Psychological Response of Healthcare Workers and Stigma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

University of Kerala
UNIVERSITY OF KERALA RESULTS OF EIGHTH SEMESTER B.TECH DEGREE EXAMINATION (2008 SCHEME) APRIL 2016 Log in to our website www.keralauniveristy.ac.in Not to be published before 20.07.2016 UNIVERSITY OF KERALA Thiruvananthapuram, Kerala, India – 695034 (Re-accredited by NAAC with ‘A’ Grade) (Established as University of Travancore by the Travancore University Act in 1937 and reconstituted as University of Kerala by the Kerala University Act of 1957 and presently governed by the Kerala University Act of 1974 passed by the Kerala State Legislative Assembly) NOTIFICATION The following is the provisional list of successful candidates at the Eighth Semester B. Tech. Degree Examination (2008 Scheme) held in April 2016. The mark list of the candidates will be sent to the respective centers of examination by 10.08.2016. The mark list of those candidates in respect of whom there are defects to be rectified will not be issued although their results have been provisionally published. Candidates who are applying for revaluation/Scrutiny should submit application only through online on or before 10.08.2016. Candidates can make use of the draft mark list available in the website for applying for revaluation. The results are available on the University Website. Sd/- CONTROLLER OF EXAMINATIONS To 1. The PRO for issuing urgent press release 2. PS to VC, PS to PVC, PA to Registrar, PA to CE 3. The Reception Officer 4. The Engineering Tabulation Sections-Section Officers should ensure that the mark lists are dispatched in time to the examination centers. 5. The Principals of all Engineering Colleges 6. -

IT/KGB/TENDER/3/98/2018 Date: 16-03-2018
Ref: IT/KGB/TENDER/3/98/2018 Date: 16-03-2018 TENDER FOR AMC OF COMPUTER HARDWARE ITEMS We invite sealed tenders on item rate basis from interested vendors for Annual Maintenance Contract of Computer Hardware Items installed at various branches/offices of our Bank in Trivandrum, Kollam, Pathanmthitta, Alappuzha, Kottayam, Idukki, Eranakulam, Thrissur, Palakkad, Malappuram, Wayanadu districts and part of Kozhikode district. List of branches and Hardware items are mentioned in Annexure D. The number of hardware items may be increased or decreased at the time of contract or even during the period of AMC which may be included or excluded from the list and the location of the equipments may also be changed. The AMC vendor shall include these items under the AMC on being informed by the Bank. Eligibility of vendor for Tender: The Vendor must have at least TWO direct offices in the mentioned geographical area (one office anywhere in TVM, KTM or EKM districts and another one anywhere in TSR, MPM or KZD districts) for fast and effective service support. Address proof of service support office or branch office should be produced such as PAN, Tax receipt, Certificate of registration like Shop & Establishment, Service Tax/Sales Tax/VAT/LBT/etc. The vendor must inform the full address and name of the office-in-charge. The vendor must have at least two qualified Service support engineers at each office above. The vendor must have an average annual turnover of Rs. 10 crore (As per last three years’ Audited Annual Financial Statement/Income tax returns - to be enclosed). -

