety technology, its early expansi- on to international markets, and above all, the trust it has built and maintains with custo- mers, employees, shareholders, and the general public. The Company has always been managed by entrepreneurial members of the Dräger family, who have responsibly met new challenges while never losing sight of the vision: Johann Heinrich Dräger, Dr. Bernhard Dräger, Dr. Heinrich Dräger, Dr. Christian Dräger, Theo Dräger, and now Stefan Dräger. Healthy growth has consistently remained the main objective of the family business and shapes decisions within the Company even now. Founded in 1889 by Johann Heinrich Dräger, the family business has been headed in the fifth generation by CEO Stefan Dräger since 2005. -

Potassium Superoxide (KO2) 1
Potassium Superoxide (KO2) 1. OTHER NAMES a. Potassium Dioxide b. Potassium hyperoxide 2. CAS NO. 12030-88-5 3. FORMULA WEIGHT 71.10 gm/mole 4. SPECIFICATION Sr SPECIFICATION POWDER SHEET GRANULES I GRANULES II No. 1. Appearance Pale Yellow Pale Yellow Pale Yellow Pale Yellow 2. KO2 content (%) min 96 90 82.5 96 3. Copper content (%) -- 0.25 0.25 0.25 4. CO2 Evolution (ml/gm) 220 Min 170 Min 190 -200 220-230 5. CO2 Evolution (ml/gm) max 6 12 12 6 6. Sizes (mm) NA L:313-318/B:216-221 / T:5.5-6 3.5-5.6 3.5-5.6 7. Weight (gm) 380-400 --- --- --- 8. Dust content (passing through 125 μ sieve ---- NA 0.5 0.5 (%) max SUPARNA CHEMICALS LTD 54 A Mittal Tower, Nariman Point, Mumbai India. Phone No: 022-22027446/7/8/9 Email Id: [email protected] [email protected] Potassium Superoxide (KO2) 5. REACTIVITY Potassium superoxide is a strong oxidizing agent and reacts explosively with organic materials. 6. SOLUBILITY Potassium superoxide is soluble in ethers and hydrocarbons. 7. STABILITY Potassium superoxide reacts readily with atmospheric moisture to form potassium hydroxide and oxygen is liberated. It should be stored in hermetically sealed condition under dry nitrogen. 8. PACKAGING a. 20 kgs in steel drums b. Other custom packing available SUPARNA CHEMICALS LTD 54 A Mittal Tower, Nariman Point, Mumbai India. Phone No: 022-22027446/7/8/9 Email Id: [email protected] [email protected] Potassium Superoxide (KO2) 9. SHIPPING INFORMATION a. -
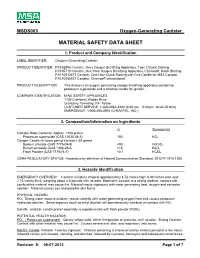
Material Safety Data Sheet
MSDS003 Oxygen-Generating Canister MATERIAL SAFETY DATA SHEET 1. Product and Company Identification LABEL IDENTIFIER: Oxygen–Generating Canister PRODUCT IDENTIFIER: P/N 92908 Canister, Navy Oxygen Breathing Apparatus, Type ll Quick Starting P/N 95710 Canister, One Hour Oxygen Breathing Apparatus, Chemox®, Quick Starting P/N 10012477 Canister, One Hour Quick Starting with One Candle for MSA Canada P/N 10065537 Canister, Chemox® International PRODUCT DESCRIPTION: This device is an oxygen generating escape breathing apparatus containing potassium superoxide and a chlorate candle for ignition. COMPANY IDENTIFICATION: MINE SAFETY APPLIANCES 1100 Cranberry Woods Drive Cranberry Township, PA 16066 CUSTOMER SERVICE: 1-800-MSA-2222 (8:30 am – 5:00 pm, local US time) EMERGENCY: 1-800-255-3924 (CHEM-TEL, INC.) 2. Composition/Information on Ingredients % Synonym(s) Canister Body Contents: Approx. 1100 grams Potassium superoxide (CAS 12030-88-5) 100 KO2 Oxygen Candle (In lower part of canister): 50 grams Sodium chlorate (CAS 7775-09-9) <90 NaClO3 Barium peroxide (CAS 1304-29-6) <10 BaO2 Flash Powder (CAS 7778-74-7) <0.1 KClO4 OSHA REGULATORY STATUS: Hazardous by definition of Hazard Communication Standard, 29 CFR 1910.1200. 3. Hazards Identification EMERGENCY OVERVIEW: Canister is kidney shaped, approximately 8.72 inches high, 6.88 inches wide and 2.75 inches thick, weighing about 4.5 pounds with no odor. Material in canister is a strong oxidizer, contact with combustible material may cause fire. Material reacts vigorously with water generating heat, oxygen and corrosive solution. Material causes eye and possible skin burns. PHYSICAL HAZARD: KO2: Strong water reactive oxidizer, reacts violently with water generating oxygen heat and caustic potassium hydroxide solution. -

