Hepatocellular Carcinoma Masquerading As a Large Renal Mass with Hepatic Invasion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primary Renal Carcinoid Tumor: a Radiologic Review
Radiology Case Reports Volume 9, Issue 2, 2014 Primary renal carcinoid tumor: A radiologic review Leslie Lamb, MD, Msc, Bsc; Wael Shaban, MBBCH, MD, PhD Carcinoid tumor is the classic famous anonym of neuroendocrine neoplasms. Primary renal carcinoid tumors are extremely rare, first described by Resnick and colleagues in 1966, with fewer than a total of 100 cases reported in the literature. Thus, given the paucity of cases, the clinical and histological behav- ior is not well understood, impairing the ability to predict prognosis. Computed tomography and (occa- sionally) octreotide studies are used in the diagnosis and followup of these rare entites. A review of 85 cases in the literature shows that no distinctive imaging features differentiate them from other primary renal masses. The lesions tend to demonstrate a hypodense appearance and do not usually enhance in the arterial phases, but can occasionally calcify. Octreotide scans do not seem to help in the diagnosis; however, they are more commonly used in the postoperative followup. In addition, we report a new case of primary renal carcinoid in a horseshoe kidney. Case report Imaging findings 40-year-old male initially presented to a community hos- pital with a 20-lb weight loss over a few months. In retro- CT of the abdomen and pelvis, done in the portal ve- spect, the patient recalled mild left-flank discomfort and nous phase, demonstrated a solid, hypodense, 4.5-cm renal fatigue, but denied any hematuria. Blood work revealed an mass containing calcifications, located in the posterior as- elevated serum glucose, and he was diagnosed with type 2 pect of the medial diabetes. -

Solitary Duodenal Metastasis from Renal Cell Carcinoma with Metachronous Pancreatic Neuroendocrine Tumor: Review of Literature with a Case Discussion
Published online: 2021-05-24 Practitioner Section Solitary Duodenal Metastasis from Renal Cell Carcinoma with Metachronous Pancreatic Neuroendocrine Tumor: Review of Literature with a Case Discussion Abstract Saphalta Baghmar, Renal cell cancinoma (RCC) is a unique malignancy with features of late recurrences, metastasis S M Shasthry1, to any organ, and frequent association with second malignancy. It most commonly metastasizes Rajesh Singla, to the lungs, bones, liver, renal fossa, and brain although metastases can occur anywhere. RCC 2 metastatic to the duodenum is especially rare, with only few cases reported in the literature. Herein, Yashwant Patidar , 3 we review literature of all the reported cases of solitary duodenal metastasis from RCC and cases Chhagan B Bihari , of neuroendocrine tumor (NET) as synchronous/metachronous malignancy with RCC. Along with S K Sarin1 this, we have described a unique case of an 84‑year‑old man who had recurrence of RCC as solitary Departments of Medical duodenal metastasis after 37 years of radical nephrectomy and metachronous pancreatic NET. Oncology, 1Hepatology, 2Radiology and 3Pathology, Keywords: Late recurrence, pancreatic neuroendocrine tumor, renal cell carcinoma, second Institute of Liver and Biliary malignancy, solitary duodenal metastasis Sciences, New Delhi, India Introduction Case Presentation Renal cell carcinoma (RCC) is unique An 84‑year‑old man with a medical history to have many unusual features such as notable for hypertension and RCC, 37 years metastasis to almost every organ in the body, postright radical nephrectomy status, late recurrences, and frequent association presented to his primary care physician with second malignancy. The most common with fatigue. When found to be anemic, sites of metastasis are the lung, lymph he was treated with iron supplementation nodes, liver, bone, adrenal glands, kidney, and blood transfusions. -
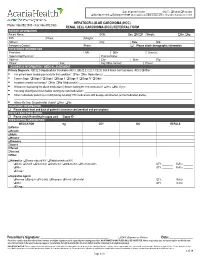
HCC/RCC Referral Form
Date Shipment Needed: Ship To: Patient Prescriber Nursing needed; Training needed ►All the supplies including syringes and needles will be dispensed if needed. HEPATOCELLULAR CARCINOMA (HCC) Phone: 866.892.1580 • Fax: 866.892.2363 RENAL CELL CARCINOMA (RCC) REFERRAL FORM PATIENT INFORMATION Patient Name: DOB: Sex: M F Weight: lbs. kg. SSN: Phone: Allergies: Address: City: State: Zip: Emergency Contact: Phone: Please attach demographic information PRESCRIBER INFORMATION Prescriber: NPI: DEA: State Lic: Supervising Physician: Practice Name: Address: City: State: Zip: Phone: Fax: Key Office Contact: Phone: DIAGNOSIS INFORMATION / MEDICAL ASSESMENT Primary Diagnosis: C22.0 Hepatocellular Carcinoma (HCC) C22.2; C22.7; C22.8; C64.9 Renal Cell Carcinoma (RCC) Other________________________________ . Has patient been treated previously for this condition? Yes No Medication(s): __________________________________________________________________ . Cancer Stage: Stage 0 Stage I Stage II Stage III Stage IV Other: ______________________________________________________________________ . Is patient currently on therapy? Yes No Medication(s): ____________________________________________________________________________________ . Will patient stop taking the above medication(s) before starting the new medication? Yes No If yes: _________________________________________________ . How long should patient wait before starting the new medication? ________________________________________________________________________________ . Other medications patient is -