Bhavana Samunnathi - Beneficiary List
Kerala State Welfare Corporation for Forward Communities [SAMUNNATHI] Bhavana Samunnathi - Beneficiary List Application Sl. No Name of Beneficiary Address No SARANYA HOUSE, MEKKEPLAVILA, CHENGAL, 1289 SREEKUMARI .S 1 MARIYAPURAM, TRIVANDRUM -695122 MUDIKONATHU VEEDU, THOTTAYKAD.P.O, 2 2982 SUDHARSANAN KALLAMBALAM, KARAVARAM, CHIRAYINKEEZHU, TRIVANDRUM-695605 KATTAKKALARIKATHU PUTHENVEEDU, 3 388 SANTHA A AUMKUZHI,CHERUPPANI, VINOBHA NIKETHAN P O,TRIVANDRUM-695542 MEKKETHERIYIL VEEDU, CHAYIKULAM, 4 1354 SINDHU S.S VEEERANAKAVU P.O, KATTAKADA, TRIVANDRUM -695572 KATTOOR THODIYIL VEEDU, KALLAMBALAM 5 2158 VIJAYA KUMARI P.O, KARAVARAM , CHIRAYINKEEZHU, TRIVANDRUM -695605 KAITHAKUZHI VEEDU, VETTINADU, 6 3410 SARASWATHY AMMA K VATTAPPARAP.O, VEMBAYAM, NEDUMANGAD, TRIVANDRUM -695028 DHANYA BHAVAN, CHAYAM, VITHURA P.O, 7 4131 VIJAYAKUMARI S THOLICODE, NEDUMANGAD, TRIVANDRUM - 695551 MAVILAM KUZHI, KULATHAMAL, 8 4553 GEETHAKUMARI J CHAYKOTTUKONAM.P.O, NEYYATTINKARA, TRIVANDRUM-695122 THIRUVONAM, PERUMBALOOR,ANCODE, 9 5958 R. LEELA PERUMKADAVILA P.O, NEYYATTINKARA, TRIVANDRUM -695124 MANDAPAVILA VEEDU, ANAD.P.O, 7276 ANITHA S 10 NEDUMANGAD, TRIVANDRUM-695541 MUNNAMATHU VEEDU, KEEZHKOLLA, 11 7376 SUKUMARI AMMA VATTAVILA.P.O, CHENKAL, NEYYATTINKARA, TRIVANDRUM-695132 VATTAKARIKKAKATHIL VEEDU, 12 8231 INDIRADEVI K SASTHAMKAVU, VITHURA.P.O, THOLIKODE, NDUMANGAD , TRIVANDRUM-695551 IRAYAMKODU, THADATHARIKATHU VEEDU, 13 10949 SUBHADRA VITHURA.P.O, THOLIKKODE, NEDUMANGAD, TRIVANDRUM-695551 ITTIYARA VEEDU, PLAMOOTTUKADA.P.O, 14 11736 K VIJAYALEKSHMI KARODE, -
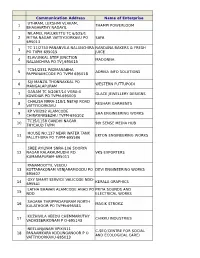
Communication Address Name of Enterprise 1 THAMPI
Communication Address Name of Enterprise UTHRAM, LEKSHMI VLAKAM, 1 THAMPI POWERLOOM BHAGAVATHY NADAYIL NILAMEL NALUKETTU TC 6/525/1 2 MITRA NAGAR VATTIYOORKAVU PO SAFA 695013 TC 11/2750 PANANVILA NALANCHIRA NANDANA BAKERS & FRESH 3 PO TVPM 695015 JUICE ELAVUNKAL STEP JUNCTION 4 MADONNA NALANCHIRA PO TV[,695015 TC54/2331 PADMANABHA 5 ADRIKA INFO SOLUTIONS PAPPANAMCODE PO TVPM 695018 SIJI MANZIL THONNAKKAL PO 6 WESTERN PUTTUPODI MANGALAPURAM GANAM TC 5/2067/14 VGRA-4 7 GLACE JEWELLERY DESIGNS KOWDIAR PO TVPM-695003 CHALISA NRRA-118/1 NETAJI ROAD 8 RESHAM GARMENTS VATTIYOORKAVU KP VIII/292 ALAMCODE 9 SHA ENGINEERING WORKS CHIRAYINKEEZHU TVPM-695102 TC15/1158 GANDHI NAGAR 10 9th SENSE MEDIA HUB THYCAUD TVPM HOUSE NO.137 NEAR WATER TANK 11 EKTON ENGINEERING WORKS PALLITHURA PO TVPM-695586 SREE AYILYAM SNRA-106 