Lower-Limb Flexibility Profile Analysis in Youth Competitive Inline Hockey Players
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
IX. Rules of the Game
International Handball Federation IX. Rules of the Game c) Wheelchair Handball Edition: 27 February 2020 Edition: 27 February 2020 Page 1 Table of contents Foreword 1. Basics 1.1. The Game 1.2. The Team 1.3. Players 1.4. Playing Time 1.5. The Ball 1.6. The Court 1.7. Goal 1.8. Equipment 1.9. Playing Kit 1.10. Straps 2. Wheelchair Specifications 3. The Game 3.1. Playing the Ball 3.2. Violations Edition: 27 February 2020 Page 2 Foreword The IHF Rules of the Game for Wheelchair Handball basically follow the IHF Rules of the Game for Indoor Handball. No special rules shall apply despite having mixed teams. However, due to the different capabilities of players, the amendments listed below shall be implemented and will be used for the upcoming IHF Wheelchair Handball events. Note: In some countries, competitions are organised for only 4 players (including goalkeeper) on the field. The international rules of this variation are currently being prepared. Edition: 27 February 2020 Page 3 ARTICLE 1 I. Basics 1.1. The Game Wheelchair handball is played by two teams of six players including one goalkeeper per team. The aim of each team is to score goals and to prevent the other team from scoring. Wheelchair handball shall be based on the spirit of Fair Play, dedicated for players with physical impairments. 1.2. The Team A team delegation consists of a maximum of 20 persons including a minimum of 12 players and a maximum of 16 players. A minimum of three female players shall be part of the team. -

Original Article Morphological Characteristics of Adolescent Elite Female Handball and Volleyball Players
Journal of Physical Education and Sport ® (JPES), Vol 19 (Supplement issue 4), Art 217 pp 1502 – 1507, 2019 online ISSN: 2247 - 806X; p-ISSN: 2247 – 8051; ISSN - L = 2247 - 8051 © JPES Original Article Morphological characteristics of adolescent elite female handball and volleyball players NOUTSOS S. KONSTANTINOS 1, MELETAKOS G. PANAGIOTIS 2, BAYIOS A. IOANNIS 3 1,2,3, Sector of Sports Games, School of Physical Education & Sports Science, National & Kapodistrian University of Athens, Ethnikis Antistasis 41, Daphne, 17237,GREECE Published online: July 31, 2019 (Accepted for publication: July 10, 2019) DOI:10.7752/jpes.2019.s4217 Abstract: The aim of the current study is to compare morphological characteristics of adolescent elite female handball and volleyball players and to investigate probable differences between them. The sample of the current study consists of athletes from women’s national handball teams (n=32, age=17.8±1.1 years, body height 166.6±4.5 cm, body mass 65.0±5.4 kg) and volleyball (n=16, age=18.0±1.4 years, body height 176.5±5.7 cm, body mass 68.1±7.4 kg). The measurements included five skin folds thicknesses (biceps, triceps, subscapular, suprailiac and calf), three circumferences [calf and biceps girth (relaxed and tensed)] end two widths (femur, humerus). In the initial somatometric parameters, the athletes exhibit higher performance triceps (p<0.001), subscapular (p<0.001) skinfold (mm) and biceps girth (relaxed) (cm) while volleyball players exhibit body height (cm) (p<0.05) and humeral diameter (cm) (p<0.05). In the secondary parameters, handball players express statistically significant body mass indices (kg/m²) (p<0.05), body fat (%) (p<0.002), sum of 5 skinfold (mm) (p<0.001), while volleyball players express fat free mass (kg) (p<0.001). -
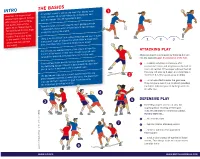
British Handball Game Guide
HE BASICS INTRO T A Handball match is won by the team that scores most Handball, the second most times over two 30 minute halves, by throwing the ball popular team sport in Europe past the keeper into the opposition’s goal. after football, is an exciting, fast paced, high scoring Teams consists of 6 court players and 1 goalkeeper with game. As an Olympic sport, 7 substitutes. Any number of substitutions can be made Handball is set to draw huge at any time during the match. crowds this summer in London. This is your guide to the basics of the game There is no ‘shot clock’ in Handball. Referees can warn a team 1 2 3 so you can keep up with if they don’t make an attempt to score within a reasonable the action! time. They then have 5 seconds to launch an attack Free throws are awarded where a foul occurs or from the ATTACKING PLAY 9m line if foul occurs in this zone. Penalties punish more Attacking players aim to score by throwing the ball serious foul play and are taken from the 7 metre mark into the opposing goal. In possession of the ball... If the ball leaves the end of the court possession goes to ... a player may take a maximum of 3 the defending keeper. If touched by a defending player first, consecutive steps and may bounce the ball as then a corner is awarded to the attacking team. much as desired. If the player catches the ball they may not bounce it again and must take a The goalkeeper may act as a court player, but is the only maximum 3 further steps, pass or shoot player allowed inside the 6 metre goal area. -

