In Vitro Fertilization | GLOWM
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Sample-11060.Pdf
Ob/Gyn Sonography An Illustrated Review 2nd Edition Jim Baun, BS, RDMS, RVT, FSDMS Professional Ultrasound Services San Francisco, California SPECIALISTS IN ULTRASOUND EDUCATION, TEST PREPARATION, AND CONTINUING MEDICAL EDUCATION iv SPECIALISTSCopyright IN ULTRASOUND © 2016, EDUCATION, 2004 by Davies Publishing, Inc. TEST PREPARATION, AND CONTINUINGAll rights MEDICAL reserved. EDUCATION No part of this work may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic or mechanical, including photocopying, scanning, and recording, without prior written permission from the publisher. Davies Publishing, Inc. Michael Davies, Publisher Specialists in Ultrasound Education, Christina J. Moose, Editorial Director Test Preparation, and Continuing Charlene Locke, Production Manager Medical Education Janet Heard, Operations Manager 32 South Raymond Avenue Pasadena, California 91105-1961 Jim Baun, Illustration Phone 626-792-3046 Stephen Beebe, Illustration Facsimile 626-792-5308 Satori Design Group, Inc., Design Email [email protected] www.daviespublishing.com Notice to Users of This Publication: In the field of ultrasonography, knowledge, technique, and best practices are continually evolving. With new research and developing technologies, changes in methodologies, professional prac- tices, and medical treatment may become necessary. Sonography practitioners and other medi- cal professionals and researchers must rely on their experience and knowledge when evaluating and using information, methods, -

27Th ANNUAL RESEARCH DAY & Henderson Lecture
27th ANNUAL RESEARCH DAY & Henderson Lecture FRIDAY, MAY 7, 2010 8:00 a.m. to 6:30 p.m. Northrop Frye Hall, Ground Floor Victoria University, 73 Queen's Park Crescent East University of Toronto M5S 1K7 Lecturer: Jane Norman MD Professor of Maternal and Fetal Health, University of Edinburgh, UK Co-Director, Edinburgh Tommy’s Centre for Maternal and Fetal Health Research Topic: Being Born Too Soon – Do Obstetricians Have Anything To Offer? Abstract deadline: Friday, March 5, 2010 http://www.obgyn.utoronto.ca/Research/ResearchDay.htm For additional information or assistance, please contact Helen Robson at [email protected] PROGRAMME-AT-A-GLANCE (A.M.) Department of Obstetrics & Gynaecology 27th Annual Research Day, Friday, May 7, 2010 Northrop Frye Hall, Victoria University, University of Toronto, 73 Queen’s Park Crescent NF=Northrop Frye Hall Burwash Hall is located at the north end of the Victoria Quad 7:30 a.m. on Poster Set-up for Poster Session I [NF, ground floor, Rms. 004, 006, 007 & 008] 8:00 a.m. Registration & Continental Breakfast [NF, ground floor lobby] 8:25 – 8:30 a.m. Welcome: Dr. Alan Bocking, Chair [NF, ground floor Lecture Hall, Rm. 003] 8:30 – 9:45 a.m. Oral Session I (O1-O5) [NF, ground floor Lecture Hall, Rm. 003] 9:45 – 10:05 a.m. Coffee Break & Poster Session I Walkabout [NF, ground floor lobby; Rms. 004, 006, 007 & 008] 10:05 – 11:05 a.m. Poster Session I Tour [NF, Rms. 004, 006, 007 & 008] Groups A-F Poster Takedown for a.m. -