ASC Webinar: Practical Approach to Liver Cytology Indication
ASC Webinar: Practical Approach to Liver Cytology Barbara A. Centeno, M.D. Director of AP Quality Assurance Director of Cytopathology and Senior member/Moffitt Cancer Center Professor/Departments of Oncologic Sciences Morsani College of Medicine University of South Florida 1 LIVER OUTLINE • Background • Cytology of benign liver and liver nodules • Cytology of Primary Liver Cancers – Hepatocellular carcinoma – Cholangiocarcinoma • Ancillary studies for key differential diagnoses • Metastases 2 Indication: Evaluation of a Mass • Nonneoplastic lesions – hemangioma • Benign liver nodule –FNH – Adenoma • Primary epithelial cancers – HCC –ICC • Less common nonepithelial neoplasms and malignancies • Metastases 3 KEY DIAGNOSTIC ISSUES • Distinction of benign or reactive hepatocytes in nonneoplastic or benign liver nodules from well- differentiated hepatocellular carcinoma • Distinction of poorly differentiated hepatocellular carcinoma from cholangiocarcinoma or metastases • Determination of primary site of origin of metastases • Determination of histogenesis of poorly differentiated malignancie 4 APPROACH TO THE DIAGNOSIS OF LIVER LESIONS • Clinical history – Age and gender • Hepatoblastoma in infants • Adenoma in females – Underlying liver disease • HCV and Cirrhosis as a predisposing risk factor for HCC – Previous history of carcinoma • Radiological imaging – Borders, possible vascular lesion • Cytological findings • Ancillary studies • Correlate all findings 5 Hepatocytes • Monolayered sheets,thin trabeculae, single cells or small, loose groups -

Kidney Cancer Early Detection, Diagnosis, and Staging Detection and Diagnosis
cancer.org | 1.800.227.2345 Kidney Cancer Early Detection, Diagnosis, and Staging Detection and Diagnosis Catching cancer early often allows for more treatment options. Some early cancers may have signs and symptoms that can be noticed, but that is not always the case. ● Can Kidney Cancer Be Found Early? ● Kidney Cancer Signs and Symptoms ● Tests for Kidney Cancer Stages and Outlook (Prognosis) After a cancer diagnosis, staging provides important information about the extent of cancer in the body and anticipated response to treatment. ● Kidney Cancer Stages ● Survival Rates for Kidney Cancer Questions to Ask About Kidney Cancer Here are some questions you can ask your cancer care team to help you better understand your cancer diagnosis and treatment options. ● Questions to Ask About Kidney Cancer 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Can Kidney Cancer Be Found Early? Many kidney cancers are found fairly early, while they are still limited to the kidney, but others are found at a more advanced stage. There are a few reasons for this: ● These cancers can sometimes grow quite large without causing any pain or other problems. ● Because the kidneys are deep inside the body, small kidney tumors cannot be seen or felt during a physical exam. ● There are no recommended screening tests for kidney cancer in people who are not at increased risk. This is because no test has been shown to lower the overall risk of dying from kidney cancer. For people at average risk of kidney cancer Some tests can find some kidney cancers early, but none of these is recommended to screen for kidney cancer in people at average risk. -