SOORYA 12 NAGAR KALAKAUMUDHI RD. VKS EXPORTERS KUMARAPURAM-695011 PANAMOOTTIL VEEDU 13 KOTTARAKONAM VENJARAMOODU PO DEVI ENGINEERING WORKS 695607 OXY SMART SERVICE VALICODE NDD- 14 KERALA GRAPHICS 695541 LATHA BHAVAN ALAMCODE ANAD PO PRIYA SOUNDS AND 15 NDD ELECTRICAL WORKS SAGARA THRIPPADAPURAM NORTH 16 MAGIK STROKZ KULATHOOR PO TVPM-695583 KUZHIVILA VEEDU CHEMMARUTHY 17 CHIKKU INDUSTRIES VADASSERIKONAM P O-695143 NEELANJANAM VPIX/511 C-SEC(CENTRE FOR SOCIAL 18 PANAAMKARA KODUNGANOOR P O AND ECOLOGICAL CARE) VATTIYOORKAVU-695013 ZENITH COTTAGE CHATHANPARA GURUPRASADAM READYMADE 19 THOTTAKKADU PO PIN695605 GARMENTS KARTHIKA VP 9/669 20 KODUNGANOORPO KULASEKHARAM GEETHAM 695013 SHAMLA MANZIL ARUKIL, 21 KUNNUMPURAM KUTTICHAL PO- N A R FLOUR MILLS 695574 RENVIL APARTMENTS TC1/1517 22 NAVARANGAM LANE MEDICAL VIJU ENTERPRISE COLLEGE PO NIKUNJAM, KRA-94,KEDARAM CORGENTZ INFOTECH PRIVATE 23 NAGAR,PATTOM PO, TRIVANDRUM LIMITED KALLUVELIL HOUSE KANDAMTHITTA 24 AMALA AYURVEDIC PHARMA PANTHA PO TVM PUTHEN PURACKAL KP IV/450-C 25 NEAR AL-UTHMAN SCHOOL AARC METAL AND WOOD MENAMKULAM TVPM KINAVU HOUSE TC 18/913 (4) 26 KALYANI DRESS WORLD ARAMADA PO TVPM THAZHE VILAYIL VEEDU OPP. -

Univesity of Kerala
Price. Rs. 150/- per copy UNIVESITY OF KERALA Election to the Senate by the member of the Local Authorities- (Under Section 17-Elected Members (7) of the Kerala University Act 1974) Electoral Roll of the Members of the Local Authorities- Thiruvanathapuram District Roll Name of Members / Name of Local Authorties Address No. Coucillors 1 Smt. Chrystal sheeba Member,Parassala Grama Anu cottege, kalloorkonam, Panchayath Parasuvaickal. P.O 2 Smt. Freeja. R Member,Parassala Grama Pinarakkala Puthen veedu, Panchayath Parasuvaickal P.O 3 Smt. Savithri kumary Member,Parassala Grama Ajin nivas, kuttikkade Parasuvaickal. Panchayath P.O 4 Smt. Kensi Lali. S Member,Parassala Grama R k Bhavan, Panathadikonam , Panchayath Kizhakinkara Veedu Parasuvaickal. P . O 5 Sri. Binu Member,Parassala Grama kuzhakottukonam, kizhakkekara puthen Panchayath veedu, parasuvaickal. P,O 6 Smt. Suseela Member,Parassala Grama Nedumpazhinji veedu, Parasuvaickal. Panchayath P.O 7 Smt. Rajamma Member,Parassala Grama Adumancadu House Panchayath Idichakkaplamoodu,Parassala. P.O 8 Sri. Surendran Member,Parassala Grama Sreenandanam Assasrivila veedu, Panchayath Pavathiyanvila Parassala. P.O 9 Sri. Rajan Member,Parassala Grama kottavila Puthuvel puthen veedu, Panchayath karumanoor, Parassala. P .O 10 Smt. Anitha. V Member,Parassala Grama kanjiramvila veedu , Neduvanvila, Panchayath Parassala. P.O 11 Sri. k . Lawrence Member,Parassala Grama Thettikuzhi puthen veedu , kodavilakam Panchayath Parassala P .O 12 Smt. Girija Member,Parassala Grama Kunjuveetuvilakathu veedu, Muriyankara Panchayath Parassala P.o 13 Smt. Sukumary Member,Parassala Grama Villuvila veedu, Muryiankara, Parassala. Panchayath P.O 14 Smt. Neela. P A Member,Parassala Grama Sreepadmam post office junction , Panchayath Parassala. P.O 15 Sri. M. Sajin Member,Parassala Grama Naduthottam puthen veedu, Inchivila Panchayath Parassala. -

