Deoxyuridine Nucleotides Induce Exon-Skipping I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Exon Skipping by Overexpression of a Drosophila Heterogeneous Nuclear
Proc. Natl. Acad. Sci. USA Vol. 92, pp. 1822-1825, March 1995 Biochemistry Exon skipping by overexpression of a Drosophila heterogeneous nuclear ribonucleoprotein in vivo (alternative splicing/dopa decarboxylase) JIE SHEN*, KAI Zut, CYNTHIA L. CASSt, ANN L. BEYERt, AND JAY HIRSH*t Departments of *Biology and tMicrobiology, University of Virginia, Charlottesville, VA 22903 Communicated by Oscar L. Miller, Jr., University of Virginia, Charlottesville, VA, November 28, 1994 (received for review September 15, 1994) ABSTRACT Heterogeneous nuclear ribonucleoproteins and a glycine-rich carboxyl-terminal domain (22-27). How- (hnRNPs) are abundant RNA-binding proteins that are im- ever, none of these Drosophila hnRNPs display sufficient plicated in splicing regulation. Here we investigate the role of sequence similarity to any vertebrate hnRNPs to determine a Drosophila hnRNP in splicing regulation in living animals. whether they are homologues of distinctive vertebrate We find that overexpression of the Drosophila hnRNP hnRNPs. The HRB98DE protein, which has 58% sequence HRB98DE leads to skipping of all internal exons in the identity with the rat Al protein in the RNA-binding domains, Drosophila dopa decarboxylase (Ddc) pre-mRNA in vivo. These is probably the closest relative of Al in D. melanogaster (25). results indicate that HRB98DE has a splicing activity that The HRB98DE gene encodes four protein isoforms derived promotes use of terminal splice sites. The effect of excess from alternative splicing and alternative use of 5' exons 1A or HRB98DE onDdc splicing is transient, even though high levels 1B. However, these HRB98DE isoforms share identical RNA- of HRB98DE persist for at least 24 hr. This suggests that binding domains. -

Sarepta Therapeutics Announces FDA Acceptance of Casimersen (SRP-4045) New Drug Application for Patients with Duchenne Muscular Dystrophy Amenable to Skipping Exon 45
Sarepta Therapeutics Announces FDA Acceptance of Casimersen (SRP-4045) New Drug Application for Patients with Duchenne Muscular Dystrophy Amenable to Skipping Exon 45 8/25/20 -- FDA grants Priority Review Status and sets regulatory action date for February 25, 2021 -- -- FDA has indicated it does not currently plan to hold an advisory committee meeting to discuss the application -- -- Received FDA's conditional approval of AMONDYS 45™ as brand name for casimersen -- -- Casimersen has been studied for the treatment of exon 45 amenable patients, approximately eight percent of patients with Duchenne -- CAMBRIDGE, Mass., Aug. 25, 2020 (GLOBE NEWSWIRE) -- Sarepta Therapeutics, Inc. (NASDAQ:SRPT), the leader in precision genetic medicine for rare diseases, today announced the U.S. Food and Drug Administration (FDA) has accepted the Company’s New Drug Application (NDA) seeking accelerated approval for casimersen (SRP-4045) and provided a regulatory action date of February 25, 2021. The FDA has indicated it does not currently plan to hold an advisory committee to discuss the application. In addition, the Company has received conditional approval of AMONDYS 45 as the brand name for casimersen. Casimersen, a phosphorodiamidate morpholino oligomer (PMO), is engineered to treat patients with Duchenne muscular dystrophy (DMD) who have genetic mutations that are amenable to skipping exon 45 of the dystrophin gene. The Company submitted its NDA filing in June 2020 and requested priority review, which the FDA granted. The NDA included data from the casimersen arm of the ESSENCE study (also known as Study 4045-301), a global, randomized, double-blind, placebo-controlled Phase 3 study evaluating the efficacy and safety of casimersen in patients amenable to skipping exons 45. -

