A Randomized Placebo-Controlled Phase 3 Trial of an Antisense
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Exon Skipping by Overexpression of a Drosophila Heterogeneous Nuclear
Proc. Natl. Acad. Sci. USA Vol. 92, pp. 1822-1825, March 1995 Biochemistry Exon skipping by overexpression of a Drosophila heterogeneous nuclear ribonucleoprotein in vivo (alternative splicing/dopa decarboxylase) JIE SHEN*, KAI Zut, CYNTHIA L. CASSt, ANN L. BEYERt, AND JAY HIRSH*t Departments of *Biology and tMicrobiology, University of Virginia, Charlottesville, VA 22903 Communicated by Oscar L. Miller, Jr., University of Virginia, Charlottesville, VA, November 28, 1994 (received for review September 15, 1994) ABSTRACT Heterogeneous nuclear ribonucleoproteins and a glycine-rich carboxyl-terminal domain (22-27). How- (hnRNPs) are abundant RNA-binding proteins that are im- ever, none of these Drosophila hnRNPs display sufficient plicated in splicing regulation. Here we investigate the role of sequence similarity to any vertebrate hnRNPs to determine a Drosophila hnRNP in splicing regulation in living animals. whether they are homologues of distinctive vertebrate We find that overexpression of the Drosophila hnRNP hnRNPs. The HRB98DE protein, which has 58% sequence HRB98DE leads to skipping of all internal exons in the identity with the rat Al protein in the RNA-binding domains, Drosophila dopa decarboxylase (Ddc) pre-mRNA in vivo. These is probably the closest relative of Al in D. melanogaster (25). results indicate that HRB98DE has a splicing activity that The HRB98DE gene encodes four protein isoforms derived promotes use of terminal splice sites. The effect of excess from alternative splicing and alternative use of 5' exons 1A or HRB98DE onDdc splicing is transient, even though high levels 1B. However, these HRB98DE isoforms share identical RNA- of HRB98DE persist for at least 24 hr. This suggests that binding domains. -

Sarepta Therapeutics Announces FDA Acceptance of Casimersen (SRP-4045) New Drug Application for Patients with Duchenne Muscular Dystrophy Amenable to Skipping Exon 45
Sarepta Therapeutics Announces FDA Acceptance of Casimersen (SRP-4045) New Drug Application for Patients with Duchenne Muscular Dystrophy Amenable to Skipping Exon 45 8/25/20 -- FDA grants Priority Review Status and sets regulatory action date for February 25, 2021 -- -- FDA has indicated it does not currently plan to hold an advisory committee meeting to discuss the application -- -- Received FDA's conditional approval of AMONDYS 45™ as brand name for casimersen -- -- Casimersen has been studied for the treatment of exon 45 amenable patients, approximately eight percent of patients with Duchenne -- CAMBRIDGE, Mass., Aug. 25, 2020 (GLOBE NEWSWIRE) -- Sarepta Therapeutics, Inc. (NASDAQ:SRPT), the leader in precision genetic medicine for rare diseases, today announced the U.S. Food and Drug Administration (FDA) has accepted the Company’s New Drug Application (NDA) seeking accelerated approval for casimersen (SRP-4045) and provided a regulatory action date of February 25, 2021. The FDA has indicated it does not currently plan to hold an advisory committee to discuss the application. In addition, the Company has received conditional approval of AMONDYS 45 as the brand name for casimersen. Casimersen, a phosphorodiamidate morpholino oligomer (PMO), is engineered to treat patients with Duchenne muscular dystrophy (DMD) who have genetic mutations that are amenable to skipping exon 45 of the dystrophin gene. The Company submitted its NDA filing in June 2020 and requested priority review, which the FDA granted. The NDA included data from the casimersen arm of the ESSENCE study (also known as Study 4045-301), a global, randomized, double-blind, placebo-controlled Phase 3 study evaluating the efficacy and safety of casimersen in patients amenable to skipping exons 45. -