REETHA S PRABHA Chief Executive Officer (In-Charge)
PROCEEDINGS OF THE CHIEF EXECUTIVE OFFICER (IN- CHARGE), ADDITIONAL SKILL ACQUISITION PROGRAMME, THIRUVANANTHAPURAM PRESENT : Smt REETHA S PRABHA Sub:- Higher Education Department - Additional Skill Acquisition Programme- Exemption from payment of Fee for APL General students 2016-17 and 2017-18 - Thiruvananthapuram District - Sanctioned- Order issued No: ASAP/SPM-TRAINING/1835/2016 Dated, 27.09.2018 Read:- 1. GO ( MS) 27/ 2013 / HEdn Dated 04/02/ 2013, Thiruvananthapuram 2. G.O.(Rt)No. 517/2018/HEDN Dated 21/03/2018, Thiruvananthapuram 3. Minutes of Meeting Held by District Committee Thiruvananthapuram Dated 18/07/2018 ORDER Vide Order referred as 1st above Government has approved to exempt the APL- General students from the incentive linked fee of ASAP. As per order referred as 2nd above Government have permitted to pool the APL General students within the district where the total fee incentives per district will be less than or equal to two times the number of batches in the district. Vide the 3rd paper read above the ASAP District Committee of Thiruvananthapuram convened on 18th July 2018 has recommended to exempt a total of 103 students from payment of incentive linked fee of ASAP for the year 2016-17 and 140 students for the year 2017-18. Hence sanction is hereby accorded for exempting the students mentioned in the annexure from payment of the fee as per the incentive linked fee structure of ASAP. If any of these students have already paid the fee, the fee collected will be reimbursed to the students. Sd/- REETHA S PRABHA Chief Executive Officer (In-Charge) To The District Programme Manager Thiruvananthapuram, All divisions of ASAP The Finance Division ASAP, The Training Division ASAP Copy To The Internal Audit Team ASAP, The SF/OC The List of APL – General students exempted from the incentive linked fee structure of ASAP, from various institutions of Thiruvananthapuram district for the year 2016-17. -

Tamil Nadu Government Gazette
© [Regd. No. TN/CCN/467/2012-14. GOVERNMENT OF TAMIL NADU [R. Dis. No. 197/2009. 2017 [Price : Rs. Paise. TAMIL NADU GOVERNMENT GAZETTE PUBLISHED BY AUTHORITY No. 30A] CHENNAI, WEDNESDAY, JULY 26, 2017 Aadi 10, Thunmugi, Thiruvalluvar Aandu–2048 Part VI–Section 1 (Supplement) NOTIFICations BY HEADS OF departments, ETC. TAMIL NADU MEDICAL COUNCIL Supplementary Medical Register for 2017. DTP—VI-1 Sup. (30A)—1 [ 1 ] 2 TAMIL NADU MEDICAL REGISTER FOR 2017 SUPPLEMENTARY LIST (Ref. No. TNMC/Govt. Press/Printing 2/2017) No. VI(1)/218/2017. Note : An asterisk is placed against the names of Medical Practioners entitled to vote at elections to the Medical Council of India under Section 3(1)(c) of the Indian Medical Council Act, 1956. Serial Number Name Father's Name Qualifi cation Date of Place of Profession and Registration Registration. and Address. Number (1) (2) (3) (4) (5) (6) .."