Operating Instructions Control Consoles
Multisport 452 OPERATING INSTRUCTIONS CONTROL CONSOLES Models with programmable team names Models with programmable numbers and names of the players Models with individual fouls Models with or without individual points Non-binding pictures ZI de Bel Air 44850 LE CELLIER FRANCE [email protected] Tél. +33 (0)2 40 25 46 90 UA452MXX12X-123_B - Control console 452M alpha & players.docx Page 1 SUMMARY Pages 3-5 Generalities 3 Scope of delivery 3 Data backup 3 Control console recharge (radio-controlled model) 4 Functions of the main control console 5 Functions of separate timer control console Pages 6-7 Set-up and Programming 6 Set-up 6 Select a sport or a function 6 Programme the parameters of the sports 7 Programme the team names, the number and the name of the players Pages 8-9 Various configurations 8 Access to the "General configuration" mode 8 Language of the control console 8 USB-keyboard type 8 Display of the clock on the scoreboard 8 Control console transmission mode (standard radio-controlled model) 9 Basketball - Led-strip display at the end of the ball possession time (24s.) 9 Basketball – Steady or blinking led-strip display 9 Global reset of the console parameters 9 In case of new sports rules (USB key) Pages 9-41 Sports and functions 9 Clock 10-11 Basketball 12-13 Handball 14-15 Volleyball 16-17 Tennis 18-19 Table Tennis 20-21 Badminton 22-23 Rink-Hockey 24-25 Inline-Hockey 26-27 Ice-Hockey 28-29 Uni-Hockey / Floorball 30-31 Soccer / Futsal 32-33 Netball 34-35 Boxing 36 Timer Function 37 Training Timer Function 38-39 "Free" mode – "Periods" mode 40-41 "Free" mode – "Sets" mode ZI de Bel Air 44850 LE CELLIER FRANCE [email protected] Tél. -

Team Handball Rules
Team Handball – Tournament Rules I. The Playing Court: A. The playing court begins at the end line paint and goes to the opposite end of the court. The goal-line is at the end of the actual court, not the paint. On either side of the court, width wise, the paint is in. If a player steps beyond the paint on either side they are out of bounds. The 3-point line is the goal area. II. Number of Players: A. There are seven players on each team (six court players and one goalie). A maximum of 12 players may dress and participate in a game for each team. Substitutes may enter the game at any time through own substitution area as long as the player they are replacing has left the court. B. There must always be a minimum of 2 women or 2 men on the court respectively. III. Referees: A. There is one referee. The referees are assisted by a timer/scorer. IV. Duration of the Game: A. The game consists of 2, 20- minute halves. This is running time except for injury or one team time-out per half. B. Teams switch sides at half. C. Overtime consists of 2, 5-minute periods. In regular tournament play after overtime if the score remains a tie then it will be recorded as a tie. In post seasons play there will be a penalty shot-foul consisting of five throws per team. D. Game begins with a jump ball. After point scored the goal keeper of the team scored on puts the ball back in play from the goal area. -

Team Handball Study Guide
MIDDLE SCHOOL PE TEAM HANDBALL STUDY GUIDE Although popular throughout much of the world, team handball is just starting in the United States. The sport uses natural athletic skills such as running, jumping, throwing and catching to provide action for the game. Spectators describe team handball as soccer with your hands, but they also notice things that remind them of basketball, water polo and ice hockey. Team handball is one of the world’s fastest team games. Two sides of seven players, including the goalie, play it. The object is to score the most goals by throwing the ball into the opponent’s goal and attackers pass or dribble the ball with their hands until a shooting opportunity is created. When a team loses possession of the ball, that team goes on defense. HOW A GAME STARTS: A Throw-off is taken from half-court. Every player must be in his/her own half of the field and opponents must be 10 feet from the thrower until the ball is thrown. MOVING THE BALL: Passing the ball is the best way to move the ball. A player may also dribble the ball as is done in basketball. A player may take only 3 steps while holding the ball. He/she may then dribble the ball, stop dribbling, and take 3 more steps. Once a player stops moving, he/she has 3 seconds to throw the ball. He/she may dribble the ball once with one hand while running. A player may bounce or roll the ball to another player. A player may roll the ball with one hand along the ground. -

