The Dead Space After Addition of Oxygen and Premedication with Narcotics and Belladonna Drugs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Term Respiratory Quotient (RQ) of Wastewater Samples
International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056 Volume: 05 Issue: 10 | Oct 2018 www.irjet.net p-ISSN: 2395-0072 Design and Fabrication of a Micro-respirometer to Measure the Short- Term Respiratory Quotient (RQ) of Wastewater Samples M. S. Rahman1, M. Z. Mousumi2, M. A. A. Sakib2, M. S. A. Fahad2, T. J. CHY2 & N. M. H. Robiul3 1Associate Professor, Department of Civil and Environmental Engineering, Shahjalal University of Science and Technology, Sylhet, Bangladesh. 2Student, Department of Civil and Environmental Engineering, Shahjalal University of Science and Technology, Sylhet, Bangladesh. 3Assistant Professor, Department of Civil and Environmental Engineering, Shahjalal University of Science and Technology, Sylhet, Bangladesh. ----------------------------------------------------------------------***--------------------------------------------------------------------- Abstract - The main objective of the study is to develop a activity [4, 5]. Therefore, the respiration process and its low-cost wastewater micro-respirometer to determine some qualitative and quantitative phenomena could be an effective important bioactivity performance indicators such as oxygen indicator of the on-going condition of a typical consumption rate (OCR), carbon dioxide evolution rate (CER) biodegradation process. Respirometric parameters such as and respiratory quotient (RQ) of wastewater samples collected cumulative oxygen consumption (COC), oxygen consumption from effluent treatment plants (ETPs) and other wastewater rate (OCR), cumulative carbon-dioxide evolution (CCE), sources. The developed apparatus was comprised of two major carbon dioxide evolution rate (CER) and respiratory parts, a reaction chamber and a measuring unit facilitated quotient (RQ) can ascertain the presence of organic matters, with a well type vertical volumeter. Validation of the newly microbes and respiration type present in wastewater by fabricated respirometer was done by checking the observing microbial activities [4, 5, 6]. -

Monitoring Anesthetic Depth
ANESTHETIC MONITORING Lyon Lee DVM PhD DACVA MONITORING ANESTHETIC DEPTH • The central nervous system is progressively depressed under general anesthesia. • Different stages of anesthesia will accompany different physiological reflexes and responses (see table below, Guedel’s signs and stages). Table 1. Guedel’s (1937) Signs and Stages of Anesthesia based on ‘Ether’ anesthesia in cats. Stages Description 1 Inducement, excitement, pupils constricted, voluntary struggling Obtunded reflexes, pupil diameters start to dilate, still excited, 2 involuntary struggling 3 Planes There are three planes- light, medium, and deep More decreased reflexes, pupils constricted, brisk palpebral reflex, Light corneal reflex, absence of swallowing reflex, lacrimation still present, no involuntary muscle movement. Ideal plane for most invasive procedures, pupils dilated, loss of pain, Medium loss of palpebral reflex, corneal reflexes present. Respiratory depression, severe muscle relaxation, bradycardia, no Deep (early overdose) reflexes (palpebral, corneal), pupils dilated Very deep anesthesia. Respiration ceases, cardiovascular function 4 depresses and death ensues immediately. • Due to arrival of newer inhalation anesthetics and concurrent use of injectable anesthetics and neuromuscular blockers the above classic signs do not fit well in most circumstances. • Modern concept has two stages simply dividing it into ‘awake’ and ‘unconscious’. • One should recognize and familiarize the reflexes with different physiologic signs to avoid any untoward side effects and complications • The system must be continuously monitored, and not neglected in favor of other signs of anesthesia. • Take all the information into account, not just one sign of anesthetic depth. • A major problem faced by all anesthetists is to avoid both ‘too light’ anesthesia with the risk of sudden violent movement and the dangerous ‘too deep’ anesthesia stage. -

The Use of Oxygen Consumption and Ammonium Excretion To
