Parotid Salivary Gland and Lesions of the Facial Nerve
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Perioral Gustatory Sweating: Case Report
The Journal of Laryngology & Otology (2012), 126, 532–534. CLINICAL RECORD © JLO (1984) Limited, 2012 doi:10.1017/S0022215112000229 Perioral gustatory sweating: case report S C KÄYSER1, K J A O INGELS2, F J A VAN DEN HOOGEN2 1Department of Primary and Community Care, Radboud University Nijmegen Medical Centre, and 2Department of Otorhinolaryngology/Head and Neck Surgery, Radboud University Nijmegen Medical Centre, The Netherlands Abstract Objective: Presentation of a case of perioral Frey syndrome. Design: Case report. Subject: A 72-year-old woman with hyperhidrosis around the mouth and chin. Results: This patient suffered from bilateral perioral gustatory sweating following a mandibular osteotomy; such a case has not previously been described. Possible pathophysiological hypotheses are discussed in relation to the anatomy and innervation of the salivary glands. Conclusion: Perioral gustatory sweating is a rare complication of osteotomy. Key words: Gustatory sweating; Frey Syndrome; Perioral; Hyperhidrosis Introduction perioral excessive sweating and flushing which only Frey syndrome, also known as auriculotemporal syndrome, is a occurred during (and not preceding) eating. Her complaints well-known complication of parotid surgery. Approximately had begun following bilateral osteotomy of the mandible in 24 per cent of patients undergoing parotidectomy experience 1960, at the age of 25 years. The indication for this procedure gustatory sweating, although the reported incidence varies had been prognathism. Her recovery had been complicated greatly.1 Frey syndrome appears following a latency period by inadequate bone healing and loss of the right and left of one to 36 months (or longer) after surgery.2,3 inferior alveolar nerves (Figure 1). The aetiology of Frey syndrome is explained by ‘aberrant The diagnosis of hyperhidrosis was made using the nervous regeneration’. -

Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone Tissue Engineering
Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone tissue Engineering Elisabet Farré Guasch Dipòsit Legal: B-25086-2011 ISBN: 978-90-5335-394-3 http://hdl.handle.net/10803/31987 ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tesisenxarxa.net) ha estat autoritzada pels titulars dels drets de propietat intel·lectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tesisenred.net) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR. No se autoriza la presentación de su contenido en una ventana o marco ajeno a TDR (framing). -

The Mandibular Nerve - Vc Or VIII by Prof
The Mandibular Nerve - Vc or VIII by Prof. Dr. Imran Qureshi The Mandibular nerve is the third and largest division of the trigeminal nerve. It is a mixed nerve. Its sensory root emerges from the posterior region of the semilunar ganglion and is joined by the motor root of the trigeminal nerve. These two nerve bundles leave the cranial cavity through the foramen ovale and unite immediately to form the trunk of the mixed mandibular nerve that passes into the infratemporal fossa. Here, it runs anterior to the middle meningeal artery and is sandwiched between the superior head of the lateral pterygoid and tensor veli palatini muscles. After a short course during which a meningeal branch to the dura mater, and the nerve to part of the medial pterygoid muscle (and the tensor tympani and tensor veli palatini muscles) are given off, the mandibular trunk divides into a smaller anterior and a larger posterior division. The anterior division receives most of the fibres from the motor root and distributes them to the other muscles of mastication i.e. the lateral pterygoid, medial pterygoid, temporalis and masseter muscles. The nerve to masseter and two deep temporal nerves (anterior and posterior) pass laterally above the medial pterygoid. The nerve to the masseter continues outward through the mandibular notch, while the deep temporal nerves turn upward deep to temporalis for its supply. The sensory fibres that it receives are distributed as the buccal nerve. The 1 | P a g e buccal nerve passes between the medial and lateral pterygoids and passes downward and forward to emerge from under cover of the masseter with the buccal artery. -

