Student Formulary January 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Compositions Comprising Drospirenone Molecularly
(19) & (11) EP 1 748 756 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 9/00 (2006.01) A61K 9/107 (2006.01) 29.04.2009 Bulletin 2009/18 A61K 9/48 (2006.01) A61K 9/16 (2006.01) A61K 9/20 (2006.01) A61K 9/14 (2006.01) (2006.01) (2006.01) (21) Application number: 05708751.2 A61K 9/70 A61K 31/565 (22) Date of filing: 10.03.2005 (86) International application number: PCT/IB2005/000665 (87) International publication number: WO 2005/087194 (22.09.2005 Gazette 2005/38) (54) COMPOSITIONS COMPRISING DROSPIRENONE MOLECULARLY DISPERSED ZUSAMMENSETZUNGEN AUS DROSPIRENON IN MOLEKULARER DISPERSION DES COMPOSITIONS CONTENANT DROSPIRENONE A DISPERSION MOLECULAIRE (84) Designated Contracting States: (72) Inventors: AT BE BG CH CY CZ DE DK EE ES FI FR GB GR • FUNKE, Adrian HU IE IS IT LI LT LU MC NL PL PT RO SE SI SK TR D-14055 Berlin (DE) Designated Extension States: • WAGNER, Torsten AL BA HR MK YU 13127 Berlin (DE) (30) Priority: 10.03.2004 EP 04075713 (74) Representative: Wagner, Kim 10.03.2004 US 551355 P Plougmann & Vingtoft a/s Sundkrogsgade 9 (43) Date of publication of application: P.O. Box 831 07.02.2007 Bulletin 2007/06 2100 Copenhagen Ø (DK) (60) Divisional application: (56) References cited: 08011577.7 / 1 980 242 EP-A- 1 260 225 EP-A- 1 380 301 WO-A-01/52857 WO-A-20/04022065 (73) Proprietor: Bayer Schering Pharma WO-A-20/04041289 US-A- 5 569 652 Aktiengesellschaft US-A- 5 656 622 US-A- 5 789 442 13353 Berlin (DE) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Drospirenone-Containing Birth Control Pills (Yaz, Yasmin, Ocella, Gianvi and Their Generics)
Drospirenone-Containing Birth Control Pills (Yaz, Yasmin, Ocella, Gianvi and their generics) Drospirenone is a progestin component of some birth control pills that does some blocking of testosterone (the "male hormone" that women have, too, and the hormone that can be a part of making acne worse). This is why drospirenone-containing birth control pills are especially good at helping acne (and why they can theoretically help hirsutism and female-pattern scalp hair loss as well). Drospirenone is also a mild diuretic and is why these birth control pills do not cause the water weight gain that some birth control pills can. Any birth control pill can theoretically help acne just by evening out hormonal fluctuations, but for many birth control pills, the effects on acne is very minimal. Which birth control pills are most likely to help acne? Some birth control pills are more like testosterone and some are less like testosterone. The ones that are less like testosterone can theoretically help acne more. The drospirenone-containing birth control pills go one step further by blocking testosterone, and may show the most benefit on clearing acne. Drospirenone is a progestin that is derived from 17-alpha-spironolactone and is chemically related to the diuretic spironolactone. Spironolactone is a diuretic (used for high blood pressure) that is sometimes used off-label for the treatment of acne, hirsutism or female-pattern hair loss. Often people say that a drospirenone-containing birth control pill may be equivalent to 25mg of spironolactone. Risks : Any estrogen-containing birth control pill increases the risk of a high blood pressure, stroke, or other life-threatening blood clot, and one study showed possibly a slightly higher risk with a drospirenone-containing birth control pill. -