Annualreport 2010
AnnualReport 2010 Seth G.S. Medical College & King Edward Memorial Hospital Municipal Corporation of Greater Mumbai Convocation Ceremony of Use of smart board by 1st MBBS students Fellowship and Certificate Courses Automated chappati maker Clean KEM campaign Cardiac Ambulance Seth G.S. Medical College & King Edward Memorial Hospital Municipal Corporation of Greater Mumbai ANNUAL REPORT 2010 Concept (Front & Back cover) Dr. Sanjay Oak Director -Medical Education and Major Hospitals Professor of Pediatric Surgery Publisher Diamond Jubilee Society Trust Seth G.S. Medical College & KEM Hospital, Parel, Mumbai 400 012. Printer Urvi Compugraphics A2/248, Shah & Nahar Industrial Estate, S.J. Marg, Lower Parel (West), Mumbai 400 013. Tel.: 91 - 22 - 2494 5863 © Seth GS Medical College & KEM Hospital, 2011 Acknowledgements Smt. Shraddha Jadhav Hon. Mayor Smt. Shailaja Girkar Shri Subodh Kumar Deputy Mayor Municipal Commissioner Shri Sunil Prabhu Smt. Manisha Patankar-Mhaiskar Leader of the House Additional Municipal Commissioner (Western Suburbs) Shri Rajhans Singh Shri Aseem Gupta Leader of the Opposition Additional Municipal Commissioner (Eastern Suburbs) Shri Rahul Shewale Shri Mohan Adtani Chairman-Standing Committee Additional Municipal Commissioner (City) Smt. Ashwini Mate Shri Rajeev Jalota Chairman-Public Health Committee Additional Municipal Commissioner (Projects) Shri Parshuram (Chotu) Desai Shri Rajendra Vale Chairman-Works Committee (City) Deputy Municipal Commissioner (Estate & General Administration) Shri Anil Pawar Shri Sanjay (Nana) Ambole Chairperson - Ward Committee Municipal Councillor From the Director’s desk..... The twin institutes of the Seth GS Medical College & KEM Hospital were established in 1926 with a nationalistic spirit to cater to the “health care needs of the northern parts of the island” to be manned entirely by Indians. -

The Relationship Between H19 and Parameters of Ovarian Reserve Xi Xia1,2, Martina S
Xia et al. Reproductive Biology and Endocrinology (2020) 18:46 https://doi.org/10.1186/s12958-020-00578-z RESEARCH Open Access The relationship between H19 and parameters of ovarian reserve Xi Xia1,2, Martina S. Burn2, Yong Chen3,2, Cengiz Karakaya4 and Amanda Kallen2* Abstract Context: The H19 long noncoding RNA (lncRNA) belongs to a highly conserved, imprinted gene cluster involved in embryonic development and growth control. We previously described a novel mechanism whereby the Anti- mullerian hormone (Amh) appears to be regulated by H19. However, the relationship between circulating H19 and markers of ovarian reserve including AMH not been investigated. Objective: To determine whether H19 expression is altered in women with decreased ovarian reserve. Design: Experimental study. Setting: Yale School of Medicine (New Haven, USA) and Gazi University School of Medicine (Ankara, Turkey). Patients or other participants: A total of 141 women undergoing infertility evaluation and treatment. Intervention: Collection of discarded blood samples and cumulus cells at the time of baseline infertility evaluation and transvaginal oocyte retrieval, respectively. Main outcome measure: Serum and cumulus cell H19 expression. Results: Women with diminished ovarian reserve (as determined by AMH) had significantly lower serum H19 expression levels as compared to controls (p < 0.01). Serum H19 was moderately positively correlated with serum AMH. H19 expression was increased 3.7-fold in cumulus cells of IVF patients who demonstrated a high response to gonadotropins, compared to low responders (p < 0.05). Conclusion: In this study, we show that downregulation of H19 in serum and cumulus cells is closely associated with decreased ovarian reserve, as measured by decreased AMH levels and reduced oocyte yield at oocyte retrieval. -

Herbal Medicines in Pregnancy and Lactation : an Evidence-Based
00 Prelims 1410 10/25/05 2:13 PM Page i Herbal Medicines in Pregnancy and Lactation An Evidence-Based Approach Edward Mills DPh MSc (Oxon) Director, Division of Clinical Epidemiology Canadian College of Naturopathic Medicine North York, Ontario, Canada Jean-Jacques Duguoa MSc (cand.) ND Naturopathic Doctor Toronto Western Hospital Assistant Professor Division of Clinical Epidemiology Canadian College of Naturopathic Medicine North York, Ontario, Canada Dan Perri BScPharm MD MSc Clinical Pharmacology Fellow University of Toronto Toronto, Ontario, Canada Gideon Koren MD FACMT FRCP Director of Motherisk Professor of Medicine, Pediatrics and Pharmacology University of Toronto Toronto, Ontario, Canada With a contribution from Paul Richard Saunders PhD ND DHANP 00 Prelims 1410 10/25/05 2:13 PM Page ii © 2006 Taylor & Francis Medical, an imprint of the Taylor & Francis Group First published in the United Kingdom in 2006 by Taylor & Francis Medical, an imprint of the Taylor & Francis Group, 2 Park Square, Milton Park, Abingdon, Oxon OX14 4RN Tel.: ϩ44 (0)20 7017 6000 Fax.: ϩ44 (0)20 7017 6699 E-mail: [email protected] Website: www.tandf.co.uk/medicine All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or trans- mitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of the publisher or in accordance with the provisions of the Copyright, Designs and Patents Act 1988 or under the terms of any licence permitting limited copying issued by the Copyright Licensing Agency, 90 Tottenham Court Road, London W1P 0LP. -

