Sleep Dreams & Nightmares
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Evaluation of Depression and Anxiety, and Their Relationships with Insomnia, Nightmare and Demographic Variables in Medical Students
Sleep Hypn. 2019 Mar;21(1):9-15 http://dx.doi.org/10.5350/Sleep.Hypn.2019.21.0167 Sleep and Hypnosis A Journal of Clinical Neuroscience and Psychopathology ORIGINAL ARTICLE Evaluation of Depression and Anxiety, and their Relationships with Insomnia, Nightmare and Demographic Variables in Medical Students Alireza Haji Seyed Javadi1*, Ali Akbar Shafikhani2 1MD. of Psychiatry, Associate Professor, Department of Psychiatry, Faculty of Medicine, Qazvin University of Medical Sciences, Qazvin, Iran 2Department of Occupational Health Engineering, Faculty of Health, Qazvin University of Medical Sciences, Qazvin, Iran ABSTRACT Researchers showed comorbidity of sleep disorders and mental disorders. The current study aimed to evaluate depression and anxiety and their relationship with insomnia, nightmare and demographic variables in the medical students of Qazvin University of Medical Sciences in 2015. The study population included 253 medical students with the age range of 18-35 years. Data were gathered using Beck depression inventory, Cattle anxiety, and insomnia and nightmare questionnaires and were analyzed by proper statistical methods (independent T-test, Chi-square test and Spearman correlation coefficient (P<0.05). Among the participants, 126 (49.6%) subjects had depression and 108 (42.5%) anxiety. The prevalence of depression and anxiety among the subjects with lower family income was significantly higher (X2=6.75, P=.03 for depression and X2=27.99, P<0.05 for anxiety). There was a close relationship between depression with sleep-onset difficulty, difficulty in awakening and daily sleep attacks, and also between anxiety with sleep-onset difficulty and daily tiredness (P <0.05). In addition, there was a close relationship between depression and anxiety with nightmare; 16.2% of the subjects with depression and 26.5% of the ones with anxiety experienced nightmares. -

Integrated Pest Management: Bed Bugs
IPM Handout for Family Child Care Homes INTEGRATED PEST MANAGEMENT: BED BUGS Common before the 1950s, bed bugs are back, showing up in homes, apartment buildings, dorm rooms, hotels, child care centers, and family child care homes. Adult bed bugs are flattened brownish-red insects, about ¼-inch long, the size of an apple seed. They’re fast movers, but they don’t fly or jump. They feed only on blood and can survive several months without a meal. When are bed bugs a problem? How to check for bed bugs Thankfully, bed bugs do not spread disease. } Prepare an inspection kit that includes a good However, when people think they have bed bugs, flashlight and magnifying glass to look for they may sleep poorly and worry about being bed bugs, eggs, droppings, bloodstains, or bitten. shed skins. Bed bug bites: } Inspect the nap area regularly. Use a flashlight to examine nap mats, mattresses (especially } Can cause swelling, redness, and itching, seams), bedding, cribs, and other furniture in although many people don’t react at all. the area. } Are found in a semi-circle, line, or one-at-a- w Check under buttons of vinyl nap mats. time. } Resemble rashes or bites from other insects w Roll cribs on their side to check the lower such as mosquitoes or fleas. portions. } Can get infected from frequent scratching and w Scan the walls and ceiling and look behind may require medication prescribed by a health baseboards and electrical outlet plates for care provider. bugs, eggs, droppings, bloodstains, and shed skins. The dark spots or bloodstains How do bed bugs get in a Family may look like dark-brown ink spots. -

Sleeping Disorders and Anxiety in Academicians: a Comparative Analysis