SELECT COMMITTEE on OLYMPIC and PARALYMPIC LEGACY Oral and Written Evidence
SELECT COMMITTEE ON OLYMPIC AND PARALYMPIC LEGACY Oral and written evidence Contents Active in Time Ltd—Written evidence ................................................................................................. 3 Association for Physical Education (afPE)—Written evidence ......................................................... 8 Big Lottery Fund—Written evidence .................................................................................................. 16 BioRegional—Written evidence ........................................................................................................... 21 Boff, Andrew—Written evidence ........................................................................................................ 24 Boggis, Emma—Written evidence ........................................................................................................ 35 British Gliding Association (BGA)—Written evidence ................................................................... 49 British Standards Institution (BSI)—Written evidence .................................................................... 51 British Swimming and the Amateur Swimming Association—Written evidence ...................... 55 British Paralympic Association (BPA)—Written evidence ............................................................. 64 Community Safety Social Inclusion Scrutiny Commission—Written evidence ......................... 70 Dorset County Council—Written evidence .................................................................................... -

A Coach's Guide for 60X30 Softball
‘The Big Alley’ A Coach’s Guide for 60x30 Softball ‘THE BIG ALLEY’ 60X30 SOFTBALL INTRODUCTION 60x30 Softball is one of the four codes of the game (60x30 Softball, 60x30 Hardball, 40x20, One-Wall) governed by GAA Handball. The 60x30, or ‘Big Alley’ as it is commonly and strategies to improve your big alley referred to, is considered by many to be game. the traditional form of the game, and got its name from the dimensions of the • The ball is larger and made of softer court (60ft x 30ft). The term ‘Big Alley’ rubber. then attached itself to the code after the • The game is very cardio based due to introduction of the 40x20 court, or the the size of the court, and thus requires ‘Small Alley,’ to Ireland in 1969. a different type of fitness to the 40x20 code for example. The 60x30 court hosts two codes of • It is less demanding on the lower back Handball; (i) Softball – which will be and hips when compared to the 40x20 the primary focus of this document, court. This is due to less bending/low and (ii) Hardball. Whilst requiring a retrievals. similar generic Handballing skill set as • The floor is concrete, which can be other codes, there are still various key punishing on the joints, thus a good pair differences unique to 60x30 Softball. of court shoes with cushioned soles is This document will highlight various tips advised to protect the knees. 2 • GAAHandball.ie • ‘The Big Alley’ ‘THE BIG ALLEY’ 60X30 SOFTBALL TACTICS 1 SERVES Every rally in Handball is initiated with a serve, and thus its importance is paramount. -

Handball Sport Rules
HANDBALL SPORT RULES Handball Sport Rules 1 VERSION: June 2016 © Special Olympics, Inc., 2016 All rights reserved HANDBALL SPORT RULES TABLE OF CONTENTS 1. INTRODUCTION .................................................................................................................................... 4 Terminology .............................................................................................................................. 4 Fair Play .................................................................................................................................... 4 2. GOVERNING RULES ............................................................................................................................... 4 3. OFFICIAL EVENTS .................................................................................................................................. 4 Individual Skills Competition ...................................................................................................... 4 Team Competition ..................................................................................................................... 4 5-A-Side Handball ...................................................................................................................... 4 Unified Sports® Team Competition ............................................................................................ 4 4. MARKING THE HANDBALL COURT ........................................................................................................ -
PE Handball Basics Study Guide
TEAM HANDBALL! ! STUDY GUIDE and WORKSHEET! !Team Handball combines elements of soccer, basketball, water polo, and hockey.! !The object of the game is to score by throwing the ball past a goalkeeper in the net.! A throw-off (like a kick-off in soccer) is used start games and to re-start play after each !goal. Another option we use in PE is to do a jump ball at center court.! The 6 meter line marks the goal area where only the goalie is allowed. All shots must be !made beyond this line.! Regulation rules state that 7 players from each team are allowed to be on the court at the same time! ! A throw-in is awarded when a ball goes out of bounds on the sidelines.! !A goal-throw is awarded if a ball goes beyond the goal line.! !Passive play is illegal. You must make a visible effort to score. No stalling! When an offensive player is fouled while shooting, a penalty shot (7 meter throw) is !typically awarded. ! !Players are not allowed to endanger others. No pushing, holding, tripping, or hitting ! A red card may result from a major violation and a yellow card for less severe rule !violations.! Minor fouls result in a free throw in which the pass or shot must be made within 3 !seconds! !Players can only hold the ball without moving for 3 seconds! !Players can dribble the ball 3 times! !Players can take up to 3 steps before or after dribbles! !Players can play the ball behind the net or the goal area ! !Players are not allowed to make contact with the ball below the knees (no kicking)! !Players are not allowed to pull, hit, or punch the ball out of an opponent’s hands! Substitutes may enter the game at any time, similar to ice hockey, once the player they are replacing has left the court! . -