Journal of Threatened Taxa
PLATINUM The Journal of Threatened Taxa (JoTT) is dedicated to building evidence for conservaton globally by publishing peer-reviewed artcles OPEN ACCESS online every month at a reasonably rapid rate at www.threatenedtaxa.org. All artcles published in JoTT are registered under Creatve Commons Atributon 4.0 Internatonal License unless otherwise mentoned. JoTT allows unrestricted use, reproducton, and distributon of artcles in any medium by providing adequate credit to the author(s) and the source of publicaton. Journal of Threatened Taxa Building evidence for conservaton globally www.threatenedtaxa.org ISSN 0974-7907 (Online) | ISSN 0974-7893 (Print) Review Ramifications of reproductive diseases on the recovery of the Sumatran Rhinoceros Dicerorhinus sumatrensis (Mammalia: Perissodactyla: Rhinocerotidae) Nan E. Schafer, Muhammad Agil & Zainal Z. Zainuddin 26 February 2020 | Vol. 12 | No. 3 | Pages: 15279–15288 DOI: 10.11609/jot.5390.12.3.15279-15288 For Focus, Scope, Aims, Policies, and Guidelines visit htps://threatenedtaxa.org/index.php/JoTT/about/editorialPolicies#custom-0 For Artcle Submission Guidelines, visit htps://threatenedtaxa.org/index.php/JoTT/about/submissions#onlineSubmissions For Policies against Scientfc Misconduct, visit htps://threatenedtaxa.org/index.php/JoTT/about/editorialPolicies#custom-2 For reprints, contact <[email protected]> The opinions expressed by the authors do not refect the views of the Journal of Threatened Taxa, Wildlife Informaton Liaison Development Society, Zoo Outreach Organizaton, or any of -

Sperm Aneuploidy and DNA Fragmentation in Unexplained
Esquerré-Lamare et al. Basic and Clinical Andrology (2018) 28:4 https://doi.org/10.1186/s12610-018-0070-6 RESEARCH ARTICLE Open Access Sperm aneuploidy and DNA fragmentation in unexplained recurrent pregnancy loss: a multicenter case-control study Camille Esquerré-Lamare1,2, Marie Walschaerts1,2, Lucie Chansel Debordeaux3, Jessika Moreau1,2, Florence Bretelle4, François Isus1,5, Gilles Karsenty6, Laetitia Monteil7, Jeanne Perrin8,9, Aline Papaxanthos-Roche3 and Louis Bujan1,2* Abstract Background: Recurrent pregnancy loss (RPL) is defined as the loss of at least three pregnancies in the first trimester. Although the most common cause is embryo aneuploidy, and despite female checkup and couple karyotyping, in about 50% of cases RPL remain unexplained. Male implication has little been investigated and results are discordant. In this context, we conducted a multi-center prospective case-control study to investigate male gamete implication in unexplained RPL. Methods: A total of 33 cases and 27 controls were included from three university hospitals. We investigated environmental and family factors with a detailed questionnaire and andrological examination, sperm characteristics, sperm DNA/chromatin status using the sperm chromatin structure assay (SCSA) and terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) and sperm aneuploidy using fluorescence in situ hybridization (FISH). The Mann-Whitney test and the Wilcoxon or Fisher exact tests were used. A non-parametric Spearman correlation was performed in order to analyze the relationship between various sperm parameters and FISH and sperm DNA fragmentation results. Results: We found significant differences between cases and controls in time to conceive, body mass index (BMI), family history of infertility and living environment. -