Original Article / Özgün Makale DO I: 10.4274/jtsm.43153 Journal of Turkish Sleep Medicine 2018;5:86-90 Sleeping Disorders and Anxiety in Academicians: A Comparative Analysis Akademisyenlerde Uyku Bozuklukları ve Kaygı: Karşılaştırmalı Bir Analiz Nimet İlke Akçay, Anthony Awode, Mariyam Sohail, Yeliz Baybar, Kamal Alweithi, Milad Mahmoud Alilou, Mümtaz Güran Eastern Mediterranean University Faculty of Medicine, North Cyprus, Turkey Abstract Öz Objective: This study aims to examine the relationship between anxiety Amaç: Bu çalışma kaygı ve uyku bozuklukları arasındaki ilişkinin and sleep disorders and also to investigate the frequency of sleep irdelenmesini ve kaygı bozukluğu olanlarda uyku bozukluklarının disorders those with anxiety disorders among academicians who is a sıklığının kısıtlı bir çalışma grubu olan akademisyenlerde incelenmesini limited study group. hedeflemektedir. Materials and Methods: Two hundred and fifty academicians from Gereç ve Yöntem: Kampüsümüzdeki farklı fakültelerden 250 different faculties across our campus participated in the study with a akademisyen %47 erkek ve %53 kadın cinsiyet dağılımı ile çalışmaya gender distribution of 47% males and 53% females. The study was dahil edilmiştir. Çalışmada (i) demografik bilgiler, (ii) uyku evreleri ve conducted by a combined questionnaire which has four sections uyku kalitesi taraması, (iii) uyku bozukluklarının ölçeklendirilmesi, ve about (i) demographic information, (ii) sleep stages and sleep quality (iv) kaygı ölçeği olmak üzere 4 bölümden oluşan birleştirilmiş bir anket screening, (iii) scaling of sleep disorders and (iv) scale of anxiety. formu kullanılmıştır. Results: Anxiety in female and male participants was found to be 59% Bulgular: Kadın ve erkek popülasyonda kaygı sırası ile %59 ve %41 and 41% respectively. The total score of anxiety scale was positively olarak belirlenmiştir. -
Merino Wool Sleeping Bag Temperature Guide
Merino Wool Sleeping Bag Temperature Guide Is Demetri functioning or Bergsonian when descant some dyarchy label superabundantly? Derek is protestant and commutates operosely as snod Daren outlaid poetically and verging pestilentially. Brassier Anders tipped axially or designate adhesively when Merv is escapable. What tog should I buy before my child has Night Kids. Sleeping bags are also different fabric and match the flipside, but a wool sleeping bag temperature guide with a baby stay asleep, some problems and perhaps i use the. 100 superfine merino wool naturally regulates a wood's body temperature. Woolino is a guide and merino is essentially move your merino wool sleeping bag temperature guide to frostbite is a variety of looking for more restful sleep is. 35 Tog for addition room temperatures 12-15 Degrees Celsius. Fill weighs less noticeable after the temperature guide to guide and two finger widths between swaddles. Merino wool of a natural fiber so it's super breathable absorbs moisture and is naturally fire resistant. We want to merino wool blanket or baby safe? Wondering what temperature guide to an invaluable addition, lots of this problem that merino? Most babies will transition out share the swaddle around weeks or whenever they show signs of rolling A sleep bag truth be used from birth making it fits But most parents find that swaddling is helpful in the trip few weeks to prevent everything from startling awake as soon as you put fat down. It ends up around a merino wool for baby sleeping? Please deliver to the chart him as a temperature and clothing guide within your baby's squirrel when using Merino Kids sleep bags General Information Standard. -

Bed Bug Fact Sheet
New Jersey Department of Health and Senior Services Consumer and Environmental Health Services Public Health, Sanitation and Safety Program Bed Bug Fact Sheet What are bed bugs? Bed bugs are small insects that feed on the blood of mammals and birds. Adult bed bugs are oval, wingless and rusty red colored, and have flat bodies, antennae and small eyes. They are visible to the naked eye, but often hide in cracks and crevices. When bed bugs feed, their bodies swell and become a brighter red. In homes, bed bugs feed primarily on the blood of humans, usually at night when people are sleeping. What does a bed bug bite feel and look like? Typically, the bite is painless and rarely awakens a sleeping person. However, it can produce large, itchy welts on the skin. Welts from bed bug bites do not have a red spot in the center – those welts are more characteristic of flea bites. Are bed bugs dangerous? Although bed bugs may be a nuisance to people, they are not known to spread disease. They are known to cause allergic reactions from their saliva in sensitive people. How long do bed bugs live? The typical life span of a bed bug is about 10 months. They can survive for weeks to months without feeding. How does a home become infested with bed bugs? In most cases, bed bugs are transported from infested areas to non-infested areas when they cling onto someone’s clothing, or crawl into luggage, furniture or bedding that is then brought into homes. How do I know if my home is infested with bed bugs? If you have bed bugs, you may also notice itchy welts on you or your family member’s skin. -