Peroxides, Su Peroxides, and Ozonides of Alkali and Alkaline Earth Metals
Peroxides, Su peroxides, and Ozonides of Alkali and Alkaline Earth Metals Il'ya Ivanovich Vol'nov Head, Laboratory of Peroxide Chemistry N. S. Kurnakov Institute of General and Inorganic Chemistry Academy of Sciences of the USSR, Moscow Translated from Russian by J. Woroncow Life Sciences Group General Dynamics/Convair Division San Diego, California Edited by A. W. Petrocelli Chief, Chemistry and Chemical Engineering Section General Dynamics / Electric Boat Division Groton, Connecticut PLENUM PRESS· NEW YORK· 1966 Born in 1913, Il'ya Ivanovich Vol'nov is head of the laboratory of peroxide chemistry of the N. S. Kurnakov Institute of General and Inorganic Chem istry of the Academy of Sciences of the USSR in Moscow. He joined the Institute in 1939 and since 1949 he has authored more than 50 articles dealing with the chemistry of the inorganic peroxides, superoxides, and ozonides. Vol'nov served as editor for the proceedings of the 2nd All-Union Conference on the Chemistry of Peroxide Compounds, published by the Academy of Sciences in 1963. He was also editor of T. A. Dobrynina's monograph on Lithium Peroxide, published in 1964, and edited a biblio graphical index covering the world-wide literature for the period 1956 to 1962 on the chemistry of peroxide compounds ( other than hydrogen peroxide) published under the auspices of the library of the Academy of Sciences of the USSR. ISBN 978-1-4684-8254-6 ISBN 978-1-4684-8252-2 (eBook) DOl 10.10071978-1-4684-8252-2 Library of Congress Catalog Card Number 66-22125 The original Russian text, first published for the N. -

Peroxide Formers and Other Potential Explosives SOP
Peroxide Formers and Other Potential Explosives SOP SCOPE/PURPOSE Scope: Any academic department that uses the types of chemicals defined herein. Purpose: Certain solvents and other chemicals are known to form potentially explosive peroxides. Many of these are organic solvents; some are inorganic solids. An inhibitor is added to most peroxide-forming solvents by the manufacturer; this is usually effective until the container is first opened. After that, the inhibitor begins to be depleted. It can also become depleted during long storage without opening. High-purity solvents (e.g., HPLC grade) sometimes have no inhibitor added. The purpose of this plan is to define a peroxide former and set forth the guidelines that should be followed with regard to purchasing, storing, testing and using these chemicals. For more information, see section 4.D.3.2 and 6.G.3 in Prudent Practices in the Laboratory, The National Academies Press: 2011. DEFINITION: Peroxide structures present an explosive hazard. If they are present in a solvent, the hazard is compounded by the presence of a flammable liquid along with the explosive substance. Peroxides are also often shock sensitive compounds that can explode if subjected to mechanical shock, intense light, rapid changes in temperature, heat, friction, or in some cases, by spontaneous reaction. Chemicals that can potentially form peroxides (peroxidizables) are categorized into three classes (A-C) defined below. Included below are examples of chemicals in each class. Below are examples of chemicals in each class. These lists are not comprehensive. Class A: Class A peroxide formers are chemicals that form explosive levels of peroxides without concentration (in other words, without having been concentrated by evaporation or distillation). -