!0 9 '2*3 5$4&5 $6$6$$ /78/78./0 -$3'&+*3.' %*))%3)&51&&32)$ #///" 4&5 ...# 9 '%2*)15* $5$*(&-:2 $6$6$$ /.8/.8./0 :6&-43-;3-&'-/0.3"%2 %*))%3%2*-'3 5* +*32)$ #///7/ ./!7 9 ,*46*3 $-2)'46* $6$6$$ /#8/8./0 -$;!3:'*-'346* (*+2-)3%*()&5)&$ #.0//# -2)'46* 7.."; 9 42'2*(5 2)%4 $6$6$$ ..8/8./0 2+<7/3.%23!%2 *-31)&243)=%-=3 6+&-*)$ "#//#7 "./!"0 9 42)- 5$(*)24(* $6$6$$ /!8/8./0 4*2*))34('--*3* '($-%3)*4(&34)*&$ #;./7 #.7;! 9 425>1 5$5>1 $6$6$$ #8/#8./0 4(:2(5&1& 2-()31+&&1 $-$4-&&34)*&$ #!/"! 0.70!/ 9 423 6$2) $6$6$$ "8/#8./0 -$.;35& %*))%35435*('2(+ 2) *$ #.#. -

National Backward Classes & Finance Development
NATIONAL BACKWARD CLASSES & FINANCE DEVELOPMENT CORPORATION LIST OF BENEFICIARIES FOR THE FINANCIAL YEAR 2017-2018 Name of SCA : The Kerala State Women's Development Corporation Ltd. Urban/Ru Religion/Ca Benef. Date of Sl No Name_Address Scheme Age Project cost NBCFDC share SCA share ral ste Contribution finance EDUCATION LOAN (90%) CHANDINI.C., CHALAYILVELI, EDUCATION HINDU, 1 CHARAMANGALAM, R 83000 74700 8300 0 22-Sep-17 MUHAMMA P.O, LOAN EZHAVA ALAPPUZHA-688525 AMRUTHA R AJAYAN, KAVUNKAL KOOMBEL HOUSE, EDUCATION HINDU, 2 AROOKUTTY P.O, R 83000 74700 8300 0 22-Sep-17 LOAN DHEEVARA CHERTHALA, ALAPPUZHA-688535 ATHIRA V VINOD, VALASSERY HOUSE, EDUCATION HINDU, 3 KOLAZHY P.O, R 200000 180000 20000 0 25-Sep-17 ATHEKKADU, LOAN EZHAVA THRISSUR-680010 SAI KRISHNA SS., GOKULAM, NEAR EDUCATION HINDU, 4 U 21 200000 180000 20000 0 11-Sep-17 KUNJUVEEDU TEMPLE, THURUVIKKAL P LOAN EZHAVA O, TRIVANRUM MEENAKSHI PREMAN, CHUVANNARIYAN PADATH, EDUCATION 5 CHIRAKKAKOM, Rural 265000 238500 26500 0 25-Nov-17 LOAN VARAPPUZHA P.O, ERNAKULAM-683517 AMRUTHA.K, AMBALI(H) EDUCATION HINDU, 6 KADALUNDI(PO) Rural 123500 111150 12350 0 15-Dec-17 KOZHIKODE(DT) LOAN THIYYA PIN-673302 Page 1 of 211 Urban/Ru Religion/Ca Benef. Date of Sl No Name_Address Scheme Age Project cost NBCFDC share SCA share ral ste Contribution finance ADITHYA.K, KOLAKKAT(H) NADAKAVU(PO) EDUCATION HINDU, 7 Rural 69600 62640 6960 0 15-Dec-17 KOZHIKODE(DT) LOAN THIYYA PIN-673011 TOTAL - EL 10,24,100 9,21,690 1,02,410 - MICRO FINANCE SCHEME (90%) AMBADI SHG, WARD XIII, THANNISSERY, ULAVAIPPU P.O, -

2008-'09 2009-'10
NORKA-ROOTS Details of Santhwana Fund disbursed during the financial year : 2009-'10 Sl.No Name of the Non-Resident Address Mode of Assistance Amount Disbursed on Keralite disbursed 1 Kumaran Thilleri Munna Nivas Medical treatment 5,000.00 02/05/2009 Oarkkatteri P.O Vadakkara 673501 2 Hydrose K Kattuthottil House Medical treatment 5,000.00 02/05/2009 House No404 Chembra P.o Chembara 3 Sasidharan N N S Mandiram Medical treatment 10,000.00 10/05/2009 Vilavoorkkal Malayinkeezh P.O 4 Viswanathan Prakash Anoop Vilasom Medical treatment 9,000.00 10/05/2009 Kappil P.O Edava 5 K .Rajendran P G Bhavan Medical treatment 