Download PDF File
Ginekologia Polska 2019, vol. 90, no. 9, 520–526 Copyright © 2019 Via Medica ORIGINAL PAPER / GYNECologY ISSN 0017–0011 DOI: 10.5603/GP.2019.0091 Anti-androgenic therapy in young patients and its impact on intensity of hirsutism, acne, menstrual pain intensity and sexuality — a preliminary study Anna Fuchs, Aleksandra Matonog, Paulina Sieradzka, Joanna Pilarska, Aleksandra Hauzer, Iwona Czech, Agnieszka Drosdzol-Cop Department of Pregnancy Pathology, Department of Woman’s Health, School of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland ABSTRACT Objectives: Using anti-androgenic contraception is one of the methods of birth control. It also has a significant, non-con- traceptive impact on women’s body. These drugs can be used in various endocrinological disorders, because of their ability to reduce the level of male hormones. The aim of our study is to establish a correlation between taking different types of anti-androgenic drugs and intensity of hirsutism, acne, menstrual pain intensity and sexuality . Material and methods: 570 women in childbearing age that had been using oral contraception for at least three months took part in our research. We examined women and asked them about quality of life, health, direct causes and effects of that treatment, intensity of acne and menstrual pain before and after. Our research group has been divided according to the type of gestagen contained in the contraceptive pill: dienogest, cyproterone, chlormadynone and drospirenone. Ad- ditionally, the control group consisted of women taking oral contraceptives without antiandrogenic component. Results: The mean age of the studied group was 23 years ± 3.23. 225 of 570 women complained of hirsutism. -

(12) STANDARD PATENT (11) Application No. AU 2015336929 B2 (19) AUSTRALIAN PATENT OFFICE
(12) STANDARD PATENT (11) Application No. AU 2015336929 B2 (19) AUSTRALIAN PATENT OFFICE (54) Title Methods of reducing mammographic breast density and/or breast cancer risk (51) International Patent Classification(s) A61K 31/568 (2006.01) A61K 31/585 (2006.01) A61K 31/4196 (2006.01) A61P 35/00 (2006.01) A61K 31/5685 (2006.01) A61P 43/00 (2006.01) (21) Application No: 2015336929 (22) Date of Filing: 2015.10.22 (87) WIPO No: W016/061615 (30) Priority Data (31) Number (32) Date (33) Country 62/067,297 2014.10.22 US (43) Publication Date: 2016.04.28 (44) Accepted Journal Date: 2021.03.18 (71) Applicant(s) Havah Therapeutics Pty Ltd (72) Inventor(s) Birrell, Stephen Nigel (74) Agent / Attorney Adams Pluck, Suite 4, Level 3 20 George Street, Hornsby, NSW, 2077, AU (56) Related Art WO 2002/009721 Al MOUSA, N.A. et al. "Aromatase inhibitors and mammographic breast density in postmenopausal women receiving hormone therapy" Menopause: The Journal of The North American Menopause Society (2008) Vol.15 No.5, pages 875 to 884 WO 2009/036566 Al SMITH, J. et al. "A Pilot Study of Letrozole for One Year in Women at Enhanced Risk of Developing Breast Cancer: Effects on Mammographic Density" Anticancer Research (2012) Vol.32 No.4, pages 1327 to 1332 OUIMET-OLIVA, D. et al. Canadian Association of Radiologists Journal (1981) Vol.32 No.3, pages 159 to 161 (see online PubMed Abstract PMID: 7298699) (12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International -

Annex D to the Report of the Panel to Be Found in Document WT/DS320/R
WORLD TRADE WT/DS320/R/Add.4 31 March 2008 ORGANIZATION (08-0902) Original: English UNITED STATES – CONTINUED SUSPENSION OF OBLIGATIONS IN THE EC – HORMONES DISPUTE Report of the Panel Addendum This addendum contains Annex D to the Report of the Panel to be found in document WT/DS320/R. The other annexes can be found in the following addenda: – Annex A: Add.1 – Annex B: Add.2 – Annex C: Add.3 – Annex E: Add.5 – Annex F: Add.6 – Annex G: Add.7 WT/DS320/R/Add.4 Page D-1 ANNEX D REPLIES OF THE SCIENTIFIC EXPERTS TO QUESTIONS POSED BY THE PANEL A. GENERAL DEFINITIONS 1. Please provide brief and basic definitions for the six hormones at issue (oestradiol-17β, progesterone, testosterone, trenbolone acetate, zeranol, and melengestrol acetate), indicating the source of the definition where applicable. Dr. Boisseau 1. Oestradiol-17β is the most active of the oestrogens hormone produced mainly by the developing follicle of the ovary in adult mammalian females but also by the adrenals and the testis. This 18-carbon steroid hormone is mainly administered as such or as benzoate ester alone (24 or 45 mg for cattle) or in combination (20 mg) with testosterone propionate (200 mg for heifers), progesterone (200 mg for heifers and steers) and trenbolone (200 mg and 40 mg oestradiol-17β for steers) by a subcutaneous implant to the base of the ear to improve body weight and feed conversion in cattle. The ear is discarded at slaughter. 2. Progesterone is a hormone produced primarily by the corpus luteum in the ovary of adult mammalian females. -