Highly Efficient Conversion of Superoxide to Oxygen Using Hydrophilic Carbon Clusters
Highly efficient conversion of superoxide to oxygen using hydrophilic carbon clusters Errol L. G. Samuela,1, Daniela C. Marcanoa,b,1, Vladimir Berkac,1, Brittany R. Bitnerd,e, Gang Wuc, Austin Pottera, Roderic H. Fabianf,g, Robia G. Pautlerd,e, Thomas A. Kentd,f,g,2, Ah-Lim Tsaic,2, and James M. Toura,b,2 aDepartment of Chemistry and bSmalley Institute for Nanoscale Science and Technology, Rice University, Houston, TX 77005; cHematology, Internal Medicine, University of Texas Houston Medical School, Houston, TX 77030; dInterdepartmental Program in Translational Biology and Molecular Medicine and Departments of eMolecular Physiology and Biophysics and fNeurology, Baylor College of Medicine, Houston, TX 77030; and gCenter for Translational Research in Inflammatory Diseases, Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX 77030 Edited* by Robert F. Curl, Rice University, Houston, TX, and approved January 12, 2015 (received for review September 8, 2014) Many diseases are associated with oxidative stress, which occurs these data, we estimate that there are 2,000–5,000 sp2 carbon when the production of reactive oxygen species (ROS) over- atoms on each PEG-HCC core. We have demonstrated the •− whelms the scavenging ability of an organism. Here, we evaluated efficacy of PEG-HCCs for normalizing in vivo O2 in models the carbon nanoparticle antioxidant properties of poly(ethylene of traumatic brain injury with concomitant hypotension. Si- • glycolated) hydrophilic carbon clusters (PEG-HCCs) by electron multaneously, we observed normalization in NO levels in paramagnetic resonance (EPR) spectroscopy, oxygen electrode, these experiments (26, 27). A better understanding of these and spectrophotometric assays. These carbon nanoparticles have 1 materials is necessary to potentially translate these thera- •− equivalent of stable radical and showed superoxide (O2 ) dismu- peutic findings to the clinic. -

HDMSP00030591 R
SUMMARY OF NFORMATION ON THE SUPEROXIDES OF SODIUM, POTASSIUM AND Na K "Compiled By : E. L . Reed Liquid Metals Information Center October 16, 1969 HDMSP00030591 r i OF CONTENT' Page In .- ociuction . Sc' :cteclilYReference Abstract ~hec :_ . PC ..3SSLMan hUD 'OhldC . - F . e - . I . Sodium Superoxide . Rate of Fo_ :_i_on of Superoxides . I . .ardour C;:wmical Reactions Involving Na, K, or NaK . b , ;H_ Documcntec . ~xi)losions Attributed to Potassium Superoxide 6 VIII. INK - Pipe-Thread - Sealant Explosions . 7 IX. Recommended Cleaning Procedures for K, Rb and C s Containers . 7 a Experimental Study of NaK Hazards . 8 XI. General Reactions of Na , K, and NaK with Organi c Compounds . 9 Resc rences . 1 0 .ca , A Ti ._uty-three Technical Report Index/ Abstract Sheets A~ - Preparation of Sodium Superoxid e A- - Excerpts from Sodium and Nat1 Engineering Handbook (Should not be further dissern i .iated ) A4 - p=rivate communication from MSA Research Corp ., Evans City, Pa. regarding potassium superoxides AS - Excerpts from Manual of Hazardous Chemical Reactions (1968 ) A6 - USAF C Bulletin No . 251 , "Explosions Involving Metallic K o r Ai - USAEC Bulletin No . 222, "NaK Reacts Explosively with Pipe Thread Sealant " AS - MSA Bulletin, "Cleaning Procedures for K , Rb, and Cs , : ntainers," (May i9 :2 ) A9 - Soc .Ur- Potassium Alloy . An Experimental Study of t-s Hazards (Feb. 1957 ) Ai0 - MSA Bulletin MD-65-1, "NaK and Potassium Technical Bulletin" All - Ethyl Corporation Bulletin, Reactions of Sodium with C :ganic Compounds" HDMSP00030592 INTRODUCTIO N 'ot Muni alloys of±so.lium and potassium (NaK) wil l e a <tu fa. -

