Clear Cell Acanthoma: New Observations on Dermatoscopy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pilar Sheath Acanthoma Presenting As a Nevus
Letter to Editor Pilar Sheath Acanthoma Presenting as a Nevus Sir, Pilar sheath acanthoma (PSA) is a rare benign follicular neoplasm, which was first described by Mehregan and Brownstein in 1978.[1] PSA usually presents as an asymptomatic, flesh colored papule with a central opening localized at the lower lip with exceptional presentations such as ear lobe, postauricular region, or cheek.[1‑3] A 42‑year‑old female referred with a solitary, slow‑growing nodular lesion at the upper lip region for 6 months. Physical exam revealed a 4 mm, pink‑brown colored nodule with a central opening [Figure 1]. Under clinical prediagnosis of melanocytic nevus, an excisional biopsy Figure 1: Physical examination of the nodule in the upper lip region was performed. In a microscopic examination, a cystic cavity that communicated with surface epidermis has been observed. The wall of the cystic cavity was composed of solid tumor islands extending in the deep dermis [Figure 2]. The cavity was lined with stratified squamous epithelium filled with keratin [Figure 3]. PSA is an uncommon, benign follicular tumor occurring in the faces of middle‑aged and elderly patients. These lesions can present at any location such as cheek, ear lobe on the head, and neck. In our case, a 42‑year‑old female was presented with a pink‑brown colored nodular lesion opening at the upper lip region. The differential diagnosis includes trichofolliculoma and dilated pore of Winer. Trichofolliculomas contain many seconder hair follicles Figure 2: A central cavity with keratin in the dermis which is continuous radiating from the wall of the primary follicle with outer with the surface epithelium (H and E, ×40) and inner root sheaths in a well‑formed stroma which are absent in PSA. -

The Tamilnadu Dr. M.G.R. Medical University Chennai, Tamil Nadu
CLINICO-PATHOLOGICAL STUDY OF SKIN SURFACE EPIDERMAL AND APPENDAGEAL TUMOURS Dissertation Submitted in partial fulfillment of university regulations for M.D. DEGREE IN DERMATOLOGY, VENEREOLOGY AND LEPROSY BRANCH XII – A THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY CHENNAI, TAMIL NADU SEPTEMBER 2006 CERTIFICATE This is to certify that this Dissertation entitled “CLINICO-PATHOLOGICAL STUDY OF SKIN SURFACE EPIDERMAL AND APPENDAGEAL TUMOURS” is a bonafide work done by DR.G.BALAJI, Postgraduate student of Department of Dermatology, Leprosy and Institute of STD, Madras Medical College and Government General Hospital, Chennai – 3 for the award of Degree of M.D.( Dermatology, Venereology and Leprosy ) Branch XII – A during the academic year of 2003-2006. This work has not previously formed in the basis for the award of any degree or diploma. Prof. Dr. B. Parveen, MD., DD., Professor & Head, Dept. of Dermatology and Leprosy, Madras Medical College & Govt. General Hospital, Chennai – 3. Prof. Dr. Kalavathy Ponniraivan, MD., The Dean Madras Medical College & Govt. General Hospital, Chennai – 3. SPECIAL ACKNOWLEDGEMENT I sincerely thank Prof. Dr. Kalavathy Ponniraivan, MD., Dean, Madras Medical College & Govt. General Hospital, Chennai – 3, for granting me permission to use the resources of this institution for my study. ACKNOWLEDGEMENT I sincerely thank Prof. B.Parveen MD.,DD, Professor and Head of Department of Dermatology for her invaluable guidance and encouragement for the successful completion of this study. I express my heart felt gratitude to Dr.N.Gomathy MD.,DD, former Head of department of Dermatology who was instrumental in the initiation of this project, giving constant guidance throughout my work. -