Analysis of Exonic Mutations Leading to Exon Skipping in Patients with Pyruvate Dehydrogenase E1␣ Deficiency
0031-3998/00/4806-0748 PEDIATRIC RESEARCH Vol. 48, No. 6, 2000 Copyright © 2000 International Pediatric Research Foundation, Inc. Printed in U.S.A. Analysis of Exonic Mutations Leading to Exon Skipping in Patients with Pyruvate Dehydrogenase E1␣ Deficiency ALESSANDRA KUPPER CARDOZO, LINDA DE MEIRLEIR, INGE LIEBAERS, AND WILLY LISSENS Center for Medical Genetics [A.K.C., L.D.M., I.L., W.L.] and Pediatric Neurology [L.D.M.], University Hospital, Vrije Universiteit Brussel, 1090 Brussels, Belgium. ABSTRACT The pyruvate dehydrogenase (PDH) complex is situated at a mutations that either reverted or disrupted the wild-type pre- key position in energy metabolism and is responsible for the dicted pre-mRNA secondary structure of exon 6, we were unable conversion of pyruvate to acetyl CoA. In the literature, two to establish a correlation between the aberrant splicing and unrelated patients with a PDH complex deficiency and splicing disruption of the predicted structure. The mutagenic experiments out of exon 6 of the PDH E1␣ gene have been described, described here and the silent mutation found in one of the although intronic/exonic boundaries on either side of exon 6 patients suggest the presence of an exonic splicing enhancer in were completely normal. Analysis of exon 6 in genomic DNA of the middle region of exon 6 of the PDH E1␣ gene. (Pediatr Res these patients revealed two exonic mutations, a silent and a 48: 748–753, 2000) missense mutation. Although not experimentally demonstrated, the authors in both publications suggested that the exonic muta- tions were responsible for the exon skipping. In this work, we Abbreviations were able to demonstrate, by performing splicing experiments, ESE, exonic splicing enhancer that the two exonic mutations described in the PDH E1␣ gene mfe, minimum free energy lead to aberrant splicing. -

Increased Dystrophin Production with Golodirsen in Patients with Duchenne Muscular Dystrophy
Published Ahead of Print on March 5, 2020 as 10.1212/WNL.0000000000009233 ARTICLE OPEN ACCESS CLASS OF EVIDENCE Increased dystrophin production with golodirsen in patients with Duchenne muscular dystrophy Diane E. Frank, PhD, Frederick J. Schnell, PhD, Cody Akana, BS, Saleh H. El-Husayni, BS, Correspondence Cody A. Desjardins, PhD, Jennifer Morgan, PhD, Jay S. Charleston, PhD, Valentina Sardone, PhD, Dr. Muntoni Joana Domingos, MD, George Dickson, PhD, Volker Straub, MD, Michela Guglieri, Eugenio Mercuri, MD, [email protected] Laurent Servais, PhD, and Francesco Muntoni, MD, on behalf of the SKIP-NMD Study Group Neurology® 2020;00:1-13. doi:10.1212/WNL.0000000000009233 Abstract MORE ONLINE Objective Class of Evidence To report safety, pharmacokinetics, exon 53 skipping, and dystrophin expression in golodirsen- Criteria for rating treated patients with Duchenne muscular dystrophy (DMD) amenable to exon 53 skipping. therapeutic and diagnostic studies Methods NPub.org/coe Part 1 was a randomized, double-blind, placebo-controlled, 12-week dose titration of once-weekly golodirsen; part 2 is an ongoing, open-label evaluation. Safety and pharmacokinetics were primary and secondary objectives of part 1. Primary biological outcome measures of part 2 were blinded exon skipping and dystrophin protein production on muscle biopsies (baseline, week 48) evaluated, respectively, using reverse transcription PCR and Western blot and immunohistochemistry. Results Twelve patients were randomized to receive golodirsen (n = 8) or placebo (n = 4) in part 1. All from part 1 plus 13 additional patients received 30 mg/kg golodirsen in part 2. Safety findings were consistent with those previously observed in pediatric patients with DMD. -
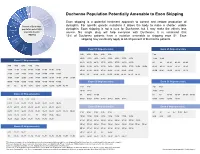
Duchenne Population Potentially Amenable to Exon Skipping
Exon 8, 2% Exon 55, 2% Exon 43, 4% Exon 52, 4% Exon 50, 4% Duchenne Population Potentially Amenable to Exon Skipping May not be Exon 44 amenable Exon skipping is a potential treatment approach to correct and restore production of to exon 6% Percent of Duchenne skipping, dystophin. For specific genetic mutations it allows the body to make a shorter, usable ~30% population potentially Exon 45 dystophin. Exon skipping is not a cure for Duchenne, but it may make the effects less 8% amenable to exon severe. No single drug will help everyone with Duchenne. It is estimated that skipping 13% of Duchenne patients have a mutation amenable to skipping exon 51. Exon Other exon skipping may eventually apply to 60-80 percent of Duchenne patients. Exon 53 skips, 8% ~20% Exon 53 Skip-amenable Exon 45 Skip-amenable 13% Exon 51 3-52 4-52 5-52 6-52 9-52 7-44 10-52 11-52 13-52 14-52 15-52 16-52 17-52 19-52 12-44 18-44 Exon 51 Skip-amenable 21-52 23-52 24-52 25-52 26-52 27-52 28-52 29-52 44 46 46-47 46-48 46-49 3-50 4-50 5-50 6-50 9-50 30-52 31-52 32-52 33-52 34-52 35-52 36-52 37-52 38-52 39-52 46-51 46-53 46-55 46-57 46-59 10-50 11-50 13-50 14-50 15-50 16-50 17-50 19-50 40-52 41-52 42-52 43-52 45-52 47-52 48-52 49-52 46-60 46-67 46-69 46-75 46-78 21-50 23-50 24-50 25-50 26-50 27-50 28-50 29-50 50-52 52 54-58 54-61 54-63 54-64 54-66 54-76 54-77 30-50 31-50 32-50 33-50 34-50 35-50 36-50 37-50 38-50 39-50 40-50 41-50 42-50 43-50 45-50 47-50 48-50 49-50 Exon 50 Skip-amenable Exon 52 Skip-amenable 50 52 52-58 52-61 52-63 52-64 52-66 52-76 52-77 2-49 8-49 2-51 -