8,000.00 12/05/2009 Konnakode,Manaloor Neyattinkara P O 6 P K Viswanathan Pariyath House Medical treatment 10,000.00 03/07/2009 Nalukody P O Changanacherry 7 Chandrasekharan Paravath Pampini Medical treatment 8,000.00 03/07/2009 Thottilpalam Kavilumpara 8 Jimnesh M Jimnesh House Medical treatment 10,000.00 03/07/2009 Malayil Chemmathur P.O Kottappally Vatakara 9 Ayishabi Thaivalappil House Medical treatment 7,000.00 03/07/2009 Elathur P.O 10 Late Chandran Nallup Nalupurakkal House Death of the breadwinner 10,000.00 03/07/2009 Kavugal P.O Pazhoor Via Mavoor 1 Sl.No Name of the Non-Resident Address Mode of Assistance Amount Disbursed on Keralite disbursed 11 Late C.P. Abdul Latheef A.T House Death of the breadwinner 10,000.00 03/07/2009 Paslat Kandy Paramba P.O North Beypore Naduvattom 12 Late Nanu Nelliyulla Parambath Death of the breadwinner 10,000.00 03/07/2009 Vanimel Vadkara 13 Late C.B.Arun Appu Cottage Death of the breadwinner -
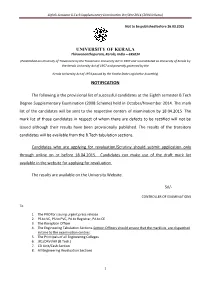
Eighth Semester B.Tech Supplementary Examination Oct/Nov 2014 (2008 Scheme)
Eighth Semester B.Tech Supplementary Examination Oct/Nov 2014 (2008 Scheme) Not to be published before 26.03.2015 UNIVERSITY OF KERALA Thiruvananthapuram, Kerala, India – 695034 (Established as University of Travancore by the Travancore University Act in 1937 and reconstituted as University of Kerala by the Kerala University Act of 1957 and presently governed by the Kerala University Act of 1974 passed by the Kerala State Legislative Assembly) NOTIFICATION The following is the provisional list of successful candidates at the Eighth semester B.Tech Degree Supplementary Examination (2008 Scheme) held in October/November 2014. The mark list of the candidates will be sent to the respective centers of examination by 18.04.2015. The mark list of those candidates in respect of whom there are defects to be rectified will not be issued although their results have been provisionally published. The results of the transitory candidates will be available from the B.Tech tabulation sections. Candidates who are applying for revaluation/Scrutiny should submit application only through online on or before 18.04.2015. Candidates can make use of the draft mark list available in the website for applying for revaluation. The results are available on the University Website. Sd/- CONTROLLER OF EXAMINATIONS To 1. The PRO for issuing urgent press release 2. PS to VC, PS to PVC, PA to Registrar, PA to CE 3. The Reception Officer 4. The Engineering Tabulation Sections-Section Officers should ensure that the marklists are dispatched in time to the examination centres. 5. The Principals of all Engineering Colleges 6. JR1/DRVI/AR (B.Tech.) 7. -

KSEB Electrical Section Codes