What Are Basal and Squamous Cell Skin Cancers?
cancer.org | 1.800.227.2345 About Basal and Squamous Cell Skin Cancer Overview If you have been diagnosed with basal or squamous cell skin cancer or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Are Basal and Squamous Cell Skin Cancers? Research and Statistics See the latest estimates for new cases of basal and squamous cell skin cancer and deaths in the US and what research is currently being done. ● Key Statistics for Basal and Squamous Cell Skin Cancers ● What’s New in Basal and Squamous Cell Skin Cancer Research? What Are Basal and Squamous Cell Skin Cancers? Basal and squamous cell skin cancers are the most common types of skin cancer. They start in the top layer of skin (the epidermis), and are often related to sun exposure. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer cells. To learn more about cancer and how it starts and spreads, see What Is Cancer?1 Where do skin cancers start? Most skin cancers start in the top layer of skin, called the epidermis. There are 3 main types of cells in this layer: ● Squamous cells: These are flat cells in the upper (outer) part of the epidermis, which are constantly shed as new ones form. When these cells grow out of control, they can develop into squamous cell skin cancer (also called squamous cell carcinoma). -

Hair Follicle Tumors
Hair Follicle Tumors 803-808-7387 www.gracepets.com These notes are provided to help you understand the diagnosis or possible diagnosis of cancer in your pet. For general information on cancer in pets ask for our handout “What is Cancer”. Your veterinarian may suggest certain tests to help confirm or eliminate diagnosis, and to help assess treatment options and likely outcomes. Because individual situations and responses vary, and because cancers often behave unpredictably, science can only give us a guide. However, information and understanding for tumors in animals is improving all the time. We understand that this can be a very worrying time. We apologize for the need to use some technical language. If you have any questions please do not hesitate to ask us. What is this tumor? This is one of many similar tumors that arise by disordered growth of the hair follicles. These tumors are almost all benign and can be permanently cured by total surgical removal. Some occur at multiple sites within the same animal. This family of tumors grade into each other. Precise nomenclature is usually irrelevant as almost all are benign. What do we know about the cause? The reason why a particular pet may develop this, or any cancer, is not straightforward. Cancer is often seemingly the culmination of a series of circumstances that come together for the unfortunate individual. Cross Section of Skin & Hair Follicle B-catenin is required for differentiation of skin cells into hair follicles. If there is over-production of this chemical in the body, hair follicle tumors develop. -

Expert-Level Diagnosis of Nonpigmented Skin Cancer by Combined Convolutional Neural Networks
Supplementary Online Content Tschandl P, Rosendahl C, Akay BN, et al. Expert-level diagnosis of nonpigmented skin cancer by combined convolutional neural networks. JAMA Dermatol. Published online November 28, 2018. doi:10.1001/jamadermatol.2018.4378 eFigure. Sensitivities (Blue) and Specificities (Orange) at Different Threshold Cutoffs (Green) of the Combined Classifier Evaluated on the Validation Set eAppendix. Neural Network Training eTable 1. Complete List of Diagnoses and Their Frequencies Within the Test-Set eTable 2. Education of Users According to Their Experience Group eTable 3. Percent of Correct Prediction of the Malignancy Status for Specific Diagnoses of a CNN Using Either Close-up or Dermatoscopic Images This supplementary material has been provided by the authors to give readers additional information about their work. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/25/2021 eFigure. Sensitivities (Blue) and Specificities (Orange) at Different Threshold Cutoffs (Green) of the Combined Classifier Evaluated on the Validation Set A threshold cut at 0.2 (black) is found for a minimum of 51.3% specificity. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/25/2021 eAppendix. Neural Network Training We compared multiple architecture and training hyperparameter combinations in a grid-search fashion, and used only the single best performing network for dermoscopic and close-up images, based on validation accuracy, for further analyses. We trained four different CNN architectures (InceptionResNetV2, InceptionV3, Xception, ResNet50) and used model definitions and ImageNet pretrained weights as available in the Tensorflow (version 1.3.0)/ Keras (version 2.0.8) frameworks. -
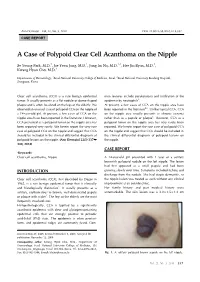
A Case of Polypoid Clear Cell Acanthoma on the Nipple
Ann Dermatol Vol. 22, No. 3, 2010 DOI: 10.5021/ad.2010.22.3.337 CASE REPORT A Case of Polypoid Clear Cell Acanthoma on the Nipple Se Young Park, M.D.1, Jae Yoon Jung, M.D.1, Jung Im Na, M.D.1,2, Hee Jin Byun, M.D.1, Kwang Hyun Cho, M.D.1 Departments of Dermatology, 1Seoul National University College of Medicine, Seoul, 2Seoul National University Bundang Hospital, Seongnam, Korea Clear cell acanthoma (CCA) is a rare benign epidermal mon features include parakeratosis and infiltration of the tumor. It usually presents as a flat nodule or dome-shaped epidermis by neutrophils3. plaque and is often localized on the legs of the elderly. We At present, a few cases of CCA on the nipple area have observed an unusual case of polypoid CCA on the nipple of been reported in the literature4-6. Unlike typical CCA, CCA a 14-year-old girl. At present, a few cases of CCA on the on the nipple area usually presents as chronic eczema nipple area have been reported in the literature. However, rather than as a papule or plaque6. However, CCA as a CCA presented as a polypoid tumor on the nipple area has polypoid tumor on the nipple area has very rarely been been reported very rarely. We herein report the very rare reported. We herein report the rare case of polypoid CCA case of polypoid CCA on the nipple and suggest that CCA on the nipple and suggest that CCA should be included in should be included in the clinical differential diagnosis of the clinical differential diagnosis of polypoid lesions on polypoid lesions on the nipple. -