Comparing the Effects of Combined Oral Contraceptives Containing Progestins with Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis In
JMIR RESEARCH PROTOCOLS Amiri et al Review Comparing the Effects of Combined Oral Contraceptives Containing Progestins With Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis in Patients With Polycystic Ovary Syndrome: Systematic Review and Meta-Analysis Mina Amiri1,2, PhD, Postdoc; Fahimeh Ramezani Tehrani2, MD; Fatemeh Nahidi3, PhD; Ali Kabir4, MD, MPH, PhD; Fereidoun Azizi5, MD 1Students Research Committee, School of Nursing and Midwifery, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 2Reproductive Endocrinology Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 3School of Nursing and Midwifery, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 4Minimally Invasive Surgery Research Center, Iran University of Medical Sciences, Tehran, Islamic Republic Of Iran 5Endocrine Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran Corresponding Author: Fahimeh Ramezani Tehrani, MD Reproductive Endocrinology Research Center Research Institute for Endocrine Sciences Shahid Beheshti University of Medical Sciences 24 Parvaneh Yaman Street, Velenjak, PO Box 19395-4763 Tehran, 1985717413 Islamic Republic Of Iran Phone: 98 21 22432500 Email: [email protected] Abstract Background: Different products of combined oral contraceptives (COCs) can improve clinical and biochemical findings in patients with polycystic ovary syndrome (PCOS) through suppression of the hypothalamic-pituitary-gonadal (HPG) axis. Objective: This systematic review and meta-analysis aimed to compare the effects of COCs containing progestins with low androgenic and antiandrogenic activities on the HPG axis in patients with PCOS. -

Case: Management Issues
Volume 9, Issue 1 (January 2013) This clinical e-newsletter from The North American Menopause Society (NAMS) presents questions and cases commonly seen in a menopause specialist’s practice. Recognized experts in the field provide their opinions and practical advice. Wen Shen, MD, MPH, the Editor of Menopause e-Consult, encourages your suggestions for future topics. Note that the opinions expressed in the commentaries are those of the authors and are not necessarily endorsed by NAMS or Dr. Shen. Case: products were used by women in 2003.2 A patient requests your advice about Presumably, this approach to the aging US testosterone from a compounding pharmacy to female population and the increasing 3 supplement her hormone therapy. How should prevalence of low sexual desire with age you advise her? Are there any guidelines for augments demand for testosterone products for 4,5 dosing testosterone ordered from these women. As demonstrated in these reviews, pharmacies? evidence documents that testosterone treatment (local/clitoral, vaginal, and systemic) increases Management issues by: sexual desire and genital sensitivity, and might improve the intensity of orgasm. Prospective, James A. Simon, MD, CCD, randomized, clinical trials of a testosterone NCMP, FACOG patch developed specifically for women Clinical Professor, Department demonstrated a statistically significant increase of Ob/Gyn George Washington University in the number of satisfying sexual events and School of Medicine improved desire, arousal, orgasm, pleasure, Women’s Health & Research ® responsiveness, and self-image—while Consultants Washington, DC decreasing sexual concerns and distress. These findings were consistent in surgically and naturally menopausal women already on The controversy over compounding rages on. -