Analysis of Exonic Mutations Leading to Exon Skipping in Patients with Pyruvate Dehydrogenase E1␣ Deficiency
0031-3998/00/4806-0748 PEDIATRIC RESEARCH Vol. 48, No. 6, 2000 Copyright © 2000 International Pediatric Research Foundation, Inc. Printed in U.S.A. Analysis of Exonic Mutations Leading to Exon Skipping in Patients with Pyruvate Dehydrogenase E1␣ Deficiency ALESSANDRA KUPPER CARDOZO, LINDA DE MEIRLEIR, INGE LIEBAERS, AND WILLY LISSENS Center for Medical Genetics [A.K.C., L.D.M., I.L., W.L.] and Pediatric Neurology [L.D.M.], University Hospital, Vrije Universiteit Brussel, 1090 Brussels, Belgium. ABSTRACT The pyruvate dehydrogenase (PDH) complex is situated at a mutations that either reverted or disrupted the wild-type pre- key position in energy metabolism and is responsible for the dicted pre-mRNA secondary structure of exon 6, we were unable conversion of pyruvate to acetyl CoA. In the literature, two to establish a correlation between the aberrant splicing and unrelated patients with a PDH complex deficiency and splicing disruption of the predicted structure. The mutagenic experiments out of exon 6 of the PDH E1␣ gene have been described, described here and the silent mutation found in one of the although intronic/exonic boundaries on either side of exon 6 patients suggest the presence of an exonic splicing enhancer in were completely normal. Analysis of exon 6 in genomic DNA of the middle region of exon 6 of the PDH E1␣ gene. (Pediatr Res these patients revealed two exonic mutations, a silent and a 48: 748–753, 2000) missense mutation. Although not experimentally demonstrated, the authors in both publications suggested that the exonic muta- tions were responsible for the exon skipping. In this work, we Abbreviations were able to demonstrate, by performing splicing experiments, ESE, exonic splicing enhancer that the two exonic mutations described in the PDH E1␣ gene mfe, minimum free energy lead to aberrant splicing. -

Opportunities and Challenges for Antisense Oligonucleotide Therapies
Received: 10 January 2020 Revised: 23 April 2020 Accepted: 8 May 2020 DOI: 10.1002/jimd.12251 REVIEW ARTICLE Opportunities and challenges for antisense oligonucleotide therapies Elsa C. Kuijper1 | Atze J. Bergsma2,3 | W.W.M. Pim Pijnappel2,3 | Annemieke Aartsma-Rus1 1Department of Human Genetics, Leiden University Medical Center, Leiden, The Abstract Netherlands Antisense oligonucleotide (AON) therapies involve short strands of modi- 2Department of Pediatrics, Center for fied nucleotides that target RNA in a sequence-specific manner, inducing Lysosomal and Metabolic Diseases, targeted protein knockdown or restoration. Currently, 10 AON therapies Erasmus Medical Center, Rotterdam, The Netherlands have been approved in the United States and Europe. Nucleotides are chem- 3Department of Clinical Genetics, Center ically modified to protect AONs from degradation, enhance bioavailability for Lysosomal and Metabolic Diseases, and increase RNA affinity. Whereas single stranded AONs can efficiently Erasmus Medical Center, Rotterdam, The Netherlands be delivered systemically, delivery of double stranded AONs requires capsulation in lipid nanoparticles or binding to a conjugate as the uptake Correspondence enhancing backbone is hidden in this conformation. With improved chem- Annemieke Aartsma-Rus, LUMC Postzone S4-P, Albinusdreef 2, 2333 ZA istry, delivery vehicles and conjugates, doses can be lowered, thereby reduc- Leiden, The Netherlands. ing the risk and occurrence of side effects. AONs can be used to knockdown Email: [email protected] or restore levels of protein. Knockdown can be achieved by single stranded Communicating Editor: Carla E. Hollak or double stranded AONs binding the RNA transcript and activating RNaseH-mediated and RISC-mediated degradation respectively. Transcript binding by AONs can also prevent translation, hence reducing protein levels. -