Chemosphere 84 (2011) 9–16 Contents lists available at ScienceDirect Chemosphere journal homepage: www.elsevier.com/locate/chemosphere The use of oxygen consumption and ammonium excretion to evaluate the toxicity of cadmium on Farfantepenaeus paulensis with respect to salinity ⇑ Edison Barbieri a, , Eduardo Tavares Paes b a Instituto de Pesca – APTA – SAA/SP, Caixa Postal 61, Cananéia 11990-000, São Paulo, Brazil b Instituto Socioambiental e dos Recursos Hídricos (ISARH) – Universidade Federal Rural da Amazônia (UFRA), Brazil article info abstract Article history: The main purpose of the present study was to detect the acute toxicity of cadmium (Cd) in F. paulensis Received 1 November 2010 and to investigate its effect on oxygen consumption and ammonium excretion different salinities. First, Received in revised form 8 February 2011 we examined the acute toxicity of Cd in F. paulensis at 24, 48, 72, and 96-h lethal concentration Accepted 14 February 2011 (LC50). Cd was significantly more toxic at 5 salinity than at 20 and 36. The oxygen consumption and Available online 7 April 2011 ammonium excretion were estimated through experiments performed on each of the twelve possible combinations of three salinities (36, 20 and 5), at temperature 20 °C. Cd showed a reduction in oxygen Keywords: consumption at 5 salinity, the results show that the oxygen consumption decreases with respect to Shrimp the Cd concentration. At the highest Cd concentration employed (2 mg LÀ1), the salinity 5 and the tem- Cd Salinity perature at 20 °C, oxygen consumption decreases 53.7% in relation to the control. In addition, after sep- Oxygen consumption arate exposure to Cd, elevation in ammonium excretion was obtained, wish were 72%, 65% and 95% Ammonium excretion higher than the control, respectively. -

The Influence of Environmental PO∑ on Hemoglobin Oxygen Saturation In
The Journal of Experimental Biology 208, 309-316 309 Published by The Company of Biologists 2005 doi:10.1242/jeb.01410 The influence of environmental PO∑ on hemoglobin oxygen saturation in developing zebrafish Danio rerio Sandra Grillitsch1,2, Nikolaus Medgyesy1,2, Thorsten Schwerte1,2 and Bernd Pelster1,2,* 1Institute for Zoology and Limnology, University of Innsbruck, Austria and 2Center for Molecular Biosciences, Innsbruck, Austria *Author for correspondence (e-mail: [email protected]) Accepted 24 November 2004 Summary Several studies suggest that during early larval deoxygenated blood (413·nm and 431·nm, respectively) development of lower vertebrates convective blood flow is under normoxic conditions and after a 10·min period of not essential to supply oxygen to the tissues, but hyperoxia (PO∑=100·kPa), assuming that at a PO∑ of information about the oxygenation status of larvae during 100·kPa the hemoglobin is fully saturated. The results the time of cutaneous respiration is still missing. If demonstrated that red blood cell oxygenation of zebrafish convective oxygen transport contributes to the oxygen larvae at 4 days post fertilization (d.p.f.), 5·d.p.f. and supply to tissues, venous blood in the central circulatory 12·d.p.f. could be increased by hyperoxia. The data system should be partly deoxygenated, and hyperoxia suggest that at the time of yolk sac degradation (i.e. should increase the oxygen saturation of the hemoglobin. 4·d.p.f. and 5·d.p.f.), when the total surface area of the To analyze the changes in hemoglobin oxygen saturation animal is reduced, bulk diffusion of oxygen may not be induced by hyperoxic incubation, zebrafish larvae sufficient to prevent a partial deoxygenation of the were incubated in a tiny chamber between hemoglobin. -

Respiration Quotient Variability: Bacterial Evidence
Vol. 519: 47–59, 2015 MARINE ECOLOGY PROGRESS SERIES Published January 20 doi: 10.3354/meps11062 Mar Ecol Prog Ser Respiration quotient variability: bacterial evidence V. Romero-Kutzner1,*, T. T. Packard1, E. Berdalet2, S. O. Roy3, J.-P. Gagné4, M. Gómez1 1EOMAR, Grupo de Ecofisiología de Organismos Marinos, Universidad de Las Palmas de Gran Canaria 35017, Spain 2Institut de Ciències del Mar (CSIC), Passeig Marítim de la Barceloneta, 37-49, 08003 Barcelona, Spain 310 Ryan Court, Embrun, Ontario K0A 1W0, Canada 4Université du Québec à Rimouski, Rimouski, Québec G5L 3A1, Canada ABSTRACT: Respiratory metabolism was compared between 2 different physiological states of acetate- and pyruvate-grown cultures of Pseudomonas nautica and Vibrio natriegens. Here, we analyze 35 h and 520 h experiments in which time-courses of protein, pyruvate, acetate, respira- tory CO2 production (RCO2), respiratory O2 consumption (RO2), isocitrate dehydrogenase (IDH) activity, and potential respiration (Φ) were measured. Respiratory quotients (RQs) were