Drugs Contraindicated in Pregnancy
DRUGS CONTRAINDICATED IN PREGNANCY (Part 1 of 2) This chart represents information on select drugs that are contraindicated (Pregnancy category X) for women who are pregnant. This is not an inclusive list of products that carry that pregnancy category. Those drugs that are contraindicated at a certain phase of the pregnancy are listed next to the product name. For more information on specific drug monographs, see product entries or consult the manufacturer. ALLERGIC DISORDERS Tazorac (tazarotene) METABOLIC DISORDERS Tilia Fe (norethindrone acetate/ethinyl Vistaril (hydroxyzine) Early pregnancy estradiol) Zavesca (miglustat) CARDIOVASCULAR SYSTEM Tri-Legest Fe (norethindrone acetate/ MUSCULOSKELETAL DISORDERS ethinyl estradiol) Advicor (niacin ext-rel/lovastatin) Tri-previfem (norgestimate/ethinyl Advil (ibuprofen) 3rd trimester Aggrenox (dipyridamole/aspirin) 3rd estradiol) Aleve (naproxen sodium) 3rd trimester trimester Tri-sprintec (norgestimate/ethinyl estradiol) Ansaid (flurbiprofen) Late pregnancy Altoprev (lovastatin) Yaz (drospirenone/ethinyl estradiol) Arava (leflunomide) Bayer (aspirin) 3rd trimester Arthrotec (diclofenac sodium/ Caduet (amlodipine/atorvastatin) ENDOCRINE SYSTEM misoprostol) Coumadin (warfarin sodium) 3rd trimester Androderm (testosterone) Bayer (aspirin) Crestor (rosuvastatin) Androgel (testosterone) BC Arthritis Strength (aspirin/ Ecotrin (aspirin) 3rd trimester 3rd trimester Android (methyltestosterone) caffeine/salicylamide) Lescol (fluvastatin) 3rd Axiron (testosterone) Carisoprodol/aspirin/codeine Lescol -

Safety and Efficacy of Testosterone for Women: a Systematic Review and Meta-Analysis of Randomised Controlled Trial Data
Articles Safety and efficacy of testosterone for women: a systematic review and meta-analysis of randomised controlled trial data Rakibul M Islam, Robin J Bell, Sally Green, Matthew J Page, Susan R Davis Summary Background The benefits and risks of testosterone treatment for women with diminished sexual wellbeing remain Lancet Diabetes Endocrinol 2019 controversial. We did a systematic review and meta-analysis to assess potential benefits and risks of testosterone for Published Online women. July 25, 2019 http://dx.doi.org/10.1016/ S2213-8587(19)30189-5 Methods We searched MEDLINE, Embase, the Cochrane Central Register of Controlled Trials, and Web of Science for See Online/Comment blinded, randomised controlled trials of testosterone treatment of at least 12 weeks’ duration completed between http://dx.doi.org/10.1016/ Jan 1, 1990, and Dec 10, 2018. We also searched drug registration applications to the European Medicine Agency and S2213-8587(19)30251-7 the US Food and Drug Administration to identify any unpublished data. Primary outcomes were the effects of Women’s Health Research testosterone on sexual function, cardiometabolic variables, cognitive measures, and musculoskeletal health. This Program (R M Islam PhD, study is registered with the International Prospective Register of Systematic Reviews (PROSPERO), number Prof R J Bell MBBS, Prof S R Davis MBBS), School CRD42018104073. of Public Health and Preventive Medicine, Monash University, Findings Our search strategy retrieved 46 reports of 36 randomised controlled trials comprising -