Duchenne Muscular Dystrophy
A Guide for Individuals and Families What is... Duchenne Muscular Dystrophy Duchenne muscular dystrophy (DMD) is the Because the DMD gene is located on the most common form of muscular dystrophy. X-chromosome, it primarily affects males, It is a genetic disorder characterized by while females typically are carriers. progressive weakness However, some females can experience and degeneration of the skeletal muscles that varying degrees of physical Duchenne control movement. symptoms and are therefore called manifesting carriers. Duchenne affects approximately1 in 5,000 live male births. It is estimated that DMD typically is inherited through the about 20,000 children are diagnosed with mother; however, in about 25% of cases, the Duchenne globally each year. disease occurs spontaneously in people who do not have a family history of DMD. DMD is classified as a dystrophinopathy, a muscle disease that results from the There is no cure for DMD, but medications deficiency of a protein called dystrophin. and therapy can help manage some symptoms and potentially slow the course of In Duchenne, a mutation in the DMD the disease. gene interferes with the production of the dystrophin protein, which is needed to form and maintain healthy muscle. Lack of the dystrophin protein in muscle cells causes them to be fragile and easily damaged. What are the signs and symptoms of DMD? DMD is a multi-systemic condition affecting many parts of the body and resulting in atrophy of the skeletal, cardiac (heart), and pulmonary (lung) muscles. Nervous system Skeleton -

213026Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 213026Orig1s000 OTHER REVIEW(S) IMMUNOGENICITY ASSESSMENT Application Type NDA Application Number 213026 Submit Date 01/10/2020 Received Date 01/10/2020 Division/Office CDER/OND/ON/DNI Review Completion Date 01/10/2021 Product Name Casimersen Proposed Proprie tary AMONDYS 45 Name Error! Bookmark not defined. Pharmacologic Class PMO exon Skipping Applicant Sarepta Therapeutics, Inc. (b) (4) Applicant Proposed Duchenne muscular dystrophy (DMD) in Indication(s) patients who have a confirmed mutation of the DMD gene that is amenable to exon 45 skipping. Immunogenicity Assessors Primary Assessor(s) Seth Thacker PhD Secondary Assessor (s) Daniela Verthelyi PhD MD Assessor Recommendation: The sponsor has submitted data for anti-dystrophin antibodies in the casimersen trials. These data were generated using assays that were developed for assessing anti-dystrophin antibodies in patients treated with eteplirsen and golodirsen and have already been deemed fit for use. The sponsor submitted anti-dystrophin ADA data for Study 4045-101, which had 12 patients enrolled No positive samples were found. The FPR for these assays in Study 4045-101 were 1.3%(IgG), 7.9% (IgE), and 39% (IgM) as calculated by the assessor. The sponsors has not submitted an assay for the detection of Casimersen-specific ADAs or provided a plan on how they assess the risk associated with the generation of novel epitopes in the dystrophin formed by exon 45 skipping. PMRs will be issued to the sponsor to develop and validate the assays and to assess the patients in study 4045-101 and 4045-301 for Abs to the product and to the peptide generated through the exon skipping strategy. -