Paraneoplastic Encephalitis Associated with Renal Cell Carcinoma
Original Article pISSN 2765-4559 eISSN 2734-1461 encephalitis |Vol. 1, No. 3| May 28, 2021 https://doi.org/10.47936/encephalitis.2021.00059 Paraneoplastic encephalitis associated with renal cell carcinoma Yoonhyuk Jang, SeonDeuk Kim, Kon Chu, Sang Kun Lee, Soon-Tae Lee Department of Neurology, Seoul National University Hospital, Seoul, Korea Purpose Paraneoplastic encephalitis is autoimmune encephalitis accompanied by tumors. Renal cell carcinoma (RCC) is a kidney cancer originating from various types of renal cells and rarely has been associated with paraneoplastic neurologic manifestation. We identified a case series of parane- oplastic encephalitis-associated RCC. Methods From a prospective institutional cohort, we identified autoimmune encephalitis patients with RCC. The association between RCC and encephali- tis was determined by the following criteria: (1) possible autoimmune encephalitis according to the operational autoimmune encephalitis diag- nostic criteria and (2) RCC simultaneously diagnosed with neurological manifestation of encephalitis. Results A total of three patients presented encephalitis accompanied by RCC. Two patients had clear cell RCC, and one had chromophobe RCC. All pa- tients showed limbic encephalitis with cognitive decline, memory impairment, or seizure. Brain magnetic resonance imaging showed T2 hyperin- tensities at the mesial temporal lobe in two patients with clear cell RCC but no remarkable findings in one patient with chromophobe RCC. While one patient who had early surgery within one month of RCC onset had a favorable response to the treatment, the other two patients showed a partial response and a detrimental result. Conclusion Paraneoplastic encephalitis associated with RCC presented as limbic encephalitis and was responsive to immunotherapy combined with tumor resection. -

Case Report Concurrent Primary Carcinoid Tumor Arising Within
Int J Clin Exp Pathol 2013;6(11):2578-2584 www.ijcep.com /ISSN:1936-2625/IJCEP1308045 Case Report Concurrent primary carcinoid tumor arising within mature teratoma and clear cell renal cell carcinoma in the horseshoe kidney: report of a rare case and review of the literature Ke Sun1, Qihan You1, Ming Zhao2, Hongtian Yao1, Hua Xiang1, Lijun Wang1 1Department of Pathology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zheji- ang 310003, China; 2Department of Pathology, Ningbo Yinzhou Second Hospital, Ningbo, Zhejiang 315100, China Received August 16, 2013; Accepted September 20, 2013; Epub October 15, 2013; Published November 1, 2013 Abstract: Primary carcinoid tumor arising in a mature teratoma of the horseshoe kidney is exceptionally rare and only 4 such cases have been reported in the world literature to date. The simultaneous occurrence of different sub- types of renal cell carcinoma (RCC) or RCC coexistence with non-RCC neoplasms from the same kidney is unusual and infrequently reported. Herein we report a case of primary carcinoid tumor arising within mature teratoma, con- current with a clear cell RCC in the horseshoe kidney of a 37-year-old man. Histologically, both the carcinoid tumor and clear cell RCC demonstrated the characteristic morphology in their classic forms. In addition to the carcinoid tumor, the mature teratoma consisted of variably sized, large cystic spaces lined by cytologically bland mucinous columnar epithelium, pseudostratified columnar epithelium, ciliated epithelium and mature smooth muscle fibers were also identified within the cystic wall. Furthermore, foci of round, small nodules composed of mature prostatic acinus were noted in the teratoma which was confirmed by exhibiting strong immunoreactivity for prostate specific antigen. -