Defect Chemistry in Alkali Peroxides and Superoxides
Defect Chemistry in Alkali Peroxides and Superoxides Von der Fakultät Chemie der Universität Stuttgart zur Erlangung der Würde eines Doktors der Naturwissenschaften (Dr. rer. nat.) genehmigte Abhandlung Vorgelegt von Oliver Gerbig aus Darmstadt Hauptberichter: Prof. Dr. J. Maier Mitberichter: Prof. Dr. J. Bill Prüfungsvorsitzender: Prof. Dr. J. van Slageren Tag der Einreichung: 28. Februar 2014 Tag der mündlichen Prüfung: 7. Mai 2014 Max-Planck-Institut für Festkörperforschung Stuttgart 2014 Erklärung Die vorliegende Doktorarbeit wurde vom Autor selbst in der Abteilung von Prof. J. Maier am Max- Planck-Institut für Festkörperforschung im Zeitraum von Januar 2010 bis März 2014 angefertigt. Der Inhalt ist die eigene Arbeit des Autors, Ausnahmen sind gekennzeichnet und wurden noch nicht zur Erlangung einer Qualifizierung oder eines Titels an der einer akademischen Institution eingereicht. Stuttgart, den 28. Februar 2014 Oliver Gerbig Declaration The work described in this thesis was carried out by the author in the Department of Prof. J. Maier at the Max Planck Institute for Solid State Research from January 2010 to March 2014. The content is the original work of the author except where indicated otherwise and has not been previously submitted to obtain any other degree or qualification at any academic institution. Stuttgart, 28th February 2014 Oliver Gerbig Table of Contents 1 Introduction and Motivation ........................................................................................................... 1 1.1 Inorganic Peroxides and -

Charge Transport in Alkali-Metal Superoxides
Article Cite This: Chem. Mater. XXXX, XXX, XXX−XXX pubs.acs.org/cm Charge Transport in Alkali-Metal Superoxides: A Systematic First- Principles Study # ¶ † ¶ # # Nicolai Rask Mathiesen, , Sheng Yang, , Juan Maria García-Lastra,*, Tejs Vegge, ‡ § ∥ ⊥ # and Donald J. Siegel*, , , , , † ‡ § ∥ Department of Physics, Mechanical Engineering Department, Materials Science & Engineering, Applied Physics Program, and ⊥ University of Michigan Energy Institute, University of Michigan, Ann Arbor, Michigan 48109, United States # Department of Energy Conversion and Storage, Technical University of Denmark, Fysikvej, Building 309, Kgs Lyngby 2800, Denmark *S Supporting Information ABSTRACT: Charge-transport mechanisms within the discharge prod- fl ucts of alkali-metal/O2 batteries can strongly in uence the performance of these systems. To date, discharge products comprising alkali peroxides (Li2O2 and Na2O2) and superoxides (LiO2, NaO2, and KO2) have been observed. In general, cells that discharge to a superoxide exhibit lower overpotentials than those that form the corresponding peroxide. These lower overpotentials have been hypothesized to originate from more efficient charge transport within the superoxides. While the transport mechanisms in the peroxides have been well studied, consensus regarding the intrinsic conductivity across the alkali-metal superoxides is lacking. Here, we present a systematic first-principles study of charge-transport mechanisms across the alkali-metal (Li, Na, K) superoxides. Our study draws on our prior investigations of the alkali peroxides and of sodium superoxide, while adding new analyses for lithium and potassium superoxides (LiO2 and KO2). In the case of − ff KO2, a nonsymmetrized room-temperature structure is proposed to account for a dynamic Jahn Teller e ect. Band gaps, equilibrium (charged) defect concentrations, mobilities, and intrinsic conductivities are estimated for both LiO2 and KO2. -