Medical Policy Eteplirsen (Exondys 51™) Injection
Medical Policy Eteplirsen (Exondys 51™) Injection SPECIALTY GUIDELINE MANAGEMENT Eteplirsen (Exondys 51™) Background: Eteplirsen (Exondys 51™) is a new antisense oligonucleotide indicated for the treatment of Duchenne muscular dystrophy (DMD), a recessive X-linked myopathy in which a person is unable to properly synthesize dystrophin, a protein essential to the maintenance of muscle cell membrane integrity, and thus suffers progressive muscle deterioration. Eteplirsen is designed to facilitate functional dystrophin production by causing gene expression to skip exon 51 on the DMD gene, the exon associated with approximately 13% of DMD-causing mutations. Authorization: Prior authorization is required for eteplirsen (Exondys 51™) requested by members enrolled in commercial (HMO, POS and PPO) products. Policy and Coverage Criteria: Initiation of Therapy: Harvard Pilgrim Health Care (HPHC) considers initiation of injected eteplirsen (Exondys 51™) as reasonable and medically necessary for the management of Duchenne muscular dystrophy (DMD) for a maximum of six months when medical record documentation confirm ALL of the following; A. Member DMD is due to mutation of the DMD gene amenable to exon 51 skipping and no other DMD- associated mutations; B. Ongoing use of a stable dose of corticosteroids going back at least six months or a contraindication to corticosteroids; C. Member is able to average a 180 meter 6-minute walk test (6MWT); D. Assessment and prescription were performed by a physician specializing in DMD; E. Dosage and use is consistent -

Skipping Multiple Exons to Treat DMD—Promises and Challenges
biomedicines Review Skipping Multiple Exons to Treat DMD—Promises and Challenges Tejal Aslesh 1, Rika Maruyama 1 and Toshifumi Yokota 1,2,* ID 1 Department of Medical Genetics, Faculty of Medicine and Dentistry, University of Alberta, 8812-112 St. Edmonton, AB T6G 2H7, Canada; [email protected] (T.A.); [email protected] (R.M.) 2 The Friends of Garret Cumming Research and Muscular Dystrophy Canada HM Toupin Neurological Science Research Chair, 8812-112 St. Edmonton, AB T6G 2H7, Canada * Correspondence: [email protected]; Tel.: +1-780-492-1102 Received: 29 November 2017; Accepted: 19 December 2017; Published: 2 January 2018 Abstract: Duchenne muscular dystrophy (DMD) is a lethal disorder caused by mutations in the DMD gene. Antisense-mediated exon-skipping is a promising therapeutic strategy that makes use of synthetic nucleic acids to skip frame-disrupting exon(s) and allows for short but functional protein expression by restoring the reading frame. In 2016, the U.S. Food and Drug Administration (FDA) approved eteplirsen, which skips DMD exon 51 and is applicable to approximately 13% of DMD patients. Multiple exon skipping, which is theoretically applicable to 80–90% of DMD patients in total, have been demonstrated in animal models, including dystrophic mice and dogs, using cocktail antisense oligonucleotides (AOs). Although promising, current drug approval systems pose challenges for the use of a cocktail AO. For example, both exons 6 and 8 need to be skipped to restore the reading frame in dystrophic dogs. Therefore, the cocktail of AOs targeting these exons has a combined therapeutic effect and each AO does not have a therapeutic effect by itself. -

Splicing Inhibition of U2AF Leads to Alternative Exon Skipping
Splicing inhibition of U2AF65 leads to alternative exon skipping Sunghee Choa, Heegyum Moona, Tiing Jen Loha, Ha Na Janga, Yongchao Liua, Jianhua Zhoub, Takbum Ohnc, Xuexiu Zhenga, and Haihong Shena,1 aSchool of Life Sciences, Gwangju Institute of Science and Technology, Gwangju 500-712, Korea; bJiangSu Key Laboratory of Neuroregeneration, Nantong University, Nantong 226001, China; and cDepartment of Cellular & Molecular Medicine, College of Medicine, Chosun University, Gwangju 501-759, Korea Edited by Michael R. Green, University of Massachusetts Medical School, Worcester, MA, and approved June 11, 2015 (received for review January 11, 2015) U2 snRNP auxiliary factor 65 kDa (U2AF65) is a general splicing factor mutations in SMN2 pre-mRNA cause predominantly skipping of that contacts polypyrimidine (Py) tract and promotes prespliceo- exon 7, which produces SMNΔ7, a truncated and less stable pro- some assembly. In this report, we show that U2AF65 stimulates al- tein with reduced self-oligomerization activity. Alternative exon 7 ternative exon skipping in spinal muscular atrophy (SMA)-related splicing of SMN pre-mRNA was modulated by orchestrated RNA– survival motor neuron (SMN) pre-mRNA. A stronger 5′ splice-site protein and protein–protein interactions, secondary structures of mutation of alternative exon abolishes the stimulatory effects of RNA, and RNA sequences (25–27). Among the mutations on U2AF65. U2AF65 overexpression promotes its own binding only on SMN2 pre-mRNA, the most functionally understood one is the the weaker, not the stronger, Py tract. We further demonstrate C-to-U point mutation on exon 7, which plays an important role in that U2AF65 inhibits splicing of flanking introns of alternative exon alternative splicing of exon 7 (25–27). -

