DRAFT – National Care Framework for Huntington's Disease (TEXT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Registration Form
CROSS-PARTY GROUP REGISTRATION FORM NAME OF CROSS-PARTY GROUP Cross-Party Group on Towns and Town Centres PURPOSE OF THE GROUP AND PROPOSED DISCUSSION TOPICS 1. Please state the purpose of the Group. 2. Please also provide a brief explanation of the purpose of the Group and why the purpose is in the public interest. 3. Please also provide details of any overlaps with the purpose of existing Cross- Party Groups and an explanation of why, regardless of any such overlap, the Group should be established. 4. Please also provide an indication of the topics which the Group anticipates discussing in the forthcoming 12 months. The purpose of the Group is to analyse policy prescriptions and develop ideas and innovations. This will help Scotland’s towns and town centres through the current economic climate to emerge stronger, smarter, cleaner, healthier and greener. The Group will discuss ways in which Scotland’s towns can work towards sustainable economic growth through greater vibrancy and vitality. The Group intends to discuss leadership, enterprise, inclusion and digital in relation to the towns agenda. MSP MEMBERS OF THE GROUP Please provide names and party designation of all MSP members of the Group. George Adam (SNP) Jackie Bailie (Scottish Labour) Neil Bibby (Scottish Labour) Graeme Dey (SNP) Jenny Gilruth (SNP) Daniel Johnson (Scottish Labour) Alex Johnstone (Scottish Conservative and Unionist Party) Alison Johnstone (Scottish Green Party) Gordon Lindhurst (Scottish Conservative and Unionist Party) Angus MacDonald (SNP) Gillian Martin (SNP) Willie Rennie (Scottish Liberal Democrats) John Scott (Scottish Conservative and Unionist Party) Andy Wightman (Scottish Green Party) NON-MSP MEMBERS OF THE GROUP For organisational members please provide only the name of the organisation, it is not necessary to provide the name(s) of individuals who may represent the organisation at meetings of the Group. -

Economy, Energy and Fair Work Committee: Annual Report 2020-21 Published in Scotland by the Scottish Parliamentary Corporate Body
Published 25 March 2021 SP Paper 1012 5th Report 2021 (Session 5) Economy, Energy and Fair Work Committee Comataidh Eaconamaidh, Lùth is Obair Chothromach Economy, Energy and Fair Work Committee: Annual Report 2020-21 Published in Scotland by the Scottish Parliamentary Corporate Body. All documents are available on the Scottish For information on the Scottish Parliament contact Parliament website at: Public Information on: http://www.parliament.scot/abouttheparliament/ Telephone: 0131 348 5000 91279.aspx Textphone: 0800 092 7100 Email: [email protected] © Parliamentary copyright. Scottish Parliament Corporate Body The Scottish Parliament's copyright policy can be found on the website — www.parliament.scot Economy, Energy and Fair Work Committee Economy, Energy and Fair Work Committee: Annual Report 2020-21, 5th Report 2021 (Session 5) Contents Introduction ____________________________________________________________1 Membership changes____________________________________________________1 Inquiries and reports_____________________________________________________2 COVID-19 – impact on Scotland’s businesses, workers and the economy ___________2 2021-22 Budget scrutiny _________________________________________________3 Energy Inquiry _________________________________________________________3 BiFab, the offshore wind energy sector and the Scottish supply chain ______________3 Scottish National Investment Bank draft missions ______________________________3 Climate Change Plan____________________________________________________4 One-off -

Economy, Energy and Fair Work Committee: Annual Report 2019-20 Published in Scotland by the Scottish Parliamentary Corporate Body
Published 3 June 2020 SP Paper 747 4th Report 2020 (Session 5) Economy, Energy and Fair Work Committee Comataidh Eaconamaidh, Lùth is Obair Chothromach Economy, Energy and Fair Work Committee: Annual Report 2019-20 Published in Scotland by the Scottish Parliamentary Corporate Body. All documents are available on the Scottish For information on the Scottish Parliament contact Parliament website at: Public Information on: http://www.parliament.scot/abouttheparliament/ Telephone: 0131 348 5000 91279.aspx Textphone: 0800 092 7100 Email: [email protected] © Parliamentary copyright. Scottish Parliament Corporate Body The Scottish Parliament's copyright policy can be found on the website — www.parliament.scot Economy, Energy and Fair Work Committee Economy, Energy and Fair Work Committee: Annual Report 2019-20, 4th Report 2020 (Session 5) Contents Introduction ____________________________________________________________1 Membership changes____________________________________________________1 Inquiries and reports_____________________________________________________2 Economic Data – Pre-release Access ______________________________________2 Pre-budget Scrutiny _____________________________________________________2 Construction and Scotland’s Economy ______________________________________2 Energy Statement ______________________________________________________3 Moveable Transactions Bill _______________________________________________3 Bank Closures _________________________________________________________4 Protected Trust Deeds ___________________________________________________4 -