Endometriosis, Ovarian Reserve and Live Birth Rate Following in Vitro
THIEME 218 Original Article Endometriosis, Ovarian Reserve and Live Birth Rate Following In Vitro Fertilization/ Intracytoplasmic Sperm Injection Endometriose, reserva ovariana e taxa de nascidos vivos após FIV/ICSI Marcela Alencar Coelho Neto1 Wellington de Paula Martins1 Caroline Mantovani da Luz1 Bruna Talita Gazeto Melo Jianini1 Rui Alberto Ferriani1 Paula Andrea Navarro1 1 Department of Obstetrics and Gynecology, Faculdade de Medicina Address for correspondence Paula Andrea Navarro, MD, PhD, de Ribeirão Preto, Universidade de São Paulo – USP, Ribeirão Preto, Departmento de Ginecologia e Obstetrícia, Faculdade de Medicina de SP, Brasil Ribeirão Preto, Hospital das Clínicas de Ribeirão Preto, Centro de Reprodução Humana, Universidade de São Paulo, Avenida Rev Bras Ginecol Obstet 2016;38:218–224. Bandeirantes, 3.900, 8o andar, Ribeirão Preto, caixa postal: 14048- 900, Ribeirão Preto, SP, Brazil (e-mail: [email protected]). Abstract Purpose To evaluate whether women with endometriosis have different ovarian reserves and reproductive outcomes when compared with women without this diagnosis undergoing in vitro fertilization/intracytoplasmic sperm injection (IVF/ ICSI), and to compare the reproductive outcomes between women with and without the diagnosis considering the ovarian reserve assessed by antral follicle count (AFC). Methods This retrospective cohort study evaluated all women who underwent IVF/ ICSI in a university hospital in Brazil between January 2011 and December 2012. All patients were followed up until a negative pregnancy test or until the end of the pregnancy. The primary outcomes assessed were number of retrieved oocytes and live birth. Women were divided into two groups according to the diagnosis of endometri- osis, and each group was divided again into a group that had AFC 6 (poor ovarian reserve) and another that had AFC 7 (normal ovarian reserve). -

Unexplained Infertility
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Helsingin yliopiston digitaalinen arkisto Department of Obstetrics and Gynaecology, Helsinki University Central Hospital, University of Helsinki, Finland UNEXPLAINED INFERTILITY Studies on aetiology, treatment options and obstetric outcome RITA ISAKSSON ACADEMIC DISSERTATION To be presented by permission of the Medical Faculty of the University of Helsinki for public criticism in the Auditorium of the Department of Obstetrics and Gynaecology, Helsinki University Central Hospital, Haartmaninkatu 2, Helsinki, on October 18th, 2002, at 12 noon. Helsinki 2002 1 Supervised by Docent Aila Tiitinen, M.D., Ph.D. Department of Obstetrics and Gynaecology Helsinki University Central Hospital Docent Bruno Cacciatore, M.D., Ph.D. Department of Obstetrics and Gynaecology Helsinki University Central Hospital Reviewed by Docent Anne-Maria Suikkari, M.D., Ph.D. The Family Federation of Finland, Infertility Clinic, Helsinki Docent Aydin Tekay, M.D., Ph.D. Department of Obstetrics and Gynaecology Oulu University Central Hospital Offi cial opponent Docent Hannu Martikainen, M.D., Ph.D. Department of Obstetrics and Gynaecology Oulu University Central Hospital ISBN 952-91-5071-7 (print) ISBN 952-10-0712-5 (PDF) Yliopistopaino Helsinki 2002 2 To my family 3 CONTENTS LIST OF ORIGINAL PUBLICATIONS ....................................................................7 ABBREVIATIONS ................................................................................................. -

International Publications (2009)
INTERNATIONAL PUBLICATIONS Faculty of Medicine, Cairo University (2009) Edited by: Professor Dr. Lamis Ragab Professor Dr. Taymour Mostafa Professor Dr. Hesham El Anany Professor Dr. Rania Mohamed Printed by MEDC INDEX 1 Pubmed Index Publications …………………………. 1-157 2 Other Cited Publications ……………………………. 158-163 3 a. Oral Presentations at International Conferences … 164-169 b. Poster Presentations at International Conferences . 170-173 c. Abstracts in International Conferences ………….. 174-176 An important part of the mission of Kasr Al Aini Faculty of Medicine, Cairo University is training a professional, specialized graduate able to conduct research and apply national and international standards of medical care. The institution should prove that academic research activities make a full contribution to the achievement of the mission. The quality and quantity of research activities should be documented. This is the third document of the published research of the faculty in international journals. The number of staff involved in peer reviewed published research is 415. We aim to increase this record by encouraging staff, especially the young generations, to publish their research in international journals with a high impact factor. The quality and quantity of research activities is an important factor in accrediting academic instutitions and ranking of universities. Dean of the Faculty Vice Dean for Postgraduate Studies & Research Prof. Dr. Ahmed Sameh Farid Prof. Dr. Lamis Ragab International Publications Acta Anaesthesiol Scand. 2009 Feb;53(2):251-6. Impact Factor: 1.953 Effect of dexmedetomidine on the characteristics of bupivacaine in a caudal block in pediatrics. Saadawy I, Boker A, Elshahawy MA, Almazrooa A, Melibary S, Abdellatif AA, Afifi W. -