Theoretical Applicability of CRISPR-Mediated Exon Skipping in Duchenne Muscular Dystrophy
University of Arkansas, Fayetteville ScholarWorks@UARK Biomedical Engineering Undergraduate Honors Theses Biomedical Engineering 5-2020 Theoretical Applicability of CRISPR-Mediated Exon Skipping in Duchenne Muscular Dystrophy Andrew Greek Follow this and additional works at: https://scholarworks.uark.edu/bmeguht Part of the Other Biomedical Engineering and Bioengineering Commons Citation Greek, A. (2020). Theoretical Applicability of CRISPR-Mediated Exon Skipping in Duchenne Muscular Dystrophy. Biomedical Engineering Undergraduate Honors Theses Retrieved from https://scholarworks.uark.edu/bmeguht/87 This Thesis is brought to you for free and open access by the Biomedical Engineering at ScholarWorks@UARK. It has been accepted for inclusion in Biomedical Engineering Undergraduate Honors Theses by an authorized administrator of ScholarWorks@UARK. For more information, please contact [email protected]. Theoretical Applicability of CRISPR-Mediated Exon Skipping in Duchenne Muscular Dystrophy Honors Thesis by Andrew Greek Department of Biomedical Engineering College of Engineering University of Arkansas Faculty Mentor: Dr. Christopher Nelson Honors Coordinator: Dr. Kyle Quinn 1 Table of Contents 1. Abstract ……………………………………………………….... 3 2. Introduction ………………………………………………………… 4 2.1. Muscular Dystrophy ………………………………………… 4 2.2. CRISPR and Exon Skipping ………………………………… 5 3. Materials and Methods ………………………………………… 5 3.1. Data Formatting ………………………………………………… 5 3.2. Mapping the Mutations ………………………………………… 6 3.3. Modelling Exon Skipping ………………………………… 8 4. Results -

SRP-4045) for Patients with Duchenne Muscular Dystrophy Amenable to Skipping Exon 45
Sarepta Therapeutics Completes Submission of New Drug Application Seeking Approval of Casimersen (SRP-4045) for Patients with Duchenne Muscular Dystrophy Amenable to Skipping Exon 45 6/26/20 -- Casimersen is designed for the treatment of exon 45 amenable patients, approximately eight percent of patients with Duchenne -- -- Casimersen is the third exon-skipping medicine using the Company’s proprietary PMO RNA-based platform -- CAMBRIDGE, Mass., June 26, 2020 (GLOBE NEWSWIRE) -- Sarepta Therapeutics, Inc. (NASDAQ:SRPT), the leader in precision genetic medicine for rare diseases, today announced the Company has completed the submission of a rolling New Drug Application (NDA) to the U.S. Food and Drug Administration (FDA) seeking accelerated approval for casimersen (SRP-4045). Casimersen, a phosphorodiamidate morpholino oligomer (PMO), is engineered to treat patients with Duchenne muscular dystrophy (DMD) who have genetic mutations that are amenable to skipping exon 45 of the Duchenne gene. The completion of the rolling submission includes data from the casimersen arm of the ESSENCE study (also known as study 4045-301), a global, randomized, double-blind, placebo-controlled Phase 3 study evaluating efficacy and safety in patients amenable to skipping exons 45 and 53. An interim analysis from ESSENCE demonstrated a statistically significant increase in dystrophin production as measured by western blot in patients who received casimersen compared to baseline and placebo. The study is ongoing, and remains blinded to collect additional efficacy and safety data. If the casimersen NDA is accepted and granted accelerated approval, the completed ESSENCE study will serve as a post-marketing confirmatory study. “The completion of our casimersen submission is an important milestone in our journey to advance treatments for the greatest possible number of people living with Duchenne muscular dystrophy,” said Doug Ingram, president and chief executive officer, Sarepta Therapeutics.