An Unusual Finding of the Auriculotemporal Nerve: Possible Risk Factor During Preauricular Skin Incisions
Case Report An unusual finding of the auriculotemporal nerve: possible risk factor during preauricular skin incisions Joe Iwanaga1,2,3, Samuel L. Bobek4, Christian Fisahn1,5, Ken Nakamura3, Yoshihiro Miyazono3, R. Shane Tubbs1 1Seattle Science Foundation, Seattle, WA 98122, USA; 2Department of Anatomy, 3Dental and Oral Medical Center, Kurume University School of Medicine, Kurume, Fukuoka 830-0011, Japan; 4Swedish Maxillofacial Surgery, 5Swedish Neuroscience Institute, Swedish Medical Center, Seattle, WA 98122, USA Correspondence to: Joe Iwanaga. Seattle Science Foundation, 550 17th Ave, James Tower, Suite 600, Seattle, WA 98122, USA. Email: [email protected]. Abstract: The auriculotemporal nerve (ATN) is a branch of the mandibular nerve and has been implicated for some migraines and its role in Frey’s syndrome is well known. An adult cadaver was found to have a duplicated ATN. The anterior trunk ascended as the superficial temporal artery and gave off the branches to the temporomandibular joint, parotid gland, external acoustic meatus and temporal region and communicated with a posterior trunk of the ATN. The posterior trunk ascended via the subcutaneous tissues 1 mm anterior to the auricle and gave off the branches to the anterior auricular region, temporal region and communicated with the anterior trunk. Such a duplicated ATN might be injured with preauricular skin incisions. Knowledge of such an anatomical variation might assist surgeons in iatrogenic injury of the ATN. Keywords: Auriculotemporal nerve (ATN); infratemporal fossa; Frey’s syndrome; mandibular nerve Submitted Aug 09, 2016. Accepted for publication Aug 17, 2016. doi: 10.21037/gs.2016.09.02 View this article at: http://dx.doi.org/10.21037/gs.2016.09.02 Introduction Case presentation The auriculotemporal nerve (ATN) is one of the branches During the dissection of a cadaver that was 87-year-old at of the mandibular division (V3) of the trigeminal nerve. -

The Buccal Fat Pad: Importance and Function
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 6 Ver. XIII (June. 2016), PP 79-81 www.iosrjournals.org The Buccal Fat Pad: Importance And Function Ulduz Zamani Ahari1, Hosein Eslami2, Parisa Falsafi*2, Aila Bahramian2, Saleh Maleki1 1. Post Graduate Student Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. 2.Department Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. ●Corresponding Author Email:[email protected] Abstract: The buccal fat is an important anatomic structure intimately related to the masticatory muscles, facial nerve , and parotid duct.while anatomically complex , an understanding of its boundaries will allow the surgeon to safely manipulate this structure in reconstructive and aesthetic procedures . Technically, the buccal fat pad is easily accessed and moblized . It is does not cause any noticeable defect in the cheek or mouth, and it can be performed in a very short time and without causing complication for the patient. The pedicled BFP graft is more resistant to infection than other kinds of free graft and will result in very success. The buccal fat pad has a satisfactory vascular supply , This property of graft and other properties will allow for the closure of defects that cannot be repaired by conventional procedures. The buccal fat pad exposed through an intraoral and buccal incision , has several clinical application including aesthetic improvement , close of oroantral and Oroantral defects reconstruction of surgical defects and palatal cleft defects and palatal cleft defects , reconstruction of maxilla and palatal defects. -

(Ear) Surgery Under Local Anaesthesia
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY LOCAL AND REGIONAL ANAESTHESIA TECHNIQUES FOR OTOLOGIC (EAR) SURGERY Alexander Bien, Richard Wagner, Eric Wilkinson The logistics of performing otologic (ear) ing devices would still be needed. Again, surgery in developing countries and in this returns to the issue of safety. humanitarian settings are challenging. Im- plementing the use of local anaesthesia to Another reason is that of recovery time and perform middle ear and mastoid surgery in turnover; the ability to perform more cases such situations has many advantages. in a shorter amount of time. Time is of the essence in the humanitarian setting, even This article will outline the rationale for more so than in a Western medical setting. local anaesthesia in otologic surgery as well A humanitarian mission may be limited to a as educate the reader about local anesthetic certain number of days or even daylight agents and the anatomy of the ear that hours. The capacity to perform even one allows local anaesthesia to be an effective additional case in any given day may trans- means under which to perform otologic late into the benefit of many - depending on procedures. the duration of the outreach - more patients. No time needs to be allotted for the reversal Rationale for Local Anaesthesia of anaesthesia and the monitoring needs during recovery are minimal - limited Performing otologic procedures under local primarily to observation. Most, if not all, of anaesthesia - as opposed to general anaes- these concerns are eliminated with the use thesia - has many advantages in a humani- of purely local anaesthetic. -