The Use of Ataluren in the Effective Management of Duchenne Muscular Dystrophy
Review Neuromuscular Diseases Early Diagnosis and Treatment – The Use of Ataluren in the Effective Management of Duchenne Muscular Dystrophy Eugenio Mercuri,1 Ros Quinlivan2 and Sylvie Tuffery-Giraud3 1. Catholic University, Rome, Italy; 2. Great Ormond Street Hospital and National Hospital for Neurology and Neurosurgery, London, UK; 3. Laboratory of Genetics of Rare Diseases (LGMR), University of Montpellier, Montpellier, France DOI: https://doi.org/10.17925/ENR.2018.13.1.31 he understanding of the natural history of Duchenne muscular dystrophy (DMD) is increasing rapidly and new treatments are emerging that have the potential to substantially improve the prognosis for patients with this disabling and life-shortening disease. For many, Thowever, there is a long delay between the appearance of symptoms and DMD diagnosis, which reduces the possibility of successful treatment. DMD results from mutations in the large dystrophin gene of which one-third are de novo mutations and two-thirds are inherited from a female carrier. Roughly 75% of mutations are large rearrangements and 25% are point mutations. Certain deletions and nonsense mutations can be treated whereas many other mutations cannot currently be treated. This emphasises the need for early genetic testing to identify the mutation, guide treatment and inform genetic counselling. Treatments for DMD include corticosteroids and more recently, ataluren has been approved in Europe, the first disease-modifying therapy for treating DMD caused by nonsense mutations. The use of ataluren in DMD is supported by positive results from phase IIb and phase III studies in which the treatment produced marked improvements in the 6-minute walk test, timed function tests such as the 10 m walk/run test and the 4-stair ascent/descent test compared with placebo. -

Are Speci C Symptoms and Signs That Will Enable the Clinician to Recognise Disease Patterns That Will Narrow Down the Differenti
CHILDHOOD DEVELOPMENTAL SCREENING 2020 https://doi.org/10.33591/sfp.46.5.u5 UNIT NO. 5 Brumbaugh D, Case LE, Clemens PR, Hadjiyannakis S, Pandya S, Street CHILDHOOD NEUROMUSCULAR DISORDERS examiner’s hands under the armpits and assessed for any arm periodic paralysis) and the rate of progression. An acute or delay/hypotonia, neuroimaging with MRI brain and aordable gene panels targeting neuromuscular disorders promising, with near-normal motor development in some receptor but reduced transcriptional activation and therefore 3. Orthopaedic Care neuromuscular diseases has resulted in faster and more accurate slip sign, and an attempt should be made to see if the infant can subacute onset of symptoms may be suggestive of an endocrine appropriate chromosomal/genetic testing can be considered. which are faster and less costly than whole exome or whole infants. is has resulted in new recommendations for neonatal has less side eects of other steroids. Clinical trials are still Prevention of contractures may be aected with appropriate diagnosis. Furthermore, new treatments are in the pipeline or N. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointes- A/Prof Stacey Tay Kiat Hong bear weight on both legs. e infant is then put into ventral or inammatory myositis, the chronic onset of symptoms may 2. If the child has evidence of lower limb involvement and genome sequencing. e choice of whole exome or whole newborn screening of SMA as well as a treatment algorithm for underway for head-to-head comparison of Vamorolone and resting splints of the ankles. Proper seating is also key to are already available for certain neuromuscular disorders, and 11 20 tinal and nutritional management. -