The Alkali Metals
INTERCHAPTER D The Alkali Metals The alkali metals are soft. Here we see sodium being cut with a knife. University Science Books, ©2011. All rights reserved. www.uscibooks.com D. THE ALKALI METALS D1 The website Periodic Table Live! is a good supple- ment to much of the material in this Interchapter. A link to this website can be found at www.McQuarrieGeneralChemistry.com. The alkali metals are lithium, sodium, potassium, rubidium, cesium, and francium. They occur in Group 1 of the periodic table and so have an ionic charge of +1 in their compounds. All the alkali metals are very reactive. None occur as the free metal in nature. They must be stored under an inert substance, such as kero sene, because they react spontaneously and rapidly with the oxygen and water vapor in the air. D-1. The Hydroxides of the Alkali Metals Are Strong Bases Figure D.1 Lithium floating on oil, which in turn is floating The alkali metals are all fairly soft and can be cut with on water. Lithium has the lowest density of any element a sharp knife (Frontispiece). When freshly cut they that is a solid or a liquid at 20°C. are bright and shiny, but they soon take on a dull fin ish because of their reaction with air. The alkali met als are so called because their hydroxides, MOH(s), Lithium has such a low density that it will actually float are all soluble bases in water (alkaline means basic). on oil (Figure D.1). The physical properties of the Lithium, sodium, and potassium have densities less alkali metals are given in Table D.1. -

University of Groningen Magnetic Order from Molecular Oxygen
University of Groningen Magnetic order from molecular oxygen anions Riyadi, Syarif IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2012 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Riyadi, S. (2012). Magnetic order from molecular oxygen anions. s.n. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 30-09-2021 Chapter 6 Thin Film Rubidium Oxides and Investigation of Cesium and Potassium Oxides 6.1 Introduction Among the alkali metal superoxides, the use of KO2 in breathing apparatus has been well established and widely applied. -

Nak HANDLING and REMOVAL
XA0055299 NaK HANDLING AND REMOVAL Jacqueline DESREUMAUX, Grilles RODRIGUEZ, Alain GUIGON, Janick VERDELLI, Georges THOMINE, French Atomic Energy Commission (CEA) Nuclear Reactor Division, Reactor Studies Department, Liquid Metals Technology Service, Centre d'Etudes de Cadarache 13108 Saint Paul lez Durance France. Abstract Sodium-potassium alloy is used in specific application in French Fast Breeder Reactors as: - cold traps, - NaK bubbler for argon purification, - valves and also in experimental irradiation devices.lt has been preferred to sodium because it is liquid from + 7 °C for the most common peritectic alloy.After its use, NaK is considered as a hazardous waste (nuclear or not) due to its high reactivity with air and water. The most important risk remains in handling NaK systems which have not been operated for some time.The NaK will be covered with a crust of the superoxide K02 which is a strong oxidising agent. Thermodynamically, K02 will react with most organic material or metallic dust or swarfs and can also react with additional NaK to give sufficient heat to boil part of the NaK, resulting in a sudden increase in pressure and small explosions. We describe the formation given to experimenters in our Sodium School and the CEA's experience in treating specific devices for transportation, decanting of tanks, tank opening and NaK removal. 1. INTRODUCTION Amongst the liquid metals used in fast reactors, sodium-potassium alloy (NaK) is used in specific applications such as the cooling of cold traps, valves or bubble chambers to purify argon. NaK is also used in special irradiation devices. The most commonly used mixture is the peritectic alloy which has a 52 % K mass composition (40% atomic) which has a fusion temperature of 6.9 °C, and is liquid up to 810 °C under normal pressure.