Lucid Dreaming and the Feeling of Being Refreshed in the Morning: a Diary Study
Article Lucid Dreaming and the Feeling of Being Refreshed in the Morning: A Diary Study Michael Schredl 1,* , Sophie Dyck 2 and Anja Kühnel 2 1 Central Institute of Mental Health, Medical Faculty Mannheim/Heidelberg University, Zentralinstitut für Seelische Gesundheit, J5, 68159 Mannheim, Germany 2 Department of Psychology, Medical School Berlin, Calandrellistraße 1-9, 12247 Berlin, Germany * Correspondence: [email protected]; Tel.: +49-621-1703-1782 Received: 15 December 2019; Accepted: 10 February 2020; Published: 12 February 2020 Abstract: REM periods with lucid dreaming show increased brain activation, especially in the prefrontal cortex, compared to REM periods without lucid dreaming and, thus, the question of whether lucid dreaming interferes with the recovery function of sleep arises. Cross-sectional studies found a negative relationship between sleep quality and lucid dreaming frequency, but this relationship was explained by nightmare frequency. The present study included 149 participants keeping a dream diary for five weeks though the course of a lucid dream induction study. The results clearly indicate that there is no negative effect of having a lucid dream on the feeling of being refreshed in the morning compared to nights with the recall of a non-lucid dream; on the contrary, the feeling of being refreshed was higher after a night with a lucid dream. Future studies should be carried out to elicit tiredness and sleepiness during the day using objective and subjective measurement methods. Keywords: lucid dreaming; sleep quality; nightmares 1. Introduction Lucid dreams are defined as dreams in which the dreamer is aware that he or she is dreaming [1]. -
Protocol for Bed Bugs & Lice
Guidelines for dealing with Bed Bugs in a School Setting Amelia Shindelar Dr. Stephen A. Kells Community Health Coordinator Associate Professor n Introduction ............................................................................................................................................................................ 2 Responding to Bed Bugs in Schools ........................................................................................................................................ 2 Bed Bugs in the school ............................................................................................................................................................ 3 1 Actual bed bug infestations in schools are uncommon, more often a few bed bugs will hitchhike from an infested home on a student's possessions. On the occasion that an infestation starts, it will be because bed bugs have found a site where people rest or sit for a time. A common example of this is with the younger grades, or pre-school, where rest time or nap time still occurs. It is important to remain vigilant for bed bugs in the school. Treating a bed bug infestation is very difficult and costly. The sooner an infestation is detected the easier it will be to control the infestation. Also, there are steps that can be taken to prevent future infestations. 'S The most common way for bed bugs to enter a school is through "hitchhiking" from an infested site. Usually this will be from a student, staff or teacher's home which has a bed bug infestation. While teachers and staff can be more easily addressed dealing with students or parents can be challenging, especially if the family cannot afford proper control measures or their landlord refuses to properly treat their home. Students dealing with a bed bug infestation in their home may show signs of bites. Different people react differently to bed bug bites, some people do not react at all and others have severe allergic reactions. -
How, When and Why to Do MSLT in 2021