Just a Cutaneous (Keratotic) Horn?
BMJ 2019;364:l595 doi: 10.1136/bmj.l595 (Published 7 March 2019) Page 1 of 2 Endgames BMJ: first published as 10.1136/bmj.l595 on 7 March 2019. Downloaded from ENDGAMES SPOT DIAGNOSIS Just a cutaneous (keratotic) horn? Jane Wilcock general practitioner, Yvonne Savage Silverdale Medical Practice, Salford, Manchester, UK A 70 year old woman attended a dermatologist with a lesion on In this case, the speed of growth made a keratoacanthoma a the dorsum of her right hand (fig 1). It had appeared over eight possibility. However, the patient also had several risk factors weeks and was painless but unsightly. She reported good health for squamous cell cancer: age, sun exposure, past lymphoma,1 and no history of warts. Fifteen years ago, she had lymphoma past chemotherapy, and no history of warts. Other invasive treated by chemotherapy; her last treatment (biological therapy) features of squamous cell cancer relevant to this case include had finished seven years ago and she had been well since. She the lesion’s arrival over eight weeks and its wide, thick, red base had holidayed in Australia for three months at a time over the with a diameter larger than the height of the horn. About 35% 2 last three years and more recently had driven frequently from of keratotic horns are invasive squamous cell cancers. http://www.bmj.com/ northern England to the south coast while a close relative was Invasive squamous cell cancer is a non-melanotic skin ill. She said she was careful to use sunscreen. malignancy with a good prognosis but may metastasise to the lymph nodes. -

Seborrheic Keratosis
Benign Epidermal and Dermal Tumors REAGAN ANDERSON, DO- PROGRAM DIRECTOR, COLORADO DERMATOLOGY INSTITUTE, RVU PGY3 RESIDENTS- JONATHAN BIELFIELD, GEORGE BRANT PGY2 RESIDENT- MICHELLE ELWAY Seborrheic Keratosis Common benign growth seen after third/fourth decade of life Ubiquitous among older individuals Tan to black, macular, papular, or verrucous lesion Occur everywhere except palms, soles, and mucous membranes Can simulate melanocytic neoplasms Pathogenesis: Sun exposure- Australian study found higher incidence in the head/neck Alteration in distribution of epidermal growth factors Somatic activating mutations in fibroblast growth factor receptor and phosphoinositide-3-kinase Seborrheic Keratosis Sign of Leser-Trelat: Rare cutaneous marker of internal malignancy • Gastric/colonic adenocarcinoma, breast carcinoma, and lymphoma m/c • Abrupt increase in number/size of SKs that can occur before, during, or after an internal malignancy is detected • 40% pruritus • M/C location is the back • Malignant acanthosis nigricans may also appear in 20% of patients • Should resolve when primary tumor is treated, and reappear with recurrence/mets Seborrheic Keratosis 6 Histologic types Acanthotic Hyperkeratotic Reticulated Irritated Clonal Melanoacanthoma Borst-Jadassohn phenomenon Well-demarcated nests of keratinocytes within the epidermis Seborrheic Keratoses Treatment Reassurance Irritated SKs (itching, catching on clothes, inflamed) Cryotherapy, curettage, shave excision Pulsed CO2, erbium:YAG lasers Electrodessication Flegel -