Whole Day Download the Hansard
Wednesday Volume 661 12 June 2019 No. 312 HOUSE OF COMMONS OFFICIAL REPORT PARLIAMENTARY DEBATES (HANSARD) Wednesday 12 June 2019 © Parliamentary Copyright House of Commons 2019 This publication may be reproduced under the terms of the Open Parliament licence, which is published at www.parliament.uk/site-information/copyright/. 635 12 JUNE 2019 636 leave within two years. Will he go back to look at the House of Commons correspondence I have sent to the Department about this very serious problem? Wednesday 12 June 2019 Alok Sharma: Of course I will look at the correspondence and make sure that the appropriate Minister meets the The House met at half-past Eleven o’clock hon. Lady. Angela Crawley (Lanark and Hamilton East) (SNP): PRAYERS With regards to the DWP’s pensions policy, this Women and Equalities Minister—the fourth—has had the opportunity to reduce the gender pay gap and tackle [MR SPEAKER in the Chair] discrimination against those with disabilities, women and LGBT and BME people before another Prime Minister and another reshuffle. What is she going to Oral Answers to Questions achieve in this term? Alok Sharma: We in the DWP have introduced a range of measures across the whole Government to WOMEN AND EQUALITIES make sure that we are supporting those across all sectors of society into work. As I said, the hon. Lady just needs to look at the jobs figures: we have joint record high The Minister for Women and Equalities was asked— employment, record high women’s employment and record high ethnic minorities in employment. -
Social Security Committee, Joint Session with The
Social Security Committee Monday 13 March 2017 Session 5 © Parliamentary copyright. Scottish Parliamentary Corporate Body Information on the Scottish Parliament’s copyright policy can be found on the website - www.parliament.scot or by contacting Public Information on 0131 348 5000 Monday 13 March 2017 CONTENTS Col. INTER-GOVERNMENTAL CO-OPERATION ON SOCIAL SECURITY ............................................................................. 1 SOCIAL SECURITY COMMITTEE 6th Meeting 2017, Session 5 CONVENER *Sandra White (Glasgow Kelvin) (SNP) DEPUTY CONVENER Pauline McNeill (Glasgow) (Lab) COMMITTEE MEMBERS *George Adam (Paisley) (SNP) *Mark Griffin (Central Scotland) (Lab) *Alison Johnstone (Lothian) (Green) *Gordon Lindhurst (Lothian) (Con) *Ben Macpherson (Edinburgh Northern and Leith) (SNP) *Ruth Maguire (Cunninghame South) (SNP) *Adam Tomkins (Glasgow) (Con) *attended THE FOLLOWING ALSO PARTICIPATED: Lisa Baron-Broadhurst (Scottish Government) Deidre Brock MP (Scottish Affairs Committee) John Dickie (Child Poverty Action Group in Scotland) Margaret Ferrier MP (Scottish Affairs Committee) Stephen Hepburn MP (Scottish Affairs Committee) Stephen Kerr (Scottish Government) Chris Law MP (Scottish Affairs Committee) Professor Nicola McEwen (University of Edinburgh) Ian Murray MP (Scottish Affairs Committee) Mary Pattison (Department for Work and Pensions) Bill Scott (Inclusion Scotland) Pete Searle (Department for Work and Pensions) Pete Wishart MP (Scottish Affairs Committee) CLERK TO THE COMMITTEE Simon Watkins LOCATION The Mary Fairfax Somerville Room (CR2) 1 13 MARCH 2017 2 Bill Scott (Inclusion Scotland): I am director of Scottish Parliament policy for Inclusion Scotland. The Convener: Thank you very much. You are Social Security Committee all pretty well known not only to us but to the Westminster MPs. Monday 13 March 2017 I will kick off by asking each of you to characterise, from your perspective, the [The Convener opened the meeting at 09:30] relationship between the Scottish Government and Inter-governmental Co-operation the DWP. -