Increased Dystrophin Production with Golodirsen in Patients with Duchenne Muscular Dystrophy
Published Ahead of Print on March 5, 2020 as 10.1212/WNL.0000000000009233 ARTICLE OPEN ACCESS CLASS OF EVIDENCE Increased dystrophin production with golodirsen in patients with Duchenne muscular dystrophy Diane E. Frank, PhD, Frederick J. Schnell, PhD, Cody Akana, BS, Saleh H. El-Husayni, BS, Correspondence Cody A. Desjardins, PhD, Jennifer Morgan, PhD, Jay S. Charleston, PhD, Valentina Sardone, PhD, Dr. Muntoni Joana Domingos, MD, George Dickson, PhD, Volker Straub, MD, Michela Guglieri, Eugenio Mercuri, MD, [email protected] Laurent Servais, PhD, and Francesco Muntoni, MD, on behalf of the SKIP-NMD Study Group Neurology® 2020;00:1-13. doi:10.1212/WNL.0000000000009233 Abstract MORE ONLINE Objective Class of Evidence To report safety, pharmacokinetics, exon 53 skipping, and dystrophin expression in golodirsen- Criteria for rating treated patients with Duchenne muscular dystrophy (DMD) amenable to exon 53 skipping. therapeutic and diagnostic studies Methods NPub.org/coe Part 1 was a randomized, double-blind, placebo-controlled, 12-week dose titration of once-weekly golodirsen; part 2 is an ongoing, open-label evaluation. Safety and pharmacokinetics were primary and secondary objectives of part 1. Primary biological outcome measures of part 2 were blinded exon skipping and dystrophin protein production on muscle biopsies (baseline, week 48) evaluated, respectively, using reverse transcription PCR and Western blot and immunohistochemistry. Results Twelve patients were randomized to receive golodirsen (n = 8) or placebo (n = 4) in part 1. All from part 1 plus 13 additional patients received 30 mg/kg golodirsen in part 2. Safety findings were consistent with those previously observed in pediatric patients with DMD. -
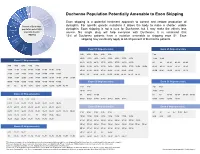
Duchenne Population Potentially Amenable to Exon Skipping
Exon 8, 2% Exon 55, 2% Exon 43, 4% Exon 52, 4% Exon 50, 4% Duchenne Population Potentially Amenable to Exon Skipping May not be Exon 44 amenable Exon skipping is a potential treatment approach to correct and restore production of to exon 6% Percent of Duchenne skipping, dystophin. For specific genetic mutations it allows the body to make a shorter, usable ~30% population potentially Exon 45 dystophin. Exon skipping is not a cure for Duchenne, but it may make the effects less 8% amenable to exon severe. No single drug will help everyone with Duchenne. It is estimated that skipping 13% of Duchenne patients have a mutation amenable to skipping exon 51. Exon Other exon skipping may eventually apply to 60-80 percent of Duchenne patients. Exon 53 skips, 8% ~20% Exon 53 Skip-amenable Exon 45 Skip-amenable 13% Exon 51 3-52 4-52 5-52 6-52 9-52 7-44 10-52 11-52 13-52 14-52 15-52 16-52 17-52 19-52 12-44 18-44 Exon 51 Skip-amenable 21-52 23-52 24-52 25-52 26-52 27-52 28-52 29-52 44 46 46-47 46-48 46-49 3-50 4-50 5-50 6-50 9-50 30-52 31-52 32-52 33-52 34-52 35-52 36-52 37-52 38-52 39-52 46-51 46-53 46-55 46-57 46-59 10-50 11-50 13-50 14-50 15-50 16-50 17-50 19-50 40-52 41-52 42-52 43-52 45-52 47-52 48-52 49-52 46-60 46-67 46-69 46-75 46-78 21-50 23-50 24-50 25-50 26-50 27-50 28-50 29-50 50-52 52 54-58 54-61 54-63 54-64 54-66 54-76 54-77 30-50 31-50 32-50 33-50 34-50 35-50 36-50 37-50 38-50 39-50 40-50 41-50 42-50 43-50 45-50 47-50 48-50 49-50 Exon 50 Skip-amenable Exon 52 Skip-amenable 50 52 52-58 52-61 52-63 52-64 52-66 52-76 52-77 2-49 8-49 2-51 -

PRAC Draft Agenda of Meeting 14-17 March 2016
14 March 2016 EMA/PRAC/199507/2016 Corr.∗ Procedure Management and Committees Support Division Pharmacovigilance Risk Assessment Committee (PRAC) Draft agenda for the meeting on 14-17 March 2016 Chair: June Raine – Vice-Chair: Almath Spooner 14 March 2016, 13:00 – 19:00, room 3/A 15 March 2016, 08:30 – 19:00, room 3/A 16 March 2016, 08:30 – 19:00, room 3/A 17 March 2016, 08:30 – 16:00, room 3/E Organisational, regulatory and methodological matters (ORGAM) 31 March 2016, 10:00 - 12:00, room 7/B, via Adobe Connect Health and safety information In accordance with the Agency’s health and safety policy, delegates are to be briefed on health, safety and emergency information and procedures prior to the start of the meeting. Disclaimers Some of the information contained in this agenda is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also change during the course of the review. Additional details on some of these procedures will be published in the PRAC meeting highlights once the procedures are finalised. Of note, this agenda is a working document primarily designed for PRAC members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the agenda cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. -