Thymic Carcinomas and Second Malignancies: a Single-Center Review
cancers Communication Thymic Carcinomas and Second Malignancies: A Single-Center Review Sunil S. Badve 1,* , Rachel Dougherty 1, Michael Balatico 1, Kenneth A. Kesler 2, Patrick Loehrer 3 and Yesim Gökmen-Polar 1 1 Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, Indianapolis, IN 46202, USA; [email protected] (R.D.); [email protected] (M.B.); [email protected] (Y.G.-P.) 2 Department of Surgery and Internal Medicine, Indiana University School of Medicine, Indianapolis, IN 46202, USA; [email protected] 3 Department of Internal Medicine, Indiana University School of Medicine, Indianapolis, IN 46202, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-317-278-9335 Simple Summary: Thymic carcinoma (TC) is a rare neoplasm that accounts for less than 0.01% of all tumors. The aim of our retrospective observational analysis is to review the incidence of second cancers associated with this histological type of cancer. We identified 92 patients with TC referred to our consultation practice and reviewed their clinical data for diagnosis of another cancer pre- or post-diagnosis of TC. This resulted in identification of 14 patients with additional cancers. The incidence of second cancer is similar to that observed in thymomas. Abstract: Thymic carcinomas account for less than 0.01% of new cancer diagnoses annually and are more aggressive than thymomas. Autoimmune disorders have been associated with thymomas Citation: Badve, S.S.; Dougherty, R.; and only recently with thymic carcinomas. Second malignancies are well described after thymomas. Balatico, M.; Kesler, K.A.; Loehrer, P.; The aim of this study was to analyze the incidence of second malignancies in patients with thymic Gökmen-Polar, Y. -

Diagnostic Utility of S100A1 Expression in Renal Cell Neoplasms: an Immunohistochemical and Quantitative RT-PCR Study
Modern Pathology (2007) 20, 722–728 & 2007 USCAP, Inc All rights reserved 0893-3952/07 $30.00 www.modernpathology.org Diagnostic utility of S100A1 expression in renal cell neoplasms: an immunohistochemical and quantitative RT-PCR study Paolo Cossu Rocca1, Matteo Brunelli2, Stefano Gobbo2, Albino Eccher2, Emma Bragantini2, Maria M Mina2, Vincenzo Ficarra3, Filiberto Zattoni4, Alberto Zamo` 2, Maurizio Pea2, Aldo Scarpa2, Marco Chilosi2, Fabio Menestrina2, Franco Bonetti2, John N Eble5 and Guido Martignoni2 1Department of Pathology, University of Sassari, Sassari, Italy; 2Department of Pathology, University of Verona, Verona, Italy; 3Department of Urology and Surgical Sciences, Urology Clinic, University of Padova, Padova, Italy; 4Department of Urology, University of Verona, Verona, Italy and 5Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, Indianapolis, IN, USA S100A1 is a calcium-binding protein, which has been recently found in renal cell neoplasms. We evaluated the diagnostic utility of immunohistochemical detection of S100A1 in 164 renal cell neoplasms. Forty-one clear cell, 32 papillary, and 51 chromophobe renal cell carcinomas, and 40 oncocytomas, 164 samples of normal renal parenchyma adjacent to the tumors and 13 fetal kidneys were analyzed. The levels of S100A1 mRNA detected by quantitative RT-PCR analysis of frozen tissues from seven clear cell, five papillary, and six chromophobe renal cell carcinomas, four oncocytomas, and nine samples of normal renal tissues adjacent to neoplasms were compared with the immunohistochemical detection of protein expression. Clear cell and papillary renal cell carcinomas showed positive reactions for S100A1 in 30 out of 41 tumors (73%) and in 30 out of 32 (94%) tumors, respectively. -

Chapter 14: Hereditary Renal Cancer Syndromes
Chapter 14: Hereditary Renal Cancer Syndromes Katherine L. Nathanson, MD Department of Medicine, Division of Translational Medicine and Human Genetics, and Cancer Control Program, Abramson Cancer Center, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania INTRODUCTION a wide spectrum of hemangioblastomas of the brain, spine, and retina, pancreatic cysts and neuroendo- Inherited forms of renal cancer are estimated to ac- crine tumors, renal cysts and clear cell renal tumors, count for 2%–5% of all kidney cancer (1). Currently, endolympatic sac tumors, and pheochromocyto- 10 inherited cancer susceptibility syndromes are de- mas. vHL disease is found across all ethnic groups, finitively associated with an increased risk of renal with approximatelyone-quarterof the incidence due cancer (Table 1) and are described in more detail be- to de novo mutations; genetic testing for mutations low. Patients with these inherited syndromes develop in VHL detects nearly 100% of individuals with vHL kidney cancer at an earlier age; furthermore, the le- disease (6). Disease usually presents in the late teens sions can be multifocal, bilateral, and heterogeneous. to early 20s, although an occasional individual may Several, including Birt-Hogg-Dubé syndrome be diagnosed in their mid-40s. The presentation of (BHD), familial clear cell renal cancer due to chromo- renal disease is quite variable even within family some 3 translocation, hereditary papillary renal cancer, members, with some patients never developing renal hereditary leiomyomatosis and renal cell cancer cancer, others having a few renal cysts, and others (HLRCC), and von Hippel-Lindau disease (vHL) with who have bilateral renal cancers and hundreds have renal cancer as a primary feature, whereas in an- of lesions within each kidney. -