Accepted Manuscript
ACCEPTED MANUSCRIPT Prenatal inflammation exposure-programmed cardiovascular diseases and potential prevention Youcai Denga,b,1,*, Liang Songa,b,1, Xuqiang Niea,b, Weinian Shoua,b,c, Xiaohui Lia,b,* aInstitute of Materia Medica, College of Pharmacy, Army Medical University (Third Military Medical University), 30# Gaotanyan Rd., Shapingba District, Chongqing 400038, China bCenter of Translational Medicine, College of Pharmacy, Army Medical University (Third Military Medical University), 30# Gaotanyan Rd., Shapingba District, Chongqing 400038, China cHerman B Wells Center for Pediatric Research, Department of Pediatrics, Indiana University School of Medicine, 1044 W. Walnut Street, R4 W302D, Indianapolis, IN 46202, USA 1These authors equally contributed to this work. *Address correspondence to: Xiaohui Li and Youcai Deng Address: Room 606, Pharmaceutical Sciences Building, 30# Gaotanyan Rd, Shapingba District, Chongqing 400038, China Tel.: (86) 23-68771632;ACCEPTED MANUSCRIPT Fax: (86)23-68753397 Email address: [email protected] (Y. Deng); [email protected] (X. Li) ___________________________________________________________________ This is the author's manuscript of the article published in final edited form as: Deng, Y., Song, L., Nie, X., Shou, W., & Li, X. (n.d.). Prenatal inflammation exposure-programmed cardiovascular diseases and potential prevention. Pharmacology & Therapeutics. https://doi.org/10.1016/j.pharmthera.2018.05.009 ACCEPTED MANUSCRIPT Abstract In recent years, the rapid development of medical and pharmacological interventions has led to a steady decline in certain noncommunicable chronic diseases (NCDs), such as cancer. However, the overall incidence of cardiovascular diseases (CVDs) has not seemed to decline. CVDs have become even more prevalent in many countries and represent a global health threat and financial burden. -
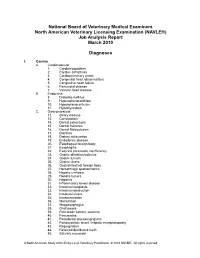
Job Analysis Final Report for Web2
National Board of Veterinary Medical Examiners North American Veterinary Licensing Examination (NAVLE®) Job Analysis Report March 2010 Diagnoses I. Canine A. Cardiovascular 1. Cardiomyopathies 2. Cardiac arrhythmia 3. Cardiopulmonary arrest 4. Congenital heart abnormalities 5. Congestive heart failure 6. Pericardial disease 7. Valvular heart disease B. Endocrine 8. Diabetes mellitus 9. Hyperadrenocorticism 10. Hypoadrenocorticism 11. Hypothyroidism C. Gastrointestinal 12. Biliary disease 13. Constipation 14. Dental extractions 15. Dental fractures 16. Dental Malocclusion 17. Diarrhea 18. Dietary indiscretion 19. Endodontic disease 20. Esophageal foreign body 21. Esophagitis 22. Exocrine pancreatic insufficiency 23. Gastric dilatation/volvulus 24. Gastric tumors 25. Gastric ulcers 26. Gastrointestinal foreign body 27. Hemorrhagic gastroenteritis 28. Hepatic cirrhosis 29. Hepatic tumors 30. Hepatitis 31. Inflammatory bowel disease 32. Intestinal neoplasia 33. Intestinal obstruction 34. Intestinal ulcers 35. Intussusception 36. Malnutrition 37. Megaesophagus 38. Oral tumors 39. Pancreatic tumors, exocrine 40. Pancreatitis 41. Periodontal disease/gingivitis 42. Portosystemic shunt / hepatic encephalopathy 43. Regurgitation 44. Retained deciduous teeth 45. Salivary mucocele A North American Study of the Entry-Level Veterinary Practitioner © 2010 NBVME. All rights reserved. D. Hemic/Lymphatic 46. Anemia (general) 47. Immune mediated hemolytic anemia 48. Immune mediated thrombocytopenia 49. Canine juvenile cellulitis 50. Coagulopathy 51. Hemangiosarcoma 52. Immunodeficiency 53. Lymphadenopathy 54. Lymphosarcoma / leukemia 55. Mast cell tumor 56. Systemic lupus erythematosus 57. Transfusion therapy E. Integumentary 58. Abscesses 59. Acral lick granuloma 60. Allergic dermatitis 61. Alopecia 62. Anal sac disease 63. Aural hematoma 64. Bite wounds 65. Burns 66. Decubitus ulcers 67. Dermatophytosis 68. Diseases of claws 69. Diseases of pads 70. Otitis externa/media 71.