Economy, Energy and Fair Work Committee
Economy, Energy and Fair Work Committee Tuesday 26 November 2019 Session 5 © Parliamentary copyright. Scottish Parliamentary Corporate Body Information on the Scottish Parliament’s copyright policy can be found on the website - www.parliament.scot or by contacting Public Information on 0131 348 5000 Tuesday 26 November 2019 CONTENTS Col. DECISION ON TAKING BUSINESS IN PRIVATE ....................................................................................................... 1 MOVEABLE TRANSACTIONS BILL ........................................................................................................................ 2 ECONOMY, ENERGY AND FAIR WORK COMMITTEE 33rd Meeting 2019, Session 5 CONVENER *Gordon Lindhurst (Lothian) (Con) DEPUTY CONVENER *Willie Coffey (Kilmarnock and Irvine Valley) (SNP) COMMITTEE MEMBERS *Jackie Baillie (Dumbarton) (Lab) *Colin Beattie (Midlothian North and Musselburgh) (SNP) *Jamie Halcro Johnston (Highlands and Islands) (Con) *Dean Lockhart (Mid Scotland and Fife) (Con) *Richard Lyle (Uddingston and Bellshill) (SNP) *Gordon MacDonald (Edinburgh Pentlands) (SNP) *Andy Wightman (Lothian) (Green) *attended THE FOLLOWING ALSO PARTICIPATED: Dr Ross Anderson Professor George Gretton Dr Hamish Patrick (Shepherd and Wedderburn) Dr Andrew Steven Bruce Wood (Morton Fraser Lawyers) CLERK TO THE COMMITTEE Alison Walker LOCATION The David Livingstone Room (CR6) 1 26 NOVEMBER 2019 2 Scottish Parliament Moveable Transactions Bill Economy, Energy and Fair Work 09:48 Committee The Convener: Agenda item 2 is the draft -

Business Bulletin Iris Ghnothaichean
Friday 19 May 2017 Business Bulletin Iris Ghnothaichean Announcement A revised version of the Guidance on Private Bills has been published, and is available in PDF and HTML formats on the Parliament’s website under Parliamentary Business / Parliamentary procedure, or from this link: http://www.scottish.parliament.uk/parliamentarybusiness/Bills/79081.aspx The revised version reflects Rule-changes agreed on 20 April 2017 relating to the super-majority requirements of the Scotland Act 2016, together with minor corrections to Presiding Officer determinations on the “proper form” of Bills and the form of accompanying documents, and recommendations on the content of Bills. A new edition of the Guidance on Hybrid Bills will be published shortly, reflecting similar changes. Today's Business Meeting of the Parliament Committee Meetings There are no meetings today. There are no meetings today. Friday 19 May 2017 1 Today's Business Future Business Motions & Questions Legislation Other Gnothaichean an-diugh Gnothaichean ri teachd Gluasadan agus Ceistean Reachdas Eile Chamber | Seòmar Meeting of the Parliament There are no meetings today. Friday 19 May 2017 2 Today's Business Future Business Motions & Questions Legislation Other Gnothaichean an-diugh Gnothaichean ri teachd Gluasadan agus Ceistean Reachdas Eile Committees | Comataidhean Committee Meetings There are no meetings today. Friday 19 May 2017 3 Today's Business Future Business Motions & Questions Legislation Other Gnothaichean an-diugh Gnothaichean ri teachd Gluasadan agus Ceistean Reachdas -

Official Report
Meeting of the Parliament (Hybrid) Thursday 17 September 2020 Session 5 © Parliamentary copyright. Scottish Parliamentary Corporate Body Information on the Scottish Parliament’s copyright policy can be found on the website - www.parliament.scot or by contacting Public Information on 0131 348 5000 Thursday 17 September 2020 CONTENTS Col. FIRST MINISTER’S QUESTION TIME ..................................................................................................................... 1 Michelle Stewart (Victims’ Rights) ................................................................................................................ 2 Health Protection Scotland (Covid Guidance) .............................................................................................. 6 Covid-19 Testing Programme ....................................................................................................................... 9 Care Homes (Visits) ................................................................................................................................... 11 Leisure Trusts (Financial Position) ............................................................................................................. 13 Covid-19 Tests (Young Adults) ................................................................................................................... 14 Family Contact (Older and Disabled Care Home Residents) ........................................................................................... 16 Covid-19 (School Staff Support) -
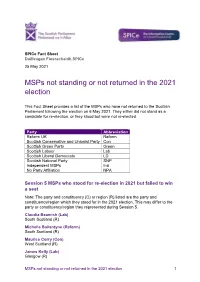
Msps Not Standing Or Not Returned in the 2021 Election
SPICe Fact Sheet Duilleagan Fiosrachaidh SPICe 25 May 2021 MSPs not standing or not returned in the 2021 election This Fact Sheet provides a list of the MSPs who have not returned to the Scottish Parliament following the election on 6 May 2021. They either did not stand as a candidate for re-election, or they stood but were not re-elected. Party Abbreviation Reform UK Reform Scottish Conservative and Unionist Party Con Scottish Green Party Green Scottish Labour Lab Scottish Liberal Democrats LD Scottish National Party SNP Independent MSPs Ind No Party Affiliation NPA Session 5 MSPs who stood for re-election in 2021 but failed to win a seat Note: The party and constituency (C) or region (R) listed are the party and constituency/region which they stood for in the 2021 election. This may differ to the party or constituency/region they represented during Session 5. Claudia Beamish (Lab) South Scotland (R) Michelle Ballantyne (Reform) South Scotland (R) Maurice Corry (Con) West Scotland (R) James Kelly (Lab) Glasgow (R) MSPs not standing or not returned in the 2021 election 1 Gordon Lindhurst (Con) Lothian (R) Joan McAlpine (SNP) South Scotland (R) John Scott (Con) Ayr (C) Paul Wheelhouse (SNP) South Scotland (R) Andy Wightman (Ind) Highlands and Islands (R) MSPs who were serving at the end of Parliamentary Session 5 but chose not to stand for re-election in 2021 Bill Bowman (Con) North East Scotland (R) Aileen Campbell (SNP) Clydesdale (C) Peter Chapman (Con) North East Scotland (R) Bruce Crawford (SNP) Stirling (C) Roseanna Cunningham (SNP) -