calculated as the ratio of the respiration rates (RCO2/RO2). Such RQs are widely used in ocean ecosystem mod- els, in calculations of carbon flux, and in evaluations of the ocean’s metabolic balance. In all the cultures, the RQ tended to increase. In the case of P. nautica on acetate, the RQ rose nearly an order of magnitude from values below 1 during carbon-substrate sufficiency to values close to 10 during carbon-substrate deficiency. In all the cultures, the respiration rates during the growth period paralleled the biomass increase, but after the substrates were exhausted, the respiration rates fell. In contrast, through this same transition period, the IDH activity and the Φ remained rel- atively high for the first 10 h of carbon-substrate deprivation, and then, these enzyme activities fell slowly, along with the biomass, as the carbon-substrate deprivation continued. -

The Oxygen Consumption and Efficiency of the Respiratory Muscles in Health and Emphysema
THE OXYGEN CONSUMPTION AND EFFICIENCY OF THE RESPIRATORY MUSCLES IN HEALTH AND EMPHYSEMA Reuben M. Cherniack J Clin Invest. 1959;38(3):494-499. https://doi.org/10.1172/JCI103826. Research Article Find the latest version: https://jci.me/103826/pdf THE OXYGEN CONSUMPTION AND EFFICIENCY OF THE RESPIRATORY MUSCLES IN HEALTH AND EMPHYSEMA * BY REUBEN M. CHERNIACK t (From The Winnipeg General Hospital and the Departments of Medicine and Physiology and Medical Research, University of Manitoba, Winnipeg, Canada) (Submitted for publication August 4, 1958; accepted October 23, 1958) The work of moving the lung, chest wall, dia- eral levels of increased ventilation by a modification of a phragm and abdominal contents during spontane- method previously described (2). The apparatus em- ployed is illustrated in Figure 1. The subject breathed ous respiration is performed by the muscles of into and out of a 9 L. Collins respirometer with carbon respiration. In order to obtain a better under- dioxide absorber incorporated. A cam on the pulley of standing of the disability present in pulmonary the spirometer activated a micro-switch which in turn disease it would be advantageous to have, in nor- opened and closed a solenoid valve through which oxy- mal and diseased states, a measure of the total gen could be delivered from a second spirometer. The micro-switch was activated towards end-inspiration so work being done, the energy cost of performing that a nonsloping record of tidal volumes and the inte- this work and the efficiency of the muscles of res- grated minute ventilation were obtained on the first piration. -

Respirometry – a Valuable Tool in Wastewater Treatment
Respirometry – A Valuable Tool in Wastewater Treatment Presented By: John Hoffman, President of Alloway Respirometry - Introduction Respirometry in Control of the Activated Sludge Process. Water Science and Technology. Spanjers, Vanrolleghem, Olsson, and Doldt. Volume 34, 3-4, P. 117-126 Respirometry - Introduction • Respirometry is a general term that encompasses a number of techniques for obtaining estimates of the rates of metabolism of vertebrates, invertebrates, plants, tissues, cells, or microorganisms…. (Cited from Wikipedia and others) • Today: Respirometry is the measurement and interpretation of the respiration rate of activated sludge. Respirometry – Introduction A respirometer is a device used to measure the rate of respiration of a living organism by measuring its rate of exchange of oxygen and/or carbon dioxide. Image From: Estimation of Instantaneous Gas Exchange in Flow-Through Respirometry Systems: A Modern Revision of Bartholomew's Z-Transform Method. Pendar H, Socha JJ (2015) Estimation of Instantaneous Gas Exchange in Flow-Through Respirometry Systems: A Modern Revision of Bartholomew's Z-Transform Method. PLOS ONE 10(10): e0139508. Respirometry – Introduction • The respiration rate = amount of oxygen per unit of volume and time that is consumed by microorganisms • Two important processes that must be controlled in a wastewater treatment plant: • Biomass Growth • Substrate Consumption Respirometry – Introduction The primary objective in a wastewater treatment system (usually): Meet regulatory objectives by the removal of carbonaceous material through the growth of heterotrophic bacteria. Nitrification by autotrophic organisms may account for about 40% of the oxygen demand. Respirometry – Introduction Respiration rate is usually measured with a respirometer. Photo by: Aragón, C., M.D. Coello, J.M. -

Indirect Calorimetry
Dr. Robert Robergs Fall, 2010 Indirect Calorimetry CALORIMETRY The science that quantifies the heat release from metabolism is termed calorimetry. CALORIMETRY Direct Indirect CalorimeterClosed Circuit Open Circuit Respiration • Expired gas analysis Chamber • Carbon/nitrogen excretion • Labeled water • Respiration chamber Figure 4.5 Indirect Calorimetry 1 Dr. Robert Robergs Fall, 2010 Bomb Calorimeter Indirect Calorimetry 2 Dr. Robert Robergs Fall, 2010 Heat release & caloric equivalents macronutrients The heat release and caloric equivalents for oxygen for the main macronutrients of catabolism (simplified). Food Rubner’s Kcal/g Kcal/g RQ Kcal/L O2 kcal/g (Bomb cal.) (body) CHO mix 4.1 4.1 4.0 1.0 5.05 Fat mix 9.3 9.3 8.9 0.70 4.73 Protein 4.1 5.7 4.3 0.81 4.46 mix Alcohol 7.1 7.0 0.82 4.86 Mixed Diet 0.84 4.83 Indirect Calorimetry 3 Dr. Robert Robergs Fall, 2010 Applications of Indirect Calorimetry • Maximal Cardiorespiratory and Muscular Endurance (VO2max) • Metabolic Intensity Absolute - VO2 (mL/kg/min or L/min) Relative - % VO2max ; % LT • Economy and Efficiency • Accumulated O2 Deficit • Metabolic Rate (BMR, RMR) • EPOC • Energy Expenditure • VO2 Kinetics Limitations Of Indirect Calorimetry 1. Whole body - the sum of all active tissue in body, not just contracting skeletal muscle. 2. Needs sophisticated and expensive equipment. 3. Highly sensitive to measurement error. 4. Can only be accurately used for metabolic intensities, economy, efficiency, and energy expenditure during steady state exercise. 5. Requires subjects to wear apparatus on face or in mouth. Indirect Calorimetry 4 Dr. Robert Robergs Fall, 2010 Systems of Measurement Inspired volume time-average system Expired volume time-average system Custom Built System Flow turbine Mixing bag Flow pump Expired gas analyzers Indirect Calorimetry 5 Dr. -
Devices to Use & What the Results Mean
ANESTHETICPEER REVIEWED MONITORING Devices to Use & What the Results Mean Jeff Ko, DVM, MS, Diplomate ACVA, and Rebecca Krimins, DVM This article is the second in a he main fundamental aspects of anesthetic monitor- ing are: series discussing the goals of 1. Oxygenation (circulatory and respiratory func- tion) anesthetic monitoring as well 2. Ventilation (respiratory function) T 3. Circulation (circulatory function with an empha- as associated procedures sis on cardiac output). and equipment. In the first These three elements work simultaneously in order to maintain adequate tissue and organ perfusion with oxygenated blood.1-3 article, the authors answered Oxygenation and ventilation are essential for maintaining a high oxygen level in the blood, while cardiac output plays a questions about anesthetic pivotal role in maintaining tissue and organ perfusion with highly monitoring, including why oxygenated blood. In this way, oxygenation, ventilation, and cir- culation each play a critical role in providing oxygen to tissues. itÕs performed, information PHYSIOLOGY FUNDAMENTALS obtained during monitoring, Oxygen Delivery Oxygen delivery is a product of blood oxygenation and cardiac and important components output.1-3 of the anesthetic process. UÊBlood oxygenation is represented by blood oxygen con- tent, which is the total amount of oxygen carried by the blood, including oxygen dissolved in plasma and oxygen bound to hemoglobin.1-3 UÊCardiac output is maintained by a complex interaction involving heart rate, stroke volume, peripheral vascular resistance (afterload), blood volume returning to the heart (preload), and blood viscosity.1-3 March/April 2012 Today’s Veterinary Practice 23 | ANESTHETIC MONITORING: DEVICES TO USE & WHAT THE RESULTS MEAN When heart rate or stroke volume or a combination Table 1. -
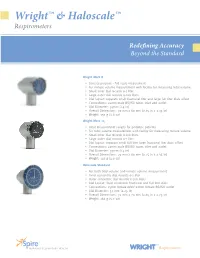
Wright™ & Haloscale™
Wright™ & Haloscale™ Respirometers Redefining Accuracy Beyond the Standard Wright Mark 8 • General purpose - full scale meaurement • For minute volume measurement with facility for measuring tidal volume • Small inner dial records 0-1 liter • Large outer dial records 0-100 liters • Dial layout: separate small fractional liter and large full liter dials offset • Connections: 22mm male BS/ISO taper, inlet and outlet • Dial Diameter: 35mm (1.4 in) • Overall Dimensions: 70 mm x 60 mm (2.75 in x 2.35 in) • Weight: 130 g (4.6 oz) Wright Mark 14 • Ideal measurement ranges for pediatric patients • For tidal volume measurement with facility for measuring minute volume • Small inner dial records 0-100 liters • Large outer dial records 0-1 liter • Dial layout: separate small full liter large fractional liter dials offset • Connections: 22mm male BS/ISO taper, inlet and outlet • Dial Diameter: 35mm (1.4 in) • Overall Dimensions: 70 mm x 60 mm (2.75 in x 2.35 in) • Weight: 130 g (4.6 oz) Haloscale Standard • For both tidal volume and minute volume measurement • Inner concentric dial records 0-1 liter • Outer concentric dial records 0-100 liters • Dial Layout: Dual concentric fractional and full liter dials • Connections: 15mm female inlet/ 22mm female BS/ISO outlet • Dial Diameter: 57 mm (2.25 in) • Overall Dimensions: 72 mm x 70 mm (2.85 in x 2.75 in) • Weight: 160 g (5.7 oz) TM TM Inspiring Respiratory Health WRIGHT Respirometers Technical Specifications Redefining Accuracy. Accuracy: Tidal volumes: Beyond Expectations. + 3% for minute volumes exceeding 5 LPM + 4% for minute volume of 4 LPM Continuous flow: No respiratory volume measurement instrument is more + 2% @ 16 LPM recognized throughout the world. -
Respiration Rates in Planarians
BIOLOGICAL SCIENCES Respiration Rates in Planarianl I. The Use of the Warburg Respirometer in Determining Oxygen ConsumptionI MABIE M. JENKINS, UDlverslt, 01 Oklahoma, Norman The rate of respiration in planarians has been investigated by a num ber of workers using various techniques. One of the earliest to do re search in this field was tibbie H. Hyman, who reported her findings in a series of articles pUblished about torty years ago. Her work has been confirmed by severalt whlle others have reported results which differ from hers to a greater or lesser degree. Th1B conflict appears to stem both from disagreement over interpretation of results obtained and from ques tions concerning the accuracy of the apparatus or method used In the determination of the respiratory rate. The Winkler method for measuring dissolved oxygen in water was used by Hyman (1919a) to determine the oxygen conaumptlon of planarl ana. In a later paper (1932) she presented statistical evidence defending the accuracy of the Winkler method in reply to Shearer's crlticl8m (1930) of her work based on his own manometric observations. Allee and 08st1ng (1934) presented a critical evaluatlon of the Winkler method, comparing it with other methods of determining oxygen consumption. They repeated some of the experiments of Hyman and others, and concluded that although some of Hymants figures might be erroneously high, due to a nitrite error, such error "need not have affected Hyman'S conclusions regarding oxygen consumption for the given experiments." Fraps (1930) found the manometric method of Warburg adequate for measurement or oxygen consumption in planarlans when certain modifica tions were applled. -

Lung Capacity Respiratory System Name: ______Date: ______Period: _____
Lung Capacity Respiratory System Name: _________________________ Date: ___________ Period: _____ Objective: Demonstrate and explain lung capacity. Key Terms: Expiration Expiratory reserve volume Inspiration Inspiratory reserve volume Residual volume Respiration Respirometer Spirometer Tidal volume Vital capacity Background Information: Inspiration, breathing in, and expiration, breathing out, occur because of a pressure gradient. Clinically, the term respiration includes one inspiration plus one expiration. The amount of air taken in or expelled during normal breathing is called the tidal volume. When a very deep breath is taken, the volume of inhaled air is known as the inspiratory reserve volume. When a normal breath is taken in and then forcibly expelled it is known as the expiratory reserve volume. The vital capacity is the maximum amount of air that can be exhaled after taking the deepest breath possible. Residual volume is the amount of air left in lungs even after maximal expiration. Human lung capacity can be measure in several ways. One way is by using a piece of laboratory equipment called a respirometer or spirometer. A less accurate (but very sanitary) method to measure lung capacity is by using a balloon. Procedure A: VITAL CAPACITY 1. Blow up the balloon several times to stretch it before beginning to take measurements. 2. Take as deep a breath as possible: exhale as much air as possible into the balloon; pinch the balloon closed to prevent air from escaping. 3. Measure and record the circumference of the balloon. 4. Repeat this procedure four more times; record each circumference. 5. Calculate and record the average. Procedure B: EXPIRATORY RESERVE 1.