GRAND ROUNDS Department of Dermatology
Calderm 2017 NorCal Conference Jiminy Cricket & Appropriate Use in Dermatopathology Maxwell A. Fung, MD Professor of Clinical Dermatology & Pathology University of California, Davis Sacramento, California No relevant financial relationships “Audience response (ARS)” a) Do you read your own dermpath? b) Read path for other providers? c) Mostly read path reports? +/- recut review d) More than one of the above? Objectives • Gain insight: WHEN to listen to the “little voice” in your head to “do the right thing,” improve patient care and stay out of trouble • “Appropriate Use”: a concept to improve patient care, stay out of trouble, reduce cost, and get paid Highly predictive dermpath “rule outs” • Epidermal inclusion cyst Ring CM, et al. Clinical simulators of cysts. J Am Acad Dermatol 2016; 75:1255-1257. • Lipoma • Skin tag • Pyogenic granuloma • Granuloma annulare 58/M “r/o cyst” left chest 58/M “r/o cyst” left chest 22/M “FINAL DIAGNOSIS: CYST, EXCISION” 22/M “FINAL DIAGNOSIS: CYST, EXCISION” Post-op √ “Wound is closed, no redness” 22/M “FINAL DIAGNOSIS: CYST, EXCISION” What would you do next? a) Accept diagnosis b) Additional excision c) Call pathologist d) Review pathology/2nd opinion “FINAL DIAGNOSIS: CYST, EXCISION” What is the “official” disease of California? Coccidioidomycosis (California disease, Valley fever, San Joaquin Valley fever, desert rheumatism) H&E • Coccidioides immitis • Thick walled spherule PAS containing endospores 10-80 mm “FINAL DIAGNOSIS: CYST, EXCISION” Annular plaques in a woman from SoCal • 81/WF from The OC • 4 year history annular erythematous dermal plaques • Started on left upper arm • Clinical diagnosis: GA (multiple derms) 81 yr old woman R/O GA right flank 81 yr old woman, R/O GA 81 yr old woman, R/O GA 81 yr old woman, R/O GA 81 yr old woman, R/O GA 81 yr old woman, R/O GA What is your diagnosis? a) Actinic granuloma b) Granuloma annulare c) Interstitial granulomatous dermatitis d) Other 81 yr old woman, R/O GA GA-like BT leprosy Zhu TH, Kamangar F, Silverstein M, Fung MA. -

7. Clear Cell Acanthoma
Listy do Redakcji / Letters to the Editor CLEAR CELL ACANTHOMA – OPIS PRZYPADKU CASE REPORT OF CLEAR CELL ACANTHOMA Brzezi ński Piotr 6 Wojskowy Oddział Gospodarczy, Ustka, Polska 6th Military Support Unit, Ustka, Poland, [email protected] N Dermatol Online. 2010; 1(2): 29-30 Acanthoma clarocellulare (ACC) wyst ępuje Clear cell acanthoma (CCA) is characterized by jako pojedynczy, ró żowo-br ązowy guzek i zwykle pink-brown nodules and usually occurs on the legs of zlokalizowany jest na ko ńczynie dolnej u osób starszych. elderly people. ACC został po raz pierwszy opisany przez Degosa jako CCA was first described by Degos as a benign tumor of łagodny nowotwór pochodzenia nabłonkowego. ACC epidermal origin. Clear cell acanthoma are also known as wyst ępuje równie ż pod innymi nazwami: Degos Degos acanthoma, tumor Degos or acanthome à cellules acanthoma, guz Degosa czy acanthome à cellules claires. Some authors have also suggested that it is a claires. localized form of inflammatory psoriasiform dermatoses. Niektórzy autorzy sugeruj ą, że jest to forma The diagnosis is rarely made before skin biopsy. When zlokalizowanego łuszczycopodobnego zapalenia skóry. examined under the microscope, clear cell acanthoma Diagnoza jest rzadko stawiana przed otrzymaniem show a characteristic accumulation of clear glycogen- wyniku biopsji skóry. W badaniu pod mikroskopem, containing cells in the epidermis. The common wida ć jasne komórki, które wykazuj ą cechy kumulacji i dermatoscopic feature of all these articles is the presence zawieraj ą glikogen. Charakterystyczn ą cech ą w obrazie of pinpoint-like/dotted vessels, which are described as dermoskopowym jest obecno ść tzw. pinpoint-like/dotted having a homogenous/bunch-like, reticular, pearl vesseles, które s ą opisane jako homogenne, podobne do lessions. -