Use of Postmenopausal Hormone Therapy and Risk of Alzheimer’S BMJ: First Published As 10.1136/Bmj.L665 on 6 March 2019
RESEARCH Use of postmenopausal hormone therapy and risk of Alzheimer’s BMJ: first published as 10.1136/bmj.l665 on 6 March 2019. Downloaded from disease in Finland: nationwide case-control study Hanna Savolainen-Peltonen,1,2 Päivi Rahkola-Soisalo,1 Fabian Hoti,3 Pia Vattulainen,3 Mika Gissler,4,5,6 Olavi Ylikorkala,1 Tomi S Mikkola1,2 1University of Helsinki and ABSTRACT ratio 1.09, 95% confidence interval 1.05 to 1.14) and Helsinki University Hospital, OBJECTIVES those of oestrogen-progestogen (1.17, 1.13 to 1.21). Obstetrics and Gynecology, To compare the use of hormone therapy between The risk increases in users of oestrogen-progestogen Haartmaninkatu 2, PO Box 140, FIN-00029 HUS, 00029 Finnish postmenopausal women with and without a therapy were not related to different progestogens Helsinki, Finland diagnosis for Alzheimer’s disease. (noreth isterone acetate, medroxyprogesterone 2 Folkhälsan Research Center, DESIGN acetate, or other progestogens); but in women Biomedicum, Helsinki, Finland younger than 60 at hormone therapy initiation, 3 Nationwide case-control study. EPID Research Oy, Espoo, these risk increases were associated with hormone Finland SETTING therapy exposure over 10 years. Furthermore, the 4National Institute for Health Finnish national population and drug register, age at initiation of systemic hormone therapy was and Welfare, Helsinki, Finland between 1999 and 2013. 5Karolinska Institute, not a decisive determinant for the increase in risk Department of Neurobiology, PARTICIPANTS of Alzheimer’s disease. The exclusive use of vaginal Care Sciences and Society, All postmenopausal women (n=84 739) in Finland estradiol did not affect the risk of the disease (0.99, Division of Family Medicine, who, between 1999 and 2013, received a diagnosis of 0.96 to 1.01). -
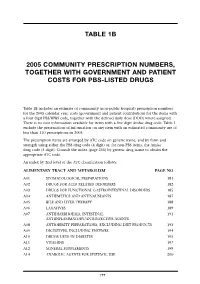
Table 1B 2005 Community Prescription Numbers, Together with Government
TABLE 1B 2005 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS-LISTED DRUGS Table 1B includes an estimate of community (non-public hospital) prescription numbers for the 2005 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 exclude the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2005. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit) or, for non-PBS items, the Amfac drug code (5 digit). Consult the index (page 255) by generic drug name to obtain the appropriate ATC code. An index by 2nd level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM PAGE NO A01 STOMATOLOGICAL PREPARATIONS 181 A02 DRUGS FOR ACID RELATED DISORDERS 182 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 185 A04 ANTIEMETICS AND ANTINAUSEANTS 187 A05 BILE AND LIVER THERAPY 188 A06 LAXATIVES 189 A07 ANTIDIARRHOEALS, INTESTINAL 191 ANTIINFLAMMATORY/ANTIINFECTIVE AGENTS A08 ANTIOBESITY PREPARATIONS, EXCLUDING DIET PRODUCTS 193 A09 DIGESTIVES, INCLUDING ENZYMES 194 A10 DRUGS USED IN DIABETES 195 A11 VITAMINS 197 A12 MINERAL SUPPLEMENTS 199 A14 ANABOLIC AGENTS FOR SYSTEMIC USE 200 177 BLOOD AND BLOOD FORMING ORGANS B01 ANTITHROMBOTIC AGENTS 201 B02 ANTIHAEMORRHAGICS 203 B03 -

The Influence of Hormone Therapy with Drospirenone-Estradiol on Endometrioid Type Endometrial Cancer Patients
J Gynecol Oncol. 2018 Sep;29(5):e72 https://doi.org/10.3802/jgo.2018.29.e72 pISSN 2005-0380·eISSN 2005-0399 Original Article The influence of hormone therapy with drospirenone-estradiol on endometrioid type endometrial cancer patients Soyi Lim ,1,* Yun Hwan Kim ,2,* Kwang-Beom Lee ,1 Jong-Min Lee 3 1Department of Obstetrics and Gynecology, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea 2Department of Obstetrics and Gynecology, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea 3Department of Obstetrics and Gynecology, Kyung-Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea Received: Oct 30, 2017 ABSTRACT Revised: Apr 17, 2018 Accepted: Apr 22, 2018 Objective: To determine whether drospirenone/estradiol (DRSP/E2) has an adverse effect on Correspondence to clinical outcomes in surgically staged International Federation of Gynecology and Obstetrics Kwang-Beom Lee (FIGO) stage I/II endometrial cancer (EC) patients. Department of Obstetrics and Gynecology, Methods: In a retrospective case-controlled study, 58 women with EC who had received Gachon University Gil Medical Center, DRSP/E2 postoperatively were compared with 116 women who had not. And, oncologic safety Gachon University College of Medicine, 21 Namdong-daero 774-beon-gil, Namdong-gu, of postoperative hormone therapy with DRSP/E2 in EC survivors were compared between the Incheon 21565, Korea. 2 groups after propensity score matching using a logistic regression model. E-mail: [email protected] Results: The median ages were 47.7 years and 53.6 years for the study and the control groups, respectively (p<0.001).