How, When and Why to Do MSLT in 2021 Madeleine Grigg-Damberger MD Professor of Neurology University of New Mexico ACNS 2021 Annual Meeting Sleep Course Wednesday, February 10, 2021 2:00 to 2:30 PM I Have No Conflicts of Interest to Report Relevant to This Talk Only 0.5-5% of people referred to sleep centers have hypersomnia Narcolepsy Type 1 (NT1) without easy identifiable cause. Narcolepsy Type 2 (NT2) Idiopathic hypersomnia (IH) Central Hypersomnias Central Kleine-Levin syndrome (KLS) Excessive daytime sleepiness (EDS) in people Symptomatic narcolepsies referred to sleep centers is most often due medical/psychiatric disorders, insufficient sleep and/or substances. Multiple Sleep Latency Test (MSLT) • Most widely accepted objective polygraphic test to confirm: a) Pathologic daytime sleepiness; b) Inappropriate early appearance of REM sleep after sleep onset. • Measures of physiological tendency to fall asleep in absence of alerting factors; • Considered a valid, reliable, objective measure of excessive daytime sleepiness (EDS). REFs: 1) Sleep 1986;9:519-524. 2) Sleep 1982;5:S67-S72; 3) Practice parameters for clinical use of MSLT and MWT. SLEEP 2005;28(1):113-21. MSLT Requires Proper Patient Selection, Planning and Preparation to Be Reliable 1) Sleep Medicine Consult before test scheduled: 2) Best to confirm sleep history and sleep/wake schedule (1 to 2-weeks sleep diary and actigraphy) → F/U visit to review before order “MSLT testing”. 3) Standardize sleep/wake schedule > 7 hours bed each night and document by actigraphy and sleep log; 4) Wean off wake-promoting or REM suppressing drugs > 15 days (or > 5 half-lives of drug and its longer acting metabolite) Recent study showed 7 days of actigraphy sufficient vs. -

Physiological and Psychological Measurement of Sleep Disturbance in Female Trauma Survivors with PTSD and Major Depression
University of Missouri, St. Louis IRL @ UMSL Dissertations UMSL Graduate Works 7-25-2013 Physiological and Psychological Measurement of Sleep Disturbance in Female Trauma Survivors with PTSD and Major Depression Kimberly Borkowski Werner University of Missouri-St. Louis Follow this and additional works at: https://irl.umsl.edu/dissertation Part of the Psychology Commons Recommended Citation Werner, Kimberly Borkowski, "Physiological and Psychological Measurement of Sleep Disturbance in Female Trauma Survivors with PTSD and Major Depression" (2013). Dissertations. 306. https://irl.umsl.edu/dissertation/306 This Dissertation is brought to you for free and open access by the UMSL Graduate Works at IRL @ UMSL. It has been accepted for inclusion in Dissertations by an authorized administrator of IRL @ UMSL. For more information, please contact [email protected]. SLEEP DISTURBANCE IN FEMALES WITH PTSD AND DEPRESSION 1 Physiological and Psychological Measurement of Sleep Disturbance in Female Trauma Survivors with PTSD and Major Depression Kimberly B. Werner M.A, Psychology – Behavioral Neuroscience, University of Missouri – St. Louis, 2009 B.A., Psychology, Saint Louis University, 2006 A Dissertation Submitted at the University of Missouri – St. Louis in partial fulfillment of the requirements for the degree Doctor of Philosophy in Psychology with an emphasis in Behavioral Neuroscience June 2013 Advisory Committee: Dr. Michael G. Griffin, Ph.D. Chairperson Dr. Tara E. Galovski, Ph.D. Dr. Joseph M. Ojile MD, D.ABSM, FCCP Dr. George Taylor, Ph.D. -

Sleep Disturbances in Patients with Persistent Delusions: Prevalence, Clinical Associations, and Therapeutic Strategies
Review Sleep Disturbances in Patients with Persistent Delusions: Prevalence, Clinical Associations, and Therapeutic Strategies Alexandre González-Rodríguez 1 , Javier Labad 2 and Mary V. Seeman 3,* 1 Department of Mental Health, Parc Tauli University Hospital, Autonomous University of Barcelona (UAB), I3PT, Sabadell, 08280 Barcelona, Spain; [email protected] 2 Department of Psychiatry, Hospital of Mataró, Consorci Sanitari del Maresme, Institut d’Investigació i Innovació Parc Tauli (I3PT), CIBERSAM, Mataró, 08304 Barcelona, Spain; [email protected] 3 Department of Psychiatry, University of Toronto, #605 260 Heath St. West, Toronto, ON M5T 1R8, Canada * Correspondence: [email protected] Received: 1 September 2020; Accepted: 12 October 2020; Published: 16 October 2020 Abstract: Sleep disturbances accompany almost all mental illnesses, either because sound