ANATOMY of EAR Basic Ear Anatomy
ANATOMY OF EAR Basic Ear Anatomy • Expected outcomes • To understand the hearing mechanism • To be able to identify the structures of the ear Development of Ear 1. Pinna develops from 1st & 2nd Branchial arch (Hillocks of His). Starts at 6 Weeks & is complete by 20 weeks. 2. E.A.M. develops from dorsal end of 1st branchial arch starting at 6-8 weeks and is complete by 28 weeks. 3. Middle Ear development —Malleus & Incus develop between 6-8 weeks from 1st & 2nd branchial arch. Branchial arches & Development of Ear Dev. contd---- • T.M at 28 weeks from all 3 germinal layers . • Foot plate of stapes develops from otic capsule b/w 6- 8 weeks. • Inner ear develops from otic capsule starting at 5 weeks & is complete by 25 weeks. • Development of external/middle/inner ear is independent of each other. Development of ear External Ear • It consists of - Pinna and External auditory meatus. Pinna • It is made up of fibro elastic cartilage covered by skin and connected to the surrounding parts by ligaments and muscles. • Various landmarks on the pinna are helix, antihelix, lobule, tragus, concha, scaphoid fossa and triangular fossa • Pinna has two surfaces i.e. medial or cranial surface and a lateral surface . • Cymba concha lies between crus helix and crus antihelix. It is an important landmark for mastoid antrum. Anatomy of external ear • Landmarks of pinna Anatomy of external ear • Bat-Ear is the most common congenital anomaly of pinna in which antihelix has not developed and excessive conchal cartilage is present. • Corrections of Pinna defects are done at 6 years of age. -
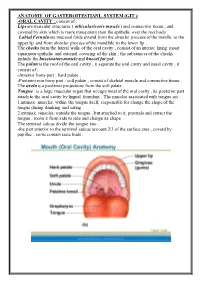
ANATOMY of GASTEROITESTIANL SYSTEM (GIT ): Consist of : ORAL CAVITY
ANATOMY OF GASTEROITESTIANL SYSTEM (GIT ): -ORAL CAVITY : consist of : Lips are muscular structures ( orbicularis oris muscle ) and connective tissue , and covered by skin which is more transparent than the epithelia over the rest body . Labial Fernula are mucosal folds extend from the alveolar process of the maxilla to the upper lip and from alveolar process of the mandible to the lower lip . The cheeks form the lateral walls of the oral cavity , consist of an interior lining moist squamous epithelia and external covering of the skin , the substances of the cheeks include the buccinators muscle and buccal fat pad. The palate is the roof of the oral cavity , it separate the oral cavity and nasal cavity , it consist of : -Anterior bony part : hard palate . -Posterior non bony part : soft palate , consist of skeletal muscle and connective tissue . The uvela is a posterior projections from the soft palate . Tongue : is a large muscular organ that occupy most of the oral cavity , its posterior part attach to the oral cavity by lingual frenulum . The muscles associated with tongue are : 1.intrinsic muscles: within the tongue itself, responsible for change the shape of the tongue during drinking and eating . 2.extrinsic muscles: outside the tongue , but attached to it, protrude and retract the tongue , move it from side to side and change its shape . The terminal sulcus divide the tongue into : -the part anterior to the terminal sulcus account 2/3 of the surface area , coverd by papillae , some contain taste buds . -the posterior one third is devoid of papillae , has few scattered taste buds , it has few small glands and lymphatic tissue (lingual tissue ) Teeth : adults have 32 teeth distributed in two dental arches, the maxillary arch , and the mandibular arch . -