Bedienungsanleitung Bedienpulte
Multisport Serie 452 BEDIENUNGSANLEITUNG BEDIENPULTE Modelle mit programmierbaren Mannschaftsnamen Modelle mit oder ohne individuellen Fouls Zeichnungen und Bilder unverbindlich ZI de Bel Air 44850 LE CELLIER FRANKREICH [email protected] Tél. +33 (0)2 40 25 46 90 UD452MXX1XX_A - Bedienpult 452M Alpha.docx Seite 1 INHALT Seiten 3-5 Allgemeines 3 Lieferumfang 3 Datenspeicherung 3 Aufladung des Bedienpultes (funkgesteuertes Modell) 4 Tastenfunktionen des Hauptbedienpultes 5 Tastenfunktionen des separaten Timer-Pultes Seiten 6-7 Inbetriebnahme - Programmierung 6 Inbetriebnahme 6 Auswahl einer Sportart oder einer Funktion 6 Programmierung der Parametern für eine Sportart 7 Programmierung der Mannschaftsnamen Seiten 8-9 Diverse Konfiguration 8 Zugang zum Menü « allgemeine Konfiguration » 8 Sprachauswahl des Bedienpultes 8 PC Tastatur-Typ 8 Ausschaltungs- und Anzeigezeit der Uhrzeit auf der Anzeigetafel 8 Steuerungsmodus des Bedienpultes (funkgesteuerte Standard-Modelle) Basketball – Auslösen der leuchtender Umfassung auf dem Basketballkorb am Ende der 9 Angriffszeiten (24 s) 9 Basketball – fixe oder blinkende Anzeige der Light Strip (Ledstrip) 9 Rücksetzung sämtlicher Parameter des Bedienpultes 9 Spielregeländerungen (USB Stick) Seiten 9-41 Sportarten und Funktionen 9 Uhrzeit der Anzeigetafel 10-11 Basketball 12-13 Handball 14-15 Volleyball 16-17 Tennis 18-19 Tischtennis 20-21 Badminton 22-23 Roller-Hockey 24-25 Inline -Hockey 26-27 Eishockey 28-29 Unihockey / Floorball 30-31 Hallenfussball 32-33 Netball 34-35 Boxen 36 Timer 37 Training 38-39 Freimodus (Selbstprogrammierbarer Modus) – Modus "Perioden" 40-41 Freimodus (Selbstprogrammierbarer Modus) – Modus "Sätze" ZI de Bel Air 44850 LE CELLIER FRANKREICH [email protected] Tél. +33 (0)2 40 25 46 90 UD452MXX1XX_A - Bedienpult 452M Alpha.docx Seite 2 ALLGEMEINES Lieferumfang Hauptbedienpult Dient zur Steuerung der Hauptfunktionen und der verschiedenen Funktionsabläufe (Timer, Spielstand, usw…). -

Summary of Main Law Changes 2019/20
Laws of the Game 2019/20 At a Glance: Summary of the main changes The International Football Association Board March 2019 Introduction The 133rd AGM of The International FA Board (The IFAB) in Aberdeen, Scotland on 2 March 2019 approved a number of amendments to, and clarifications of, the Laws of the Game for 2019/20. Three changes were approved following 2 years of worldwide experiments: • The introduction of yellow and red cards for misconduct by team officials • A player being substituted leaving the field at the nearest point on the boundary line • At a goal kick and a free kick for the defending team in their own penalty area, the ball is in play as soon the kick is taken (it can be played before it leaves the penalty area) Other changes include: clearer wording for ‘handball’, attacking team players must be at least 1m away from a defensive ‘wall’, the goalkeeper only has to have one foot on the goal line at a penalty kick, and a new dropped ball procedure (including a dropped ball being awarded if the ball hits a match official and goes into the goal, team possession changes or a promising attack starts). This document summarises the main changes only – a more detailed version with the exact text of all the changes may be found in the document ‘Laws of the Game 2019-20 – Changes and clarifications’; both documents are available on The IFAB’s website (www.theifab.com ). Downloadable versions of the Laws of the Game 2019/20 in English, French, German and Spanish will be available in mid/late May on The IFAB’s website, along with details of the new IFAB Laws of the Game app.