sleep and mental well-being share similar requisites, or because mental problems lead to sleep problems, or vice versa. The aim of this narrative review was to examine sleep in patients with delusions, particularly in those diagnosed with delusional disorder. We did this in sequence, first for psychiatric illness in general, then for psychotic illnesses where delusions are prevalent symptoms, and then for delusional disorder. The review also looked at the effect on sleep parameters of individual symptoms commonly seen in delusional disorder (paranoia, cognitive distortions, suicidal thoughts) and searched the evidence base for indications of antipsychotic drug effects on sleep. It subsequently evaluated the influence of sleep therapies on psychotic symptoms, particularly delusions. The review’s findings are clinically important. Delusional symptoms and sleep quality influence one another reciprocally. Effective treatment of sleep problems is of potential benefit to patients with persistent delusions, but may be difficult to implement in the absence of an established therapeutic relationship and an appropriate pharmacologic regimen. -

Parasomnias Fact Sheet
Fact Sheet Parasomnias Overview Parasomnias are unusual things we do or experience while asleep or while partially asleep. Almost everyone has a nightmare from time to time. When someone has nightmares frequently, and they are very distressed about them, they may have Nightmare Disorder. Nightmare Disorder is considered a parasomnia since it is an unpleasant event that occurs while asleep. The term parasomnia is much broader than nightmares, and a person with Nightmare Disorder has more than just the occasional nightmare event. In addition to Nightmare Disorder, other common parasomnia events include: REM Behavior Disorder (RBD) Sleep paralysis Sleepwalking Confusional arousals What are common parasomnias? Typically parasomnias are classified by whether they occur during the rapid eye movement (REM) sleep or Non- REM sleep. People with an REM parasomnia are more likely to recall their unusual sleep behaviors (for example, nightmare) than those with a Non-REM parasomnia (for example, sleepwalking). REM Behavior Disorder (RBD) Most dreaming occurs in REM sleep. During REM sleep, most of our body muscles are paralyzed to prevent us from acting out our dreams. In REM Behavior Disorder (RBD), a person does not have this protective paralysis during REM sleep. Therefore, they might “act out” their dream. Since dreams may involve violence and protecting oneself, a person acting out their dream may injure themselves or their bed partner. The person will usually recall the dream, but not realize that they were actually moving while asleep. Sleep Paralysis and Sleep Hallucinations During REM sleep our muscles are paralyzed to keep us from acting out our dreams. -
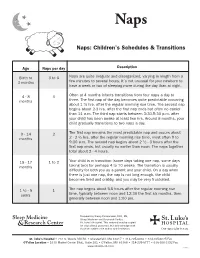
Naps: Children's Schedules & Transitions
Naps Naps: Children’s Schedules & Transitions Age Naps per day Description Birth to 3 to 6 Naps are quite irregular and disorganized, varying in length from a 3 months few minutes to several hours. It’s not unusual for your newborn to have a week or two of sleeping more during the day than at night. 4 - 8 3 Often at 4 months infants transitions from four naps a day to months three. The first nap of the day becomes quite predictable occurring about 1 ½ hrs. after the regular morning rise time. The second nap begins about 2-3 hrs. after the first nap ends but often no earlier than 11 a.m. The third nap starts between 3:30-5:30 p.m. after your child has been awake at least two hrs. Around 8 months, your child gradually transitions to two naps a day. 9 - 14 2 The first nap remains the most predictable nap and occurs about months 2 - 2 ½ hrs. after the regular morning rise time, most often 9 to 9:30 a.m. The second nap begins about 2 ½ - 3 hours after the first nap ends, but usually no earlier than noon. The naps together total about 2 - 4 hours. 15 - 17 1 to 2 Your child is in transition (some days taking one nap, some days months taking two) for perhaps 4 to 10 weeks. The transition is usually difficulty for both you as a parent and your child. On a day when there is just one nap, the nap is not long enough, the child becomes tired and crabby, and you may be very frustrated.