Duchenne Muscular Dystrophy
A Guide for Individuals and Families What is... Duchenne Muscular Dystrophy Duchenne muscular dystrophy (DMD) is the Because the DMD gene is located on the most common form of muscular dystrophy. X-chromosome, it primarily affects males, It is a genetic disorder characterized by while females typically are carriers. progressive weakness However, some females can experience and degeneration of the skeletal muscles that varying degrees of physical Duchenne control movement. symptoms and are therefore called manifesting carriers. Duchenne affects approximately1 in 5,000 live male births. It is estimated that DMD typically is inherited through the about 20,000 children are diagnosed with mother; however, in about 25% of cases, the Duchenne globally each year. disease occurs spontaneously in people who do not have a family history of DMD. DMD is classified as a dystrophinopathy, a muscle disease that results from the There is no cure for DMD, but medications deficiency of a protein called dystrophin. and therapy can help manage some symptoms and potentially slow the course of In Duchenne, a mutation in the DMD the disease. gene interferes with the production of the dystrophin protein, which is needed to form and maintain healthy muscle. Lack of the dystrophin protein in muscle cells causes them to be fragile and easily damaged. What are the signs and symptoms of DMD? DMD is a multi-systemic condition affecting many parts of the body and resulting in atrophy of the skeletal, cardiac (heart), and pulmonary (lung) muscles. Nervous system Skeleton -

213026Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 213026Orig1s000 OTHER REVIEW(S) IMMUNOGENICITY ASSESSMENT Application Type NDA Application Number 213026 Submit Date 01/10/2020 Received Date 01/10/2020 Division/Office CDER/OND/ON/DNI Review Completion Date 01/10/2021 Product Name Casimersen Proposed Proprie tary AMONDYS 45 Name Error! Bookmark not defined. Pharmacologic Class PMO exon Skipping Applicant Sarepta Therapeutics, Inc. (b) (4) Applicant Proposed Duchenne muscular dystrophy (DMD) in Indication(s) patients who have a confirmed mutation of the DMD gene that is amenable to exon 45 skipping. Immunogenicity Assessors Primary Assessor(s) Seth Thacker PhD Secondary Assessor (s) Daniela Verthelyi PhD MD Assessor Recommendation: The sponsor has submitted data for anti-dystrophin antibodies in the casimersen trials. These data were generated using assays that were developed for assessing anti-dystrophin antibodies in patients treated with eteplirsen and golodirsen and have already been deemed fit for use. The sponsor submitted anti-dystrophin ADA data for Study 4045-101, which had 12 patients enrolled No positive samples were found. The FPR for these assays in Study 4045-101 were 1.3%(IgG), 7.9% (IgE), and 39% (IgM) as calculated by the assessor. The sponsors has not submitted an assay for the detection of Casimersen-specific ADAs or provided a plan on how they assess the risk associated with the generation of novel epitopes in the dystrophin formed by exon 45 skipping. PMRs will be issued to the sponsor to develop and validate the assays and to assess the patients in study 4045-101 and 4045-301 for Abs to the product and to the peptide generated through the exon skipping strategy. -

Medical Policy Eteplirsen (Exondys 51™) Injection
Medical Policy Eteplirsen (Exondys 51™) Injection SPECIALTY GUIDELINE MANAGEMENT Eteplirsen (Exondys 51™) Background: Eteplirsen (Exondys 51™) is a new antisense oligonucleotide indicated for the treatment of Duchenne muscular dystrophy (DMD), a recessive X-linked myopathy in which a person is unable to properly synthesize dystrophin, a protein essential to the maintenance of muscle cell membrane integrity, and thus suffers progressive muscle deterioration. Eteplirsen is designed to facilitate functional dystrophin production by causing gene expression to skip exon 51 on the DMD gene, the exon associated with approximately 13% of DMD-causing mutations. Authorization: Prior authorization is required for eteplirsen (Exondys 51™) requested by members enrolled in commercial (HMO, POS and PPO) products. Policy and Coverage Criteria: Initiation of Therapy: Harvard Pilgrim Health Care (HPHC) considers initiation of injected eteplirsen (Exondys 51™) as reasonable and medically necessary for the management of Duchenne muscular dystrophy (DMD) for a maximum of six months when medical record documentation confirm ALL of the following; A. Member DMD is due to mutation of the DMD gene amenable to exon 51 skipping and no other DMD- associated mutations; B. Ongoing use of a stable dose of corticosteroids going back at least six months or a contraindication to corticosteroids; C. Member is able to average a 180 meter 6-minute walk test (6MWT); D. Assessment and prescription were performed by a physician specializing in DMD; E. Dosage and use is consistent