Dr. E. Anitha Dr. K. Sujatha* INTERNATIONAL JOURNAL OF
ORIGINAL RESEARCH PAPER Volume - 10 | Issue - 01 | January - 2021 | PRINT ISSN No. 2277 - 8179 | DOI : 10.36106/ijsr INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH A RARE VARIATION OF AURICULOTEMPORAL NERVE IN RELATION WITH MAXILLARY ARTERY- A CADAVERIC STUDY Anatomy MBBS, M.D., Assistant Professor, Department Of Anatomy, Government Stanley Dr. E. Anitha Medical College, Chennai - 600001. MBBS, D.A,M.D., Professor And HOD Of Department Of Anatomy, Government Dr. K. Sujatha* Stanley Medical College, Chennai – 600001. *Corresponding Author ABSTRACT Auriculotemporal nerve is a branch of posterior division of the mandibular nerve. It carries sensory, secretomotor and sympathetic bres. Clinical knowledge about this nerve, its course and relationship with adjacent vessels are important for performing neurosurgery and facio- maxillary surgeries. Aim of the present study was to observe the origin of this nerve, its relation to adjacent vessels and its communication to other branches of mandibular nerve. We studied 35 cadavers of both male and female of South Indian populations which were used for routine dissection for teaching 1st year MBBS medical graduates. During the study, we found a rare variation of auriculotemporal nerve, having 3 roots, encircling the maxillary artery instead of the middle meningeal artery. Knowledge of such rare variation will denitely help the surgeons to plan their surgery and prevent injuries to both nerve and the vessel. KEYWORDS Auriculotemporal Nerve (ATN), Mandibular Nerve, Maxillary Artery, Middle Meningeal Artery, Inferior Alveolar Nerve (IAN). INTRODUCTION of auriculotemporal nerve and its communication with the inferior The Auriculotemporal nerve is a branch of posterior division of the alveolar nerve. Gulekon et al, in their study have reported 4 roots of mandibular nerve. -
Bichectomy: Achieving Aesthetic, Funcional and Psychological Results with a Simple Intraoral Surgical Procedure
Volume 1- Issue 2: 2017 DOI: 10.26717/BJSTR.2017.01.000205 Simone De Luccas. Biomed J Sci & Tech Res ISSN: 2574-1241 Opinion Open Access Bichectomy: Achieving Aesthetic, Funcional and Psychological Results with A Simple Intraoral Surgical Procedure Simone De Luccas* Dentist Surgeon, Brazil Received: July 13, 2017; Published: July 19, 2017 *Corresponding author: Simone De Luccas, Dentist Surgeon Rua Antonio Meneghetti, 226 - Sala 4 - Parque Terra Nova II, São Bernardo do Campo - SP, 09820-700, Brazil, Tel: ; Email: Opinion or female, with a round face. The best example is Nefertiti, the Bichectomy, or Bichat fat pad removal, is a surgical procedure Egyptian queen, that is still considered a beauty symbol with her indicated when there is excess volume on the middle third of the face (bellow the cheekbones / zygoma) giving it a chubby or round look. The ideal candidates are men and women who wish to achieve definedAlso and in prominentmy opinion, jaw the line. removal of Bichat fat pads do not a slimmer face appearance in this area, and it is also recommended contribute to ageing or future skin slack around the area. These are for patients with chronic cheek biting. Extra-oral photographs are the result of the normal ageing process, due to the loss of collagen part of the preoperative clinical assessment and will be compared and elastin and the shifting of fat tissues under the skin that are with photographs taken postoperative (immediately after the inevitable with age. This procedure changes the contour of the face with a decrease in bulk, resulting in less weight for the tissues to months), when the facial contour and volume reduction will be support, and, therefore, less sagging. -

A Review of the Mandibular and Maxillary Nerve Supplies and Their Clinical Relevance
AOB-2674; No. of Pages 12 a r c h i v e s o f o r a l b i o l o g y x x x ( 2 0 1 1 ) x x x – x x x Available online at www.sciencedirect.com journal homepage: http://www.elsevier.com/locate/aob Review A review of the mandibular and maxillary nerve supplies and their clinical relevance L.F. Rodella *, B. Buffoli, M. Labanca, R. Rezzani Division of Human Anatomy, Department of Biomedical Sciences and Biotechnologies, University of Brescia, V.le Europa 11, 25123 Brescia, Italy a r t i c l e i n f o a b s t r a c t Article history: Mandibular and maxillary nerve supplies are described in most anatomy textbooks. Accepted 20 September 2011 Nevertheless, several anatomical variations can be found and some of them are clinically relevant. Keywords: Several studies have described the anatomical variations of the branching pattern of the trigeminal nerve in great detail. The aim of this review is to collect data from the literature Mandibular nerve and gives a detailed description of the innervation of the mandible and maxilla. Maxillary nerve We carried out a search of studies published in PubMed up to 2011, including clinical, Anatomical variations anatomical and radiological studies. This paper gives an overview of the main anatomical variations of the maxillary and mandibular nerve supplies, describing the anatomical variations that should be considered by the clinicians to understand pathological situations better and to avoid complications associated with anaesthesia and surgical procedures. # 2011 Elsevier Ltd. -

The Syndrome of the Auriculotemporal Nerve Louis J
Louis J. KARNOSH are subject is an embolic accident due to dislodgment of a portion of a mural thrombus in the auricles. There is no evidence, however, that an accident of this kind is more likely to occur during anesthesia and operation than at other times. Summary Anesthesia and surgical operations do not increase the work load of the heart to an important degree. Patients who have organic heart dis- ease but who have been able to carry on normal daily activities without symptoms referable to the heart can be expected to tolerate anesthesia and operation without difficulty, provided that anoxia and shock are avoided. On the other hand, if there have been symptoms of a dimin- ished myocardial reserve or if congestive heart failure is present, a per- iod of preoperative treatment with rest and digitalis is advisable. The treatment should be as thorough as possible during the interval for which the operation can be safely delayed. With adequate treatment, patients who have had congestive failure can be expected to tolerate anesthesia and surgery without difficulty. Postoperative complications, however, such as pulmonary embolism, atelectasis, pneumonia, and abdominal distention, are not well borne and may be responsible for a return of decompensation. In patients who have auricular fibrillation with or without con- gestive failure, digitalis should be given before operation in sufficient amounts to reduce the ventricular rate to a satisfactory level. The drug usually should also be administered before operation to patients who have enlargement of the heart due to hypertension, even though there have been no symptoms of diminished myocardial reserve.