SMS Format -> KSEB <Space> Section Code<Space> Consumer No -> 537252 KSEB Electrical Section Codes Section Code Electrical Section Name 5617 Adimali 4609 Adoor 6516 Agali 6648 Alakode 6521 Alanellur 5501 Alappuzha ( North) 5502 Alappuzha (Town) 5503 Alappuzha(South) 6574 Alathiyoor 6509 Alathur 5568 Aluva North 5567 Aluva Town 5569 Aluva West 6534 Ambalappara 5505 Ambalappuzha 6762 Ambalavayal 4656 Amboori 5670 Ammadam 6756 Anakkayam 4597 Anchal 4669 Anchal (West) 6748 Angadipuram 5579 Angamaly. 5648 Annamanada 5553 Arakkunnam 5535 Aranmula 6789 Areekkad 6767 Areekkulam 6549 Areekode 5679 Arimboor 5705 Arookutty 5515 Aroor 5518 Arthinkal 4652 Aryanad 5572 Athani 4664 Athirampuzha 6615 Atholy 4531 Attingal. 4532 Avanavanchery. 4632 Ayarkunnam 4565 Ayathil. 6624 Ayenchery 4629 Aymanam 4591 Ayoor 4608 Ayroor 5678 Ayyanthole 6662 Azhikode 6743 Azhiyoor 6690 Badiadkka 6773 Balamthode 4542 Balaramapuram 6613 Balussery 6603 Beach 5699 Beach, Guruvayoor Page 1 of 13 SMS Format -> KSEB <Space> Section Code<Space> Consumer No -> 537252 4513 Beach, Trivandrum 6635 Beypore 5627 Bharananganam 6697 Bheemanady 5702 Big Bazar 6518 Bigbazar 6655 Burnassery 4558 Cantonment, Kollam 4506 Cantonment. 6602 Central, Kozhikode 4672 Chadayamangalam 6660 Chakkarakkal 6716 Chakkittapara 5651 Chalakudy 6538 Chalissery 6661 Chalode 5508 Champakulam 4636 Changanacherry 6585 Changaramkulam 6745 Chapparappadavu 5527 Charummood 4575 Chathannoor. 6772 Chattanchal 6708 Chattiparamba 5698 Chavakkad 4571 Chavara. 5691 Chelakkara 6744 Chelannur 6577 Chelari 6721 Chemperi 4644 -

Accused Persons Arrested in Thiruvananthapuram Rural District from 04.10.2020To10.10.2020 Name of Name of Arresting Name of the Place at Date & the Court Sl
Accused Persons arrested in Thiruvananthapuram Rural district from 04.10.2020to10.10.2020 Name of Name of Arresting Name of the Place at Date & the Court Sl. Name of the Age & Address of Cr. No & Police Officer, father of which Time of at which No. Accused Sex Accused Sec of Law Station Rank & Accused Arrested Arrest accused Designatio produced n 1 2 3 4 5 6 7 8 9 10 11 KUNNUMPURA ARYANAD NOTICE 2186/2020 SI THU VEEDU, 10-10-2020 (THIRUVA SERVED - 38, KAMPANI U/s 4(2)(E) MURALEE 1 SANTHOSH PATHROSE MANCHADIMO at 12:45 NANTHAP JFMC I, Male MUKK R/W 5 OF DHARAN ODU, Hrs URAM NEDUMA KEDO 2020 NAIR MYLAKKARA RURAL) NGADU 14/428, ARYANAD NOTICE 2185/2020 SI THADATHARIK 10-10-2020 (THIRUVA SERVED - 26, VELLANAD U/s 4(2)(E) MURALEE 2 ARUN SHAJI ATHU VEEDU, at 12:20 NANTHAP JFMC I, Male U R/W 5 OF DHARAN ATTUKAL, Hrs URAM NEDUMA KEDO 2020 NAIR VELLANADU RURAL) NGADU VARKALA 3660/2020 ARRESTE Souparnika,Vatta 10-10-2020 (THIRUVA 35, U/s 279 IPC Ajith D - JFMC 3 Sajan Babu plamoodu Nadayara jn at 20:10 NANTHAP Male & 185 MV Kumar I, colony,Panayara Hrs URAM ACT VARKALA RURAL) 1747/2020 U/s Sec. 4(2)(f) r/w 5 MARANAL Nellikkadu, of Kerala LOOR ARRESTE azhakam,kulappa 10-10-2020 47, Epidemic (THIRUVA Santhosh D - JFMC 4 Venu Soman llivilakom, Chappath at 19:50 Male Diseases NANTHAP kumar KATTAKA meleputhanveed, Hrs Ordinance URAM DA maranalloor 2020r/w 4(v) RURAL) , of regulationact 1746/2020 U/s Sec.