Metastasis of Rectal Adenocarcinoma to the Pancreas. Two Case Reports and a Review of the Literature
JOP. J Pancreas (Online) 2007; 8(2):214-222. CASE REPORT Metastasis of Rectal Adenocarcinoma to the Pancreas. Two Case Reports and a Review of the Literature Jeannine Bachmann1, Christoph W Michalski1, Frank Bergmann2, Markus W Büchler1, Jörg Kleeff1, Helmut Friess1 Departments of 1General Surgery and 2Pathology. University of Heidelberg. Heidelberg, Germany ABSTRACT CASE PRESENTATIONS Context The vast majority of pancreatic Two patients were referred for explorative tumors are of pancreatic origin. Nonetheless, laparotomy and resection of the tumors in the a variety of extrapancreatic tumors can pancreas. involve the pancreas and may manifest with different clinicopathological characteristics. Case 1 Case report We report on two patients with a history of rectal cancer who were referred to A 61-year-old woman in good general our department with a pancreatic mass: one condition presented to our department patient 2 years after a low anterior resection complaining of abdominal pain in the left (TNM stage: pT3 pN0 pM0), the other patient upper quadrant. She had had the pain for at 2.5 years after an abdominoperineal resection least one year. Past medical history revealed (TNM stage: pT3 pN1 pM0). In the first case, that a low anterior resection for a poorly computed tomography showed a cystic mass differentiated (G3) rectal adenocarcinoma had in the pancreas but fine-needle biopsy been performed 2 years before presentation followed by cytopathological analysis (TNM stage: pT3 pN0 pM0); neoadjuvant revealed only necrotic tissue. In the other radiation therapy had been administered patient, magnetic resonance tomography before that surgery and no adjuvant treatment showed a hypodense structure in the had been given. -

Kidney Solid Tumor Rules
Kidney Equivalent Terms and Definitions C649 (Excludes lymphoma and leukemia M9590 – M9992 and Kaposi sarcoma M9140) Introduction Note 1: Tables and rules refer to ICD-O rather than ICD-O-3. The version is not specified to allow for updates. Use the currently approved version of ICD-O. Note 2: 2007 MPH Rules and 2018 Solid Tumor Rules are used based on date of diagnosis. • Tumors diagnosed 01/01/2007 through 12/31/2017: Use 2007 MPH Rules • Tumors diagnosed 01/01/2018 and later: Use 2018 Solid Tumor Rules • The original tumor diagnosed before 1/1/2018 and a subsequent tumor diagnosed 1/1/2018 or later in the same primary site: Use the 2018 Solid Tumor Rules. Note 3: Renal cell carcinoma (RCC) 8312 is a group term for glandular (adeno) carcinoma of the kidney. Approximately 85% of all malignancies of the kidney C649 are RCC or subtypes/variants of RCC. • See Table 1 for renal cell carcinoma subtypes/variants. • Clear cell renal cell carcinoma (ccRCC) 8310 is the most common subtype/variant of RCC. Note 4: Transitional cell carcinoma rarely arises in the kidney C649. Transitional cell carcinoma of the upper urinary system usually arises in the renal pelvis C659. Only code a transitional cell carcinoma for kidney in the rare instance when pathology confirms the tumor originated in the kidney. Note 5: For those sites/histologies which have recognized biomarkers, the biomarkers are most frequently used to target treatment. Biomarkers may identify the histologic type. Currently, there are clinical trials being conducted to determine whether these biomarkers can be used to identify multiple primaries.