The Loch Ness Monster, Haggis, and a Lower Voting Age: What America Can Learn from Scotland
THE LOCH NESS MONSTER, HAGGIS, AND A LOWER VOTING AGE: WHAT AMERICA CAN LEARN FROM SCOTLAND JOSHUA A. DOUGLAS* This Article, prepared for an American University Law Review symposium, explores what the United States can learn from Scotland’s experience in lowering the voting age to sixteen. The minimum voting age in American elections seems firmly entrenched at eighteen, based in part on the Twenty-Sixth Amendment, which prohibits states from denying the right to vote to anyone aged eighteen or older. Yet the conversation about lowering the voting age to sixteen, at least for local elections, has gained steam in recent years. The debate in America, however, is nascent compared to the progress in Scotland, which lowered the voting age to sixteen for its Independence Referendum in 2014 and for all Scottish elections in 2015. Using original research from interviews I conducted in Scotland, this Article offers three main takeaways for American jurisdictions considering this reform: the Scottish experience in lowering the voting age has been mostly successful because advocates (1) went into schools to register students to vote and encourage them to participate; (2) offered meaningful civics education, though that instruction was somewhat uneven across the country; and (3) created a bipartisan coalition of policymakers who supported the change. As the debate on the voting age in the United States expands, advocates should draw upon these lessons from Scotland. * Thomas P. Lewis Professor of Law, University of Kentucky J. David Rosenberg College of Law. Thanks to Chris Bradley, Jan Eichhorn, Tony Gaughan, Andy McLaughlin, Andy Mycock, Carly Muetterties, and Lori Ringhand for comments on drafts of this Article. -

Meeting of the Parliament
Meeting of the Parliament Thursday 25 May 2017 Session 5 © Parliamentary copyright. Scottish Parliamentary Corporate Body Information on the Scottish Parliament’s copyright policy can be found on the website - www.parliament.scot or by contacting Public Information on 0131 348 5000 Thursday 25 May 2017 CONTENTS Col. GENERAL QUESTION TIME .................................................................................................................................. 1 Good Food Nation Bill ................................................................................................................................. 1 Transport (Rural Areas) ................................................................................................................................ 2 Road Safety (M74 Junction 21) .................................................................................................................... 3 Benefit Cap ................................................................................................................................................... 4 NHS Greater Glasgow and Clyde (Chief Executive Meetings) .................................................................... 5 Film Studio (Meetings) .................................................................................................................................. 7 FIRST MINISTER’S QUESTION TIME ..................................................................................................................... 9 Engagements ............................................................................................................................................... -
Holyrood Updated April 2021
SCOTLAND’S CIVIC LINKS WITH MALAWI CONSTITUENCY MAPPING: HOLYROOD UPDATED APRIL 2021 A briefing by the Scotland Malawi Partnership on the distribution of the 1,225 Scotland-Malawi links it represents, across Holyrood regions and constituencies 0 EXECUTIVE SUMMARY Each year more than 109,000 Scots are involved in a civic link with Malawi. The Scotland Malawi Partnership exists as a politically neutral and non-governmental membership networking helping to coordinate, represent and support the work of 1,225 organisations and key individuals linked with Malawi across Scotland. To do this, and to maintain all-party support for its members’ work with Malawi, the Scotland Malawi Partnership helps its members connect with their local MSP and MP, and to brief MSPs and Scottish MPs on Malawi links in their constituency. Every single constituency of Scotland has a number of civic Malawi partnerships and SMP members. This latest report, updated in April 2021, gives a handful of examples of Malawi links in each of Scotland’s 73 Holyrood constituencies and 8 regions. The partnerships contained in this report are just a fraction of all the Malawi links across Scotland. Full details can be found at www.scotland-malawipartnership.org. CONTENTS Midlothian North and Musselburgh 63 All-Party Foreword 2 Mid Scotland and Fife Region: 64 SMP Members 3 Clackmannanshire and Dunblane 65 Scotland and Malawi by numbers 11 Cowdenbeath 66 Scotland’s links with Malawi 12 Dunfermline 67 Constituency by constituency: Kirkcaldy 68 Central Scotland Region: 13 Mid Fife