Keratoacanthomas Information for Patients You Have Been Given a Diagnosis of Keratoacanthoma
Department of Dermatology Keratoacanthomas Information for patients You have been given a diagnosis of keratoacanthoma. This leaflet has been written to give you more information about this condition and the different ways it can be treated. What are keratoacanthomas (also known as KAs)? Keratoacanthomas are relatively common skin growths. They are not cancerous but at first they look and behave like a form of skin cancer. They grow quickly over a few weeks, appearing at first as a small reddish bump which then becomes a bigger nodule, often with a central horn or plug. If left alone KAs usually go away by themselves – although this can take weeks or months to do so. They can appear anywhere on the body, but are most common in sun-exposed areas, such as the face, neck, and the back of the hands and arms. They are more likely to develop as you get older. What causes keratoacanthomas? The exact cause of KAs is not known. It is thought that sun exposure, contact with tar, smoking, some wart viral infections, injury to the skin and a suppressed immune system can lead to an increased risk of developing KAs. Are keratoacanthomas hereditary (passed from parent to child)? The majority are not hereditary, although they may be present as a feature of some rare inherited conditions. How is keratoacanthoma diagnosed? The doctor will have diagnosed your keratoacanthoma by asking you some questions and looking at its appearance. However, because it can look very similar to a skin cancer called a squamous cell carcinoma, the most common diagnosis (and treatment) is to remove it surgically and send a tissue sample to the laboratory to be tested. -

A Deep Learning System for Differential Diagnosis of Skin Diseases
A deep learning system for differential diagnosis of skin diseases 1 1 1 1 1 1,2 † Yuan Liu , Ayush Jain , Clara Eng , David H. Way , Kang Lee , Peggy Bui , Kimberly Kanada , ‡ 1 1 1 Guilherme de Oliveira Marinho , Jessica Gallegos , Sara Gabriele , Vishakha Gupta , Nalini 1,3,§ 1 4 1 1 Singh , Vivek Natarajan , Rainer Hofmann-Wellenhof , Greg S. Corrado , Lily H. Peng , Dale 1 1 † 1, 1, 1, R. Webster , Dennis Ai , Susan Huang , Yun Liu * , R. Carter Dunn * *, David Coz * * Affiliations: 1 G oogle Health, Palo Alto, CA, USA 2 U niversity of California, San Francisco, CA, USA 3 M assachusetts Institute of Technology, Cambridge, MA, USA 4 M edical University of Graz, Graz, Austria † W ork done at Google Health via Advanced Clinical. ‡ W ork done at Google Health via Adecco Staffing. § W ork done at Google Health. *Corresponding author: [email protected] **These authors contributed equally to this work. Abstract Skin and subcutaneous conditions affect an estimated 1.9 billion people at any given time and remain the fourth leading cause of non-fatal disease burden worldwide. Access to dermatology care is limited due to a shortage of dermatologists, causing long wait times and leading patients to seek dermatologic care from general practitioners. However, the diagnostic accuracy of general practitioners has been reported to be only 0.24-0.70 (compared to 0.77-0.96 for dermatologists), resulting in over- and under-referrals, delays in care, and errors in diagnosis and treatment. In this paper, we developed a deep learning system (DLS) to provide a differential diagnosis of skin conditions for clinical